The University of Pittsburgh Medical Center (UPMC) is a world-renowned healthcare provider and insurer with groundbreaking work in research, treatments, and clinical care. UPMC runs 40 hospitals and more than 700 doctors’ offices and outpatient centers, serving patients throughout western and central Pennsylvania, Maryland, New York, and around the globe.
Established in 2000 under the guidance of Michael “Micky” Collins, the UPMC Sports Medicine Concussion Program sees over 20,000 concussed patients every year. Most of the patients treated at UPMC — including professional, collegiate, high school, and youth athletes — suffered a sports-related concussion. The program also treats patients with non-sports-related concussions, as well as those with other neurological and psychiatric brain disorders.
In addition to treating patients, UPMC’s concussion program also has a robust research component. This program has become well-known over the past few years because the NFL has awarded UPMC multiple funding grants to study the impact of concussions on their players. For example, the latest clinical trial, still ongoing, aims to assess the long-term impact of concussions on brain health.
UPMC specializes in treating patients shortly after their concussion, but, as we’ll explain later in the article, their approach is not ideal for patients with persistent symptoms after a head injury. Some patients experience symptoms for months or years after their concussion; experiencing these ongoing symptoms is known as post-concussion syndrome (PCS). These patients have much lower recovery rates when using the same approach as patients with recent concussions because their needs are no longer the same as acute concussion patients’.
At Cognitive FX, we specialize in treating this complex group of PCS patients. Our clinic brings together clinicians from over a dozen specialties to collaboratively provide evidence-based, multidisciplinary treatment tailored to the unique brain injury of each person who visits our clinic. This treatment program is designed to address the root causes of the symptoms directly, rather than tackling individual symptoms one at a time. This personalized, holistic approach leads to our unprecedented 90 percent treatment success rate.
Take our former patient Sam Pembleton, for example. Several months after suffering a soccer concussion, she experienced debilitating symptoms, including headaches, fatigue, and sensitivity to light.

Sam (in red) playing the sport she loved.
Eventually, after Sam visited many well-known concussion clinics without success, Sam’s mother found Cognitive FX. During therapy, Sam recognized some of the exercises and techniques used at other clinics she had visited, though there were many she had never done before.
“The biggest difference was, at Cognitive FX, they were doing a bunch of different treatments at the same time, working different parts of your brain all at once,” she explained.
In addition, Sam’s treatment plan was designed based on the results of her fNCI brain scan. (An fNCI looks at blood flow patterns in the brain to determine how and where the brain was affected by the concussion.)
“I think the most difficult thing for people to grasp is the fact that unlike a broken bone or something, a concussion is so different for everyone. Each person’s brain is so different that one treatment may work for one person, whereas someone else may need a completely different approach,” she said. “A concussion is like a fingerprint. It's unique for each person.”
Understanding which clinic — UPMC or Cognitive FX — is right for you depends largely on understanding the difference between recent concussion and post-concussion syndrome.
In this article, we’ll explain why each condition needs a different treatment approach and explore the differences between what we offer at Cognitive FX versus what is offered at UPMC, in terms of:
90% of our patients report significant symptom reduction after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.
What Happens to the Brain After a Concussion (and Why Acute and Chronic Concussions Can’t Be Treated the Same Way)

The brain’s first reaction to a concussion is to trigger a localized inflammatory response in the affected area. This happens within 24 hours of the injury and is a crucial part of the brain’s recovery mechanisms, involving a series of chemicals released in the brain to aid the injured tissue.
Concussions and the resulting inflammation affect blood flow in the brain and cause changes in the way brain cells communicate with surrounding blood vessels to receive the resources they need to function. In a healthy brain, brain cells and blood vessels share a highly dynamic connection, one which allows brain cells to request the oxygen and nutrients they need to perform a particular task and have them delivered to the right location at the right time in the right amount. This is called neurovascular coupling (NVC).
Concussions disrupt this link; consequently, cells either receive the wrong amount (too little or too much) or get it at the wrong time. When this happens, cells are no longer able to complete the tasks assigned to them. Your brain will try to complete the task using an alternative pathway, but this pathway will inevitably be less efficient, causing you to tire out more quickly. This NVC dysfunction causes a variety of symptoms, such as headaches, brain fog, and fatigue.
The brain has an incredible ability to recover, however, and can use brain cells that remain healthy after the injury. The brain can fix the neural pathways disrupted by the concussion or form new ones to regain lost functions. This mechanism is called neuroplasticity. In patients who recover within a few days after their concussion, this is a straightforward process. At this stage, neurovascular coupling disruption is easily reversible by itself or with some simple therapy (cardiovascular exercise, physical therapy, vision therapy, and/or vestibular therapy as needed) to “nudge” neuroplasticity in the right direction.
Unfortunately, for some patients, not all symptoms resolve within this period. At least 15 percent of patients experience persistent symptoms that last months or even years, but that number can be as high as 60 percent depending on geographical location, injury severity, quality of care, and so forth. These patients suffer from a condition called post-concussion syndrome (PCS).
In these patients, the brain keeps using less efficient pathways to complete tasks even after inflammation has resolved. Once neurovascular coupling disruption becomes more established, it’s more challenging to treat. Standard therapies used to treat concussed patients are often not enough to treat PCS patients. Instead, PCS patients benefit from a customized, multidisciplinary therapeutic approach to restore healthier neurovascular signaling pathways.
In PCS patients, treatment is further complicated because brain injuries can also lead to chronic symptoms stemming from a combination of secondary conditions, including autonomic nervous system dysfunction, vision and vestibular problems, hormone imbalance, and breathing problems.
For example, the autonomic nervous system (ANS) — which controls many bodily functions, including heart rate, blood pressure, digestion speed, and body temperature — often becomes dysfunctional after a concussion.
Under normal circumstances, the ANS’ main branches, the sympathetic nervous system (SNS, which controls the fight-or-flight reaction) and the parasympathetic nervous system (PNS, which controls the rest-and-digest response), work together in harmony. However, in TBI patients, the SNS can become dominant even when there’s no need to react to a stressful situation. As a result, patients experience symptoms such as irregular breathing, high or low blood pressure, neck pain, headaches, digestive issues, dizziness, sensitivity to light, and more.
Further reading: Post-concussion ANS dysfunction (dysautonomia)
Vision problems are also common after a concussion and can prevail for a long period if not treated properly. PCS patients may experience a wide range of post-concussion vision problems, such as double vision, tired eyes, and problems with focusing and eye teaming (how the eyes work together). Vision therapy is often effective for patients who experience visual symptoms for longer than three months.
Some patients also experience changes in vestibular function. Mild traumatic brain injuries can disrupt the connection between the brain, vision, and vestibular system, which makes it harder for the brain to understand where it's positioned relative to surroundings. This leads to symptoms such as headache, dizziness or vertigo, balance problems, and spatial disorientation. Fortunately, post-concussion vestibular therapy is very effective for these issues.
Brain injuries can also damage the hypothalamus and pituitary glands and cause hormonal imbalance. These small structures are responsible for controlling hormone levels in the body. Structural or functional damage to these areas disrupts the production of many different hormones, causing multiple symptoms throughout the body, including low blood pressure, weight gain, low libido, amenorrhea, heart palpitations, hair loss, fatigue, mood swings, and headaches.
Further reading: Hormone dysfunction following head injury
Finally, concussions may affect breathing dynamics, disrupting the mechanisms that regulate the levels of carbon dioxide (CO2) and oxygen (O2) in the bloodstream. Breathing issues can cause patients to feel dizzy and lightheaded, have frequent headaches, or struggle with physical activity. Breathing exercises — an important part of the treatment we offer at Cognitive FX — go a long way to help accelerate the patient’s recovery.
As you can see, post-concussion syndrome is vastly more complex than acute concussion. This information is key to understanding which concussion treatments represent the best option for you.
Treatment plans for patients with a recent concussion typically involve cardiovascular exercise complimented by one or two standard therapies (physical, vision, and/or vestibular therapy) done over a few sessions. For most patients, this is usually enough to correct neurovascular dysfunction and eliminate symptoms.
In contrast, treatment for post-concussion syndrome is more challenging. Symptoms persisting longer than three months mean neurovascular disruption has become more established. In this case, patients need a more detailed evaluation process to find out exactly how and where the concussion affected their brain and which secondary conditions are present, followed by customized therapy sessions to address their specific situation.
With that in mind, we can now discuss key similarities and differences between the concussion treatment program at UPMC and at Cognitive FX.
UPMC Concussion Clinic vs. Cognitive FX: Patient Evaluation

The quality of a clinic’s assessment can have a huge impact on recovery outcomes. Properly assessing the cause of symptoms is needed to determine the appropriate therapy course.
UPMC
At UPMC, before patients start treatment for their concussion, they must undergo a detailed medical examination. UPMC’s standard concussion testing includes:
- A patient interview with a doctor to discuss medical history and symptoms present.
- Vestibular ocular motor screening (VOMS),which assesses the systems in charge of balance, vision, and movement. This test — originally developed by experts at UPMC — aims to identify the presence of vision and balance issues after a concussion.
- ImPACT (Immediate Post Concussion Assessment and Cognitive Testing), which looks at cognitive issues, such as verbal and visual memory, processing speed, and reaction time. This test alone cannot be used to offer a concussion diagnosis, but it is helpful if the patient takes it when healthy to establish a baseline before sustaining a concussion.
- Some patients may receive a CT or MRI scan if there is a risk of skull fractures or bleeding in the brain.
The team at UPMC then uses the results from these tests to create a concussion treatment and management plan for each patient. They follow an active treatment approach where patients are encouraged to do therapy and return to normal activities after a short period of rest (typically 48 hours) after the concussion.
Cognitive FX
At Cognitive FX, the initial part of the assessment patients must complete is somewhat similar to what’s done at UPMC. Our patients need to meet with one of our team members to review their medical history and concussion symptoms. Patients also undergo a series of tests, including:
- A physical exam to identify problems with balance, hand-eye coordination, reaction times, and other physical abilities. For example, patients use digital eye-tracking software to assess vision problems, such as difficulty tracking or poor peripheral vision.
- Neurocognitive testing to assess memory, concentration, reasoning, and other cognitive functions.
- A psychological evaluation to spot symptoms of anxiety, depression, and other mental health problems.
- Advanced neuroimaging to determine where and how your brain was affected by the concussion (more information below).
- A structural brain and cervical spine MRI to make sure patients do not have any serious structural injuries before they begin treatment.
The first three exams (physical, cognitive, psychological) are comprehensive and help our therapists tailor their routines to your ability levels. But patient evaluations don’t end here at Cognitive FX. We go one step further than UPMC to find exactly how the concussion affected the patient’s brain using state-of-the-art brain imaging technology called functional Neurocognitive Imaging (fNCI).
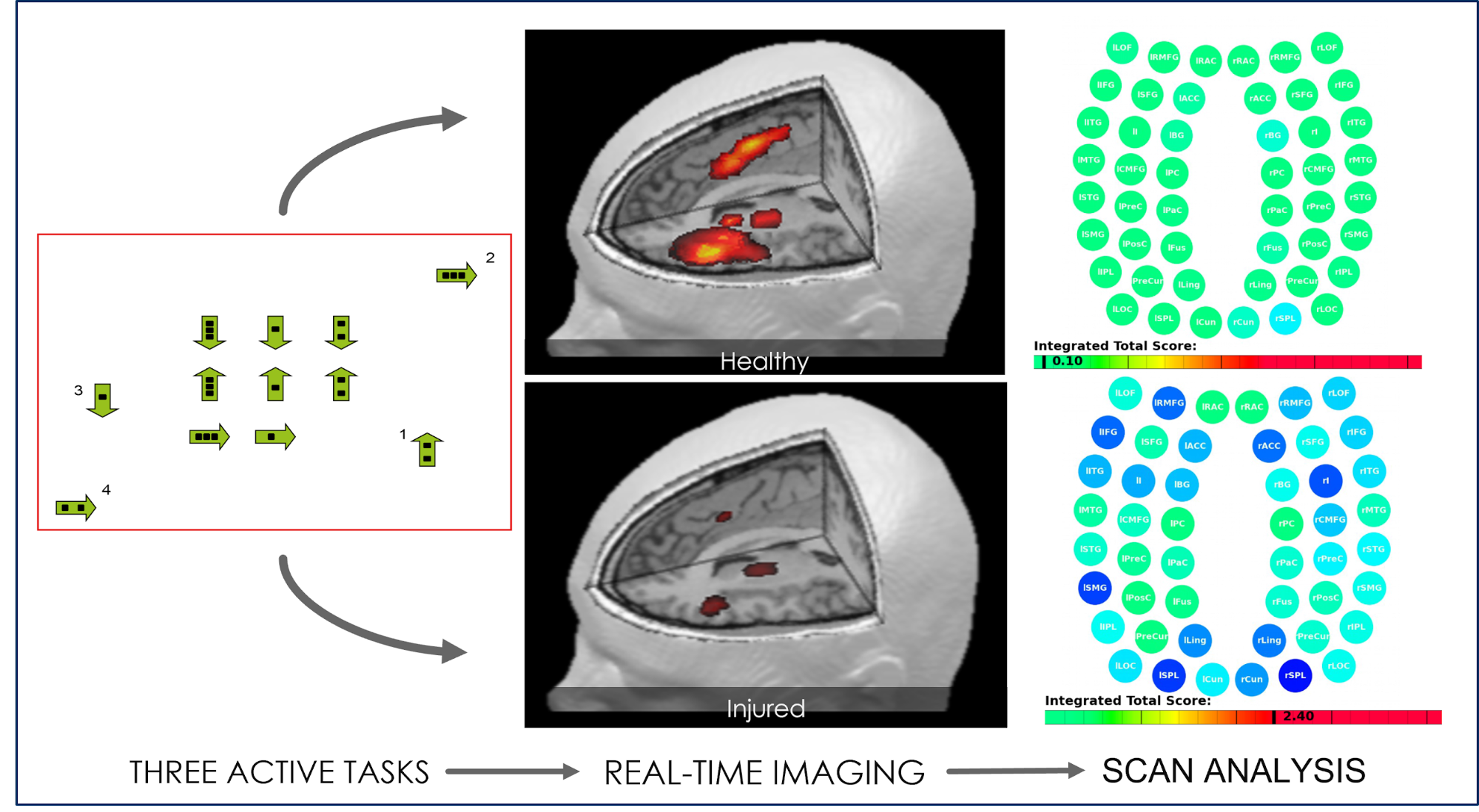
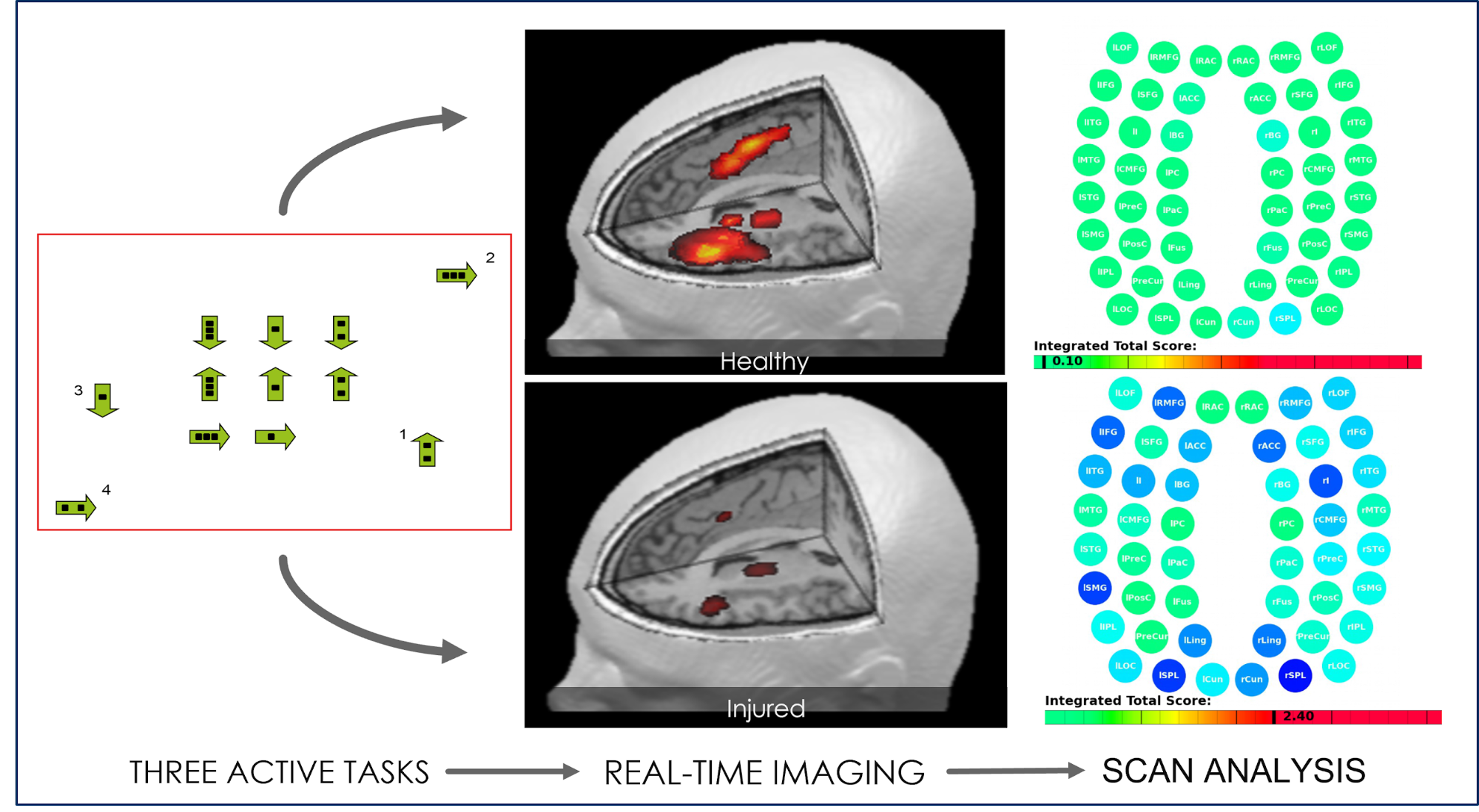
The scan, a special method of functional magnetic resonance imaging (fMRI), measures blood flow in 100 different regions of the brain while patients carry out a set of standardized cognitive tasks. The resultant real-time images are combined and compared with scans from healthy people to identify the areas where NVC dysfunction is disrupting normal brain function.
Regions are grouped based on function — and then scored. Green scores indicate normal function, while yellow and red scores indicate sections with neurovascular coupling dysfunction.

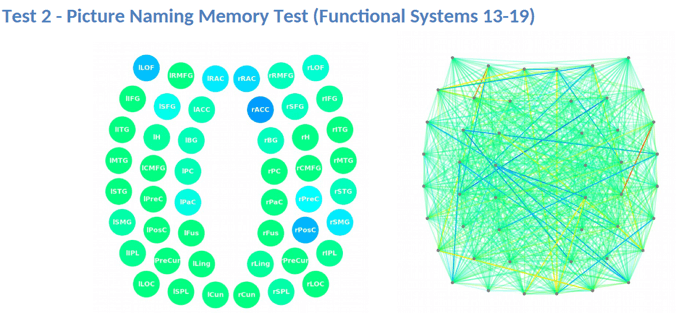
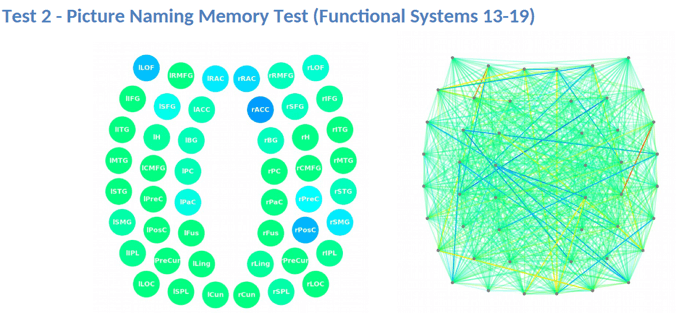
The scan also measures how these regions in the brain communicate with each other. Regions in green are normal, while regions in varying shades of blue are less active than normal. For example, in the image below, rACC (the right anterior cingulate cortex) is underperforming and most likely contributing to the patient’s attention and memory problems.
Once all medical exams and brain scans are completed, our team can design a customized treatment plan to target exactly the areas of the brain that show dysfunction.
Key Takeaways
In our view, UPMC provides a sound initial medical examination for recently concussed patients, but it lacks the depth needed for post-concussion syndrome patients.
Staff at UPMC don't offer any means to identify what areas of the brain were affected by the concussion. For example, concussions may cause highly localized or diffuse damage, yet patients may experience similar symptoms either way. In this case, how can they truly tailor treatment to the patient when therapists don’t know what parts of the brain are affected? For example, patients may experience short-term memory problems, but there are many brain regions involved in memory, and knowing exactly which ones to target makes it much easier to promote recovery.
At Cognitive FX, we don’t leave treatment outcomes to chance. Not only do our therapists design a tailor-made treatment plan for each patient based on the results of their scan, but different therapists are in constant communication with each other during the patient’s treatment to adjust the approach as needed.
UPMC Concussion Clinic vs Cognitive FX: Treatments Offered

Both clinics accept people of all ages for treatment of concussion and post-concussion syndrome. There is some overlap in therapies used, but the in-clinic experience is very different.
UPMC
Based on the results of their medical assessment, patients are placed into at least one of six categories (“types of concussion”), which will influence the treatment they receive. The six categories are:
- Cognitive and fatigue: Patients in this category have trouble with prolonged or complex cognitive tasks, which may get worse with increased fatigue. Common symptoms include poor concentration, trouble retaining information, and decreased multitasking skills.
- Vestibular: Patients in this category experience mainly problems with balance, motion, and vision.
- Ocular: Patients in this category experience vision problems, including trouble bringing the eyes together or tracking an object.
- Migraine: Patients in this category experience headaches, nausea, and sensitivity to light or noise.
- Cervical: Patients experience trouble with stress or pressure on the neck, spine, or spinal cord, which may lead to headaches.
- Anxiety and mood: Patients experience symptoms of anxiety and depression, which makes social interactions harder.
To treat these patients, the UPMC team of concussion experts includes neuropsychologists, neurosurgeons, neuroradiologists, neuro-optometrists, sports medicine doctors, vestibular and physical therapists, athletic trainers, and physiatrists (experts in physical medicine). These specialists may use a variety of different therapies to treat concussed patients, including:
- Vestibular therapy: The vestibular therapists at the UPMC concussion program use a variety of exercises to treat problems with dizziness, focusing, motor skills, balance, and hand/eye coordination. Typically, these therapists work closely with physical therapists.
- Exertion therapy: This type of therapy aims to help patients return to exercise after their injury. Therapists use aerobic and strength exercises to safely increase the patient’s heart rate, overcome exercise intolerance, and get back to the pre-concussion level of activity.
- Neuro-optometry (vision therapy): This therapy addresses the connection between the eyes and the brain. Neuro-optometrists use tailored exercises to improve vision problems, such as double vision, tracking problems, convergence insufficiency, inability to focus, and others.
- Orthopaedic consultation: This treatment is useful for patients experiencing certain symptoms, such as headaches and neck pain.
- Medications: UPMC doctors can prescribe a variety of treatments, including pharmacological options, to treat problems triggered by the concussion, such as sleep disturbances or headaches. Not all concussion cases require medicine, but UPMC doctors believe it can be useful in “complex cases” (aka, when patients present with chronic symptoms).
Many of these therapies are valid, helpful approaches to concussion management. That said, we recommend caution with medication. We’ve written extensively on why patients should be cautious with medication for post-concussion syndrome.
Unfortunately, many doctors do not have the resources to treat PCS fully, so they attempt to control specific symptoms with meds — migraine meds for headaches, nausea patches, antidepressants for cognitive and emotional symptoms, etc.
But these medications…
- Were never tested on brain injury patients.
- Do not target the underlying cause of the symptom (and therefore often do not provide relief for PCS patients).
- Are more likely to cause side effects in brain injury patients.
- May have negative interactions (we’ve seen patients come in with 7+ meds, some of which were not good to take in combination).
- And more.
There are specific circumstances where a patient is best served with medication, but it is rarely the right answer for post-concussion syndrome patients — especially before other therapeutic interventions have been tried.
For a more in-depth discussion on medications for PCS, read this post.
Cognitive FX
At Cognitive FX, we don’t categorize patients like the UPMC clinic does. Many of our patients would fall into all six of their categories if we did! Each patient is unique and receives a completely customized treatment plan. Our therapists use a cutting-edge combination of aerobic exercise and multidisciplinary therapies to target the root causes of PCS symptoms in patients, including neurovascular coupling disruption, autonomic dysfunction, vision changes, and vestibular issues.
Once patients complete the patient evaluation, they are ready to start treatment. Typically, this involves a three-step cycle that is repeated throughout the course of treatment: Prepare, Activate, and Recover.

Prepare
Treatment starts with short sessions of aerobic exercise intervals, typically on a stationary bike or treadmill. Physical exercise promotes healthy blood flow within the brain and triggers the release of many helpful neurochemicals, including one called brain-derived neurotrophic factor (BDNF). BDNF helps the brain to learn new information and boosts the efficacy of subsequent therapies.

Lauren Taylor Brem in neurointegration (advanced vision and vestibular) therapy.
Activate
During the second step, patients attend therapy to treat their PCS symptoms. While patients receive most of the therapies we offer, the exact combination of exercises within each therapy varies considerably depending on the results from the brain scan. This level of personalized treatment is something that UPMC does not offer.
Therapies Offered at Cognitive FX
At Cognitive FX, the primary purpose of each therapy is to stimulate healthier NVC in the brain regions identified as underperforming for each patient. Different therapies excel at helping different brain regions. All therapies are conducted in-house with close, daily communication between therapists to ensure they are fine-tuned for your needs.
|
Cognitive
therapy
|
- The aim is to engage key brain regions and rehabilitate cognitive skills, such as memory, attention, decision-making, and reasoning.
- Patients engage in cognitive activities, such as solving logic puzzles and identifying word patterns.
|
|
Occupational
therapy
|
- Patients engage in exercises that help the brain, body, and eyes coordinate with each other.
- Therapists help patients readjust to their daily activities by focusing on difficulties identified on their fNCI scan, including compensatory strategies for work and school as they recover.
|
|
Neuromuscular
therapy
|
- The aim is to relieve headaches and neck pain, rehabilitate balance, improve body-brain coordination, and promote physical activity.
- Patients receive massages, stretches, and soft tissue manipulation to increase blood flow.
- Patients also engage in cognitive games and physical therapy exercises.
|
|
Sensorimotor
therapy
|
- The aim is to improve cognitive and physical skills and reduce symptoms of depression.
- Patients follow simple movement patterns in time with a metronome to address cognitive, visual, and vestibular symptoms.
|
|
Vision
therapy
|
- The aim is to address vision problems, such as blurred vision, difficulty focusing, and light sensitivity.
- Patients engage in different exercises, including Dynavision, visual tracking exercises, the Brock String, and some other computerized technologies.
- If patients need further therapy after treatment, our therapists can help find a suitable neuro-optometric rehabilitation program.
|
|
Neurointegration therapy (vestibular therapy)
|
- The aim is to help with a variety of vestibular issues, including poor posture, dizziness, and vertigo. Vision exercises are often incorporated as well.
- Patients engage in gaze stabilization and balance exercises. For example, patients catch a ball while standing on a balance board or walk in a figure eight pattern while keeping their eyes focused on a point.
|
|
Psychotherapy
|
- Patients meet with a clinical psychologist to evaluate their mental health status.
- For patients suffering from depression and anxiety, our therapists recommend cognitive behavioral therapy (CBT). We do not offer this type of therapy but can refer them to a specialist.
- Patients learn mindfulness exercises and other relaxation strategies.
|
Note: While care for pediatric post-concussion syndrome patients is similar to that for adults, we tailor our approach based on age.
For further information, see our post on post-concussion syndrome in children.

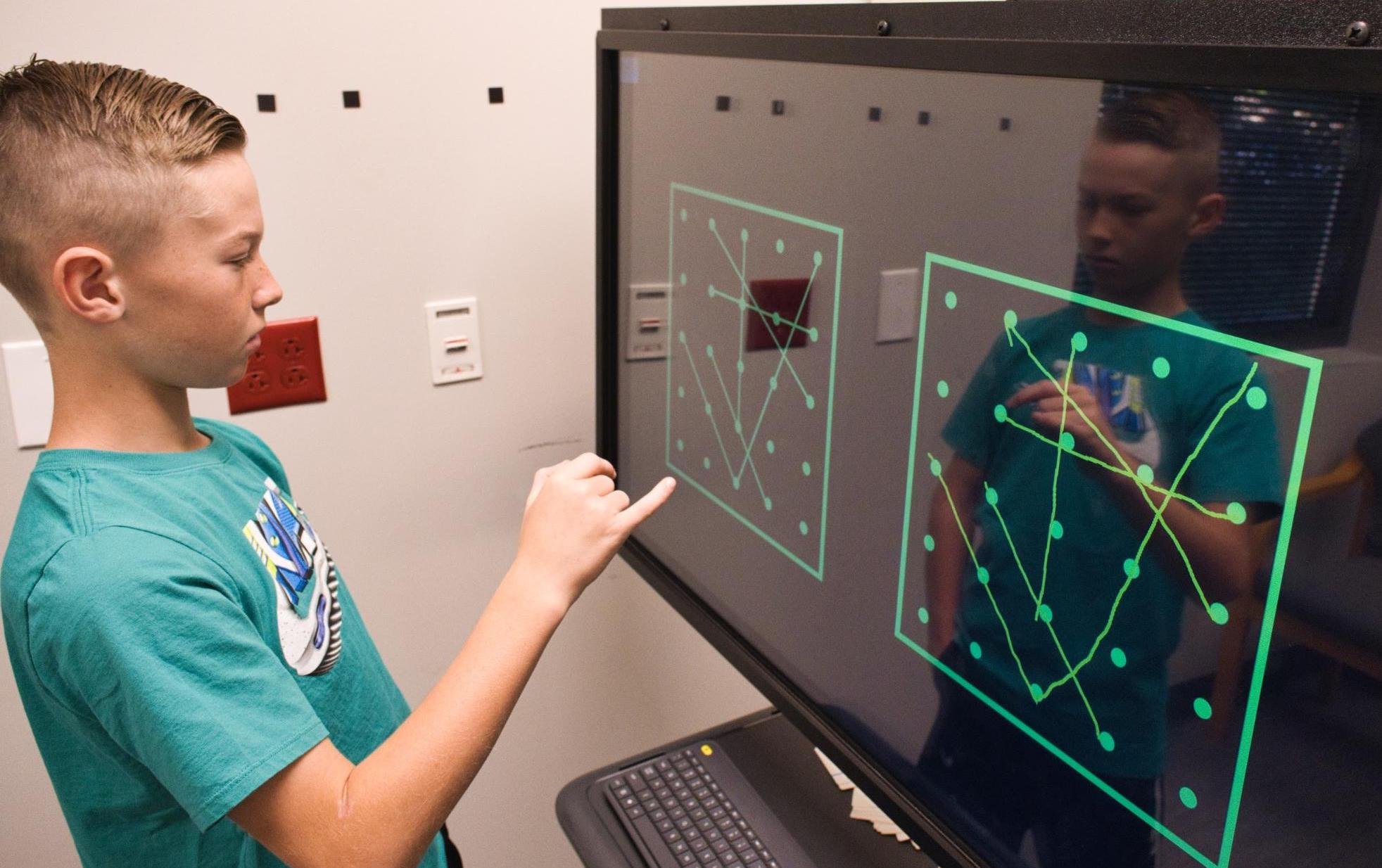
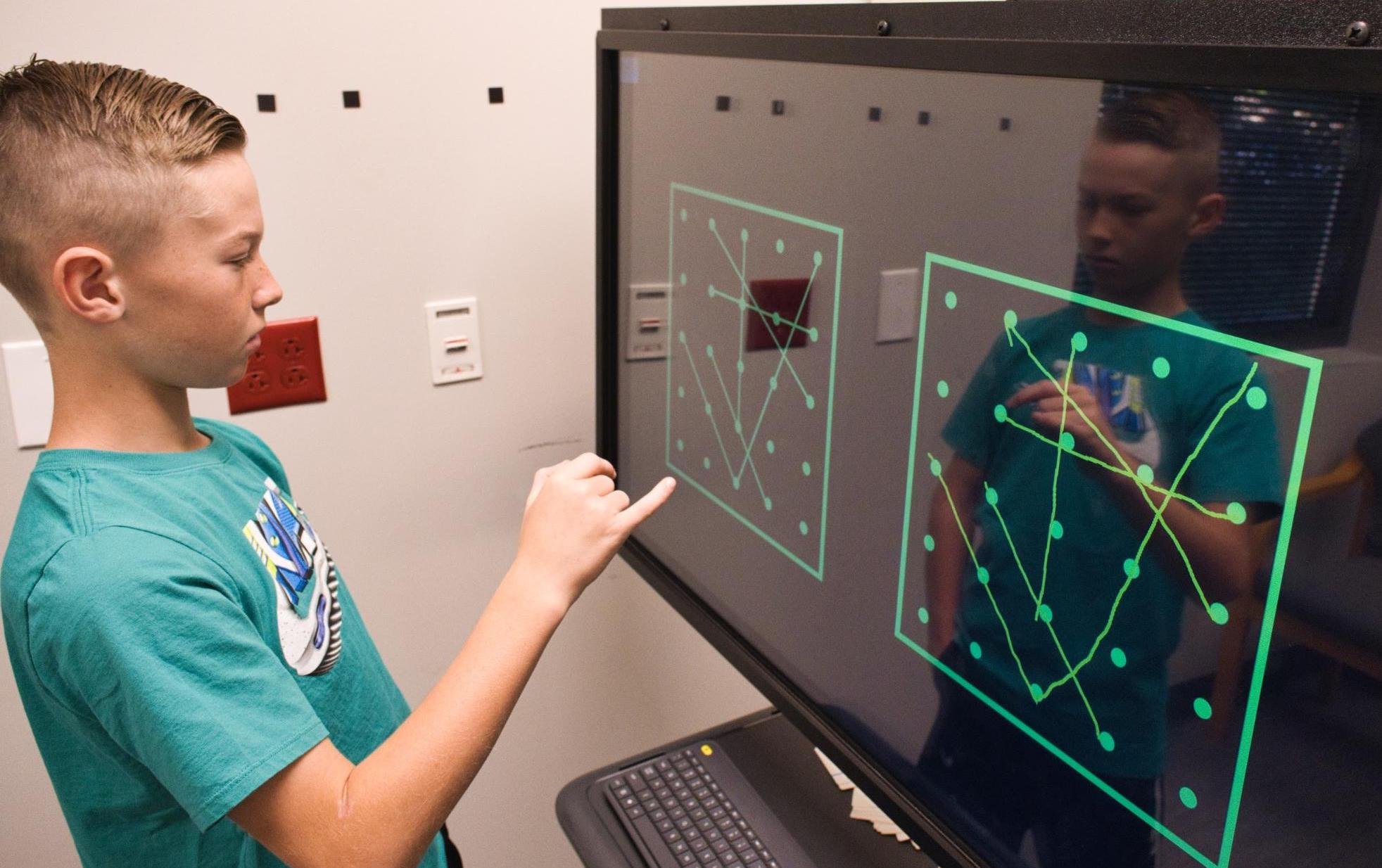
Patient Scotty Allen (from the Strange Parts YouTube channel) tries Dynavision therapy.
Rest
The final step involves time to unwind in between therapies. Patients learn a variety of breathing and mindfulness exercises, listen to brainwaves, or receive neuromuscular massage of the neck and shoulders.
At the end of treatment, patients undergo a second scan to see how their brain is responding to therapy. Then, patients meet with one of our therapists to discuss their progress and how to continue recovery at home.
Patients receive a series of exercises to do at home, typically including aerobic exercises, cognitive games, and relaxation techniques. These exercises take about one hour every day, five days a week. When patients start to feel better, they can gradually do these exercises less often. If needed, we refer patients to additional specialists, such as endocrinologists, psychologists, and vision therapists.
Key Takeaways
Both UPMC and Cognitive FX offer active therapy, but the patient experience is markedly different.
At UPMC, there is minimal communication between therapists. The vestibular specialist focuses exclusively on vestibular therapy, the physical therapist focuses on physical issues, and so forth. Exercises from each therapy are siloed, minimizing how many brain regions are active at one time. But one of the secrets to improving neurovascular function is to engage multiple brain regions at once.
In addition, there is minimal communication between therapists at UPMC concerning each patient. This approach is enough to treat acutely concussed patients but has lower chances of success for PCS patients. For example, in a study published by the UPMC team, PCS patients experienced some improvements in terms of memory and vision, but the treatment was not beneficial for many other cognitive skills and balance issues.
In contrast, at Cognitive FX, our therapists work together and often teach patients exercises to address different symptoms at the same time. For example, patients may be asked to balance on a Bosu ball (vestibular therapy) and recite the names of animals alphabetically (cognitive therapy) while catching a ball (vision/physical therapy). On top of that, our team is in constant communication regarding our patients’ progress and how to adjust the difficulty levels and type of therapy they receive. Our doctors and therapists use a Slack channel to troubleshoot therapeutic approaches between appointments. Patients are often surprised when Dr. Allen or Dr. Fong greet them in the hallway and comment on the therapy they just came from!
With this approach, over 90 percent of Cognitive FX patients experience improvements in symptoms by the end of their first week of treatment, and the average symptom improvement is over 60 percent. We can only boast this level of results for our patients thanks to an incredible level of coordination and communication between staff.
You can read more about our patients’ recovery journeys here.
Ready to begin your EPIC recovery journey? Sign up for a consultation.
UPMC Concussion Clinic vs. Cognitive FX: Pricing and Insurance

UPMC
UPMC has its own insurance provider, called UPMC for You. This covers services that are medically necessary for each patient. Some of the services may have limits, copayments, need a referral from a doctor, or require prior authorization by UPMC for You.
Patients can keep track of their health information on the UPMC Health Plan mobile app and get 24/7 medical advice with the UPMC MyHealth 24/7 Nurse Line.
Your treatment costs will depend on whether you carry this insurance, how much it costs you, what conditions you’re receiving treatment for, where you’re receiving treatment, which treatment you receive, the number of patient visits needed, and a host of other factors.
Cognitive FX
Cognitive FX is not an in-network provider with any insurance providers. We do provide CPT codes (see the full list on our pricing page), and some of our patients may obtain partial reimbursement when filing with their insurance companies.
Our treatment is costly but priced fairly for the services we offer. No other clinic in the world — including UPMC — has assembled a medical team as extensive as ours nor do they offer the same level of personalized treatment, thanks to the fNCI results.
We have four packages for patients to choose from, ranging from $2,500 to $24,700. If you choose the packages just with the brain scan — “fNCI only” or the “fNCI + Action plan” — but later decide to continue treatment with us, whatever you’ve already paid is credited to the cost of treatment.
So, for example, if you choose the fNCI scan only but then decide to move forward for one week of treatment, your treatment plan cost would be $10,500 ($13,000 less the $2,500 you had already paid). If you need help choosing, a member of our team would be happy to discuss options with you.
.jpg?width=1472&height=1999&name=Comparing%20Treatment%20Plans%20at%20Cognitive%20FX%20(2024).jpg)
Keep in mind that these costs are for true post-concussion syndrome treatment, which at our clinic goes far beyond the acute concussion care offered at many concussion clinics.
Final Comparison Between UPMC and Cognitive FX
Evaluation: The initial patient evaluation process is similar between both clinics, but Cognitive FX offers more in-depth physical and cognitive evaluations, then goes one step further with a functional brain scan to identify the areas affected by the concussion. These results are crucial in designing a customized treatment for each patient. UPMC cannot offer this level of personalization for treatment.
Treatment: Both clinics offer some of the same therapies, but treatment at UPMC is siloed between departments and sometimes even performed in different locations. (Their two main locations are the Water St. UPMC Rooney Sports Complex and the Cranberry Springs Drive UPMC Lemieux Sports Complex, but there are satellite locations as well.) At Cognitive FX, we know that integration between therapies is the best way to help our patients. Our in-house team is constantly in communication as they monitor patients and adjust treatment as needed to maximize the benefits for the patients.
Overall, we feel that UPMC offers a solid treatment for patients with an acute (recent) concussion. Their concussion research is important for helping future generations. But their approach is not ideal for PCS patients. At Cognitive FX, our therapists focus specifically on treating PCS patients and others with persistent symptoms from brain injuries. Your needs are unique; we don’t categorize you and hope for the best. We use multidisciplinary, evidence-based methods and cutting-edge technology to give you the best chance at recovery.
The average symptom improvement reported by our patients is 60 percent. To see if you’re a good fit for our program, sign up for a consultation.










.jpg?width=1472&height=1999&name=Comparing%20Treatment%20Plans%20at%20Cognitive%20FX%20(2024).jpg)