If you're suffering from persistent symptoms after a concussion — a condition called post-concussion syndrome (PCS) — you might think that Stanford Healthcare (part of Stanford University) would be a serious contender as your treatment provider. After all, Stanford Healthcare is world-renowned for combining clinical care, clinical research, and education to provide coordinated and personalized healthcare covering many different conditions.
However, despite its well-deserved renown for providing state-of-the-art therapies, Stanford Healthcare does not have a dedicated clinic for treating patients who are experiencing persistent symptoms after a concussion or traumatic brain injury (TBI). Instead, they have two separate departments located in Palo Alto, California — a Neuropsychology Clinic and an Outpatient Neurologic Rehabilitation Program — that focus on treating a wide array of neurological conditions and are more suited for treating acute concussions (i.e., concussions that have recently been sustained).
As we’ll explain later in this article, their approach is not ideal for patients with persistent post-concussion symptoms. Patients who experience symptoms for months or years after their concussion have much lower recovery rates when using the same approach as patients with recent concussions because their needs are no longer the same as acute concussion patients’.
At Cognitive FX, we specialize in treating this complex group of PCS patients. Our clinic brings together clinicians from over a dozen specialties to collaboratively provide evidence-based, multidisciplinary treatment tailored to the unique brain injury of each person who visits our clinic. This treatment program is designed to address the root causes of the symptoms directly, rather than tackling individual symptoms one at a time. This personalized, holistic approach leads to our unprecedented 90 percent treatment success rate.
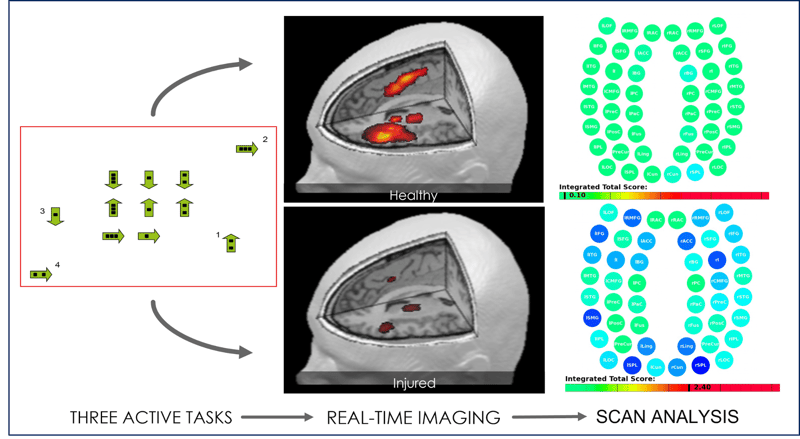
As a part of our evaluation process, we offer functional brain imaging that identifies which specific areas of your brain were affected by the injury and in what way. This allows us to tailor your treatment plan to your brain, something most clinics (including Stanford Medicine) simply cannot do.
Understanding which option — Stanford or Cognitive FX — is right for you depends largely on understanding the difference between recent concussion and post-concussion syndrome.
In this article, we’ll explain why each condition needs a different treatment approach and explore the differences between what we offer at Cognitive FX versus what is offered at Stanford, in terms of:
90% of our patients report reduced symptoms after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.
What Happens to the Brain After a Concussion (and Why Acute & Chronic Concussions Can’t Be Treated the Same Way)

The brain’s first reaction to a concussion is to trigger a localized inflammatory response in the affected area. This happens within 24 hours of the injury and is a crucial part of the brain’s recovery mechanisms, involving a series of chemicals released in the brain to aid the injured tissue.
Concussions and the resulting inflammation affect blood flow in the brain and cause changes in the way brain cells communicate with surrounding blood vessels to receive the resources they need to function. In a healthy brain, brain cells and blood vessels share a highly dynamic connection, one which allows brain cells to request the oxygen and nutrients they need to perform a particular task and have them delivered to the right location at the right time in the right amount. This is called neurovascular coupling (NVC).
Concussions disrupt this link; consequently, cells either receive the wrong amount (too little or too much) or get it at the wrong time. When this happens, cells are no longer able to complete the tasks assigned to them. Your brain will try to complete the task using an alternative pathway, but this pathway will inevitably be less efficient, causing you to tire out more quickly. This NVC dysfunction causes a variety of symptoms, some of which are associated with different concussion subtypes, such as headaches, brain fog, and fatigue.
The brain has an incredible ability to recover, however, and can use brain cells that remain healthy after the injury. The brain can fix the neural pathways disrupted by the concussion or form new ones to regain lost functions. This mechanism is called neuroplasticity. In patients who recover within a few days after their concussion, this is a straightforward process. At this stage, neurovascular coupling disruption is easily reversible by itself or with some simple therapy (cardiovascular exercise, physical therapy, vision therapy, and/or vestibular therapy as needed) to “nudge” neuroplasticity in the right direction.
Unfortunately, for some patients, not all symptoms resolve within this period. At least 15 percent of patients experience persistent symptoms that last months or even years, but that number can be as high as 60 percent depending on geographical location, injury severity, quality of care, and so forth. These patients suffer from a condition called post-concussion syndrome (PCS).
In these patients, the brain keeps using less efficient pathways to complete tasks even after inflammation has resolved. Once neurovascular coupling disruption becomes more established, it’s more challenging to treat. Standard therapies used to treat concussed patients are often not enough to treat PCS patients. Instead, PCS patients benefit from a customized, multidisciplinary therapeutic approach to restore healthier neurovascular signaling pathways.
In PCS patients, treatment is further complicated because brain injuries can also lead to chronic symptoms stemming from a combination of secondary conditions, including autonomic nervous system dysfunction, vision and vestibular problems, hormone imbalance, and breathing problems.
For example, the autonomic nervous system (ANS) — which controls many bodily functions, including heart rate, blood pressure, digestion speed, and body temperature — often becomes dysfunctional after a concussion.
Under normal circumstances, the ANS’ main branches, the sympathetic nervous system (SNS, which controls the fight-or-flight reaction) and the parasympathetic nervous system (PNS, which controls the rest-and-digest response), work together in harmony. However, in TBI patients, the SNS can become dominant even when there’s no need to react to a stressful situation. As a result, patients experience symptoms such as irregular breathing, high or low blood pressure, neck pain, headaches, digestive issues, dizziness, sensitivity to light, and more.
Further reading: Post-concussion ANS dysfunction (dysautonomia)
Vision problems are also common after a concussion and can prevail for a long period if not treated properly. PCS patients may experience a wide range of post-concussion vision problems, such as double vision, tired eyes, and problems with focusing and eye teaming (how the eyes work together). Vision therapy is often effective for patients who experience visual symptoms for longer than three months.
Some patients also experience changes in vestibular function. Mild traumatic brain injuries can disrupt the connection between the brain, vision, and vestibular system, which makes it harder for the brain to understand where it's positioned relative to its surroundings. This leads to symptoms such as headache, dizziness or vertigo, balance problems, and spatial disorientation. Fortunately, post-concussion vestibular therapy is very effective for these issues.
Brain injuries can also damage the hypothalamus and pituitary glands and cause hormonal imbalance. These small structures are responsible for controlling hormone levels in the body. Structural or functional damage to these areas disrupts the production of many different hormones, causing multiple symptoms throughout the body, including low blood pressure, weight gain, low libido, amenorrhea, heart palpitations, hair loss, fatigue, mood swings, and headaches.
Further reading: Hormone dysfunction following head injury
Finally, concussions may affect breathing dynamics, disrupting the mechanisms that regulate the levels of carbon dioxide (CO2) and oxygen (O2) in the bloodstream. Breathing issues can cause patients to feel dizzy and lightheaded, have frequent headaches, or struggle with physical activity. Breathing exercises — an important part of the treatment we offer at Cognitive FX — go a long way to help accelerate the patient’s recovery.
As you can see, post-concussion syndrome is vastly more complex than acute concussion. This information is key to understanding which concussion treatments represent the best option for you.
Treatment plans for patients with a recent concussion typically involve cardiovascular exercise complimented by one or two standard therapies (physical, vision, and/or vestibular therapy) done over a few sessions. For most patients, this is usually enough to correct neurovascular dysfunction and eliminate symptoms.
In contrast, treatment for post-concussion syndrome is more challenging. Symptoms persisting longer than three months mean neurovascular disruption has become more established. In this case, patients need a more detailed evaluation process to find out exactly how and where the concussion affected their brain and which secondary conditions are present, followed by customized therapy sessions to address their specific situation.
With that in mind, we can now discuss key similarities and differences between the concussion treatment program at Stanford and Cognitive FX.
Staff Expertise

Stanford
Stanford’s concussion treatment team is centered around treating recently concussed patients. They do not currently have a dedicated department for treating persistent post-concussion symptoms.
As we mentioned above, Stanford has two main departments that assess and treat concussion patients: the Neuropsychology Clinic and the Outpatient Neurologic Rehabilitation Program at Stanford Neuroscience Health Center.
Some patients come directly from the Neuropsychology clinic to the outpatient rehabilitation program. Still, the rehabilitation team also works closely with clinicians and medical providers from other locations (including the emergency department) who refer their patients to the rehabilitation center. They treat thousands of concussed patients every year with a customized treatment plan developed for each patient.
Combined, these two departments offer the following in terms of staff expertise:
Neuropsychologists assess patients after a severe or mild traumatic brain injury, including:
- Conducting a comprehensive neuropsychology assessment (see below for patient evaluation)
- Providing treatment recommendations, including to address cognitive and behavioral symptoms caused by the injury
- Assessing if patients are ready to return to work or school
Occupational therapists provide treatments to help patients with daily activities, including:
- Finding ways to carry out activities of daily living (ADLs)
- Engaging in physical exercise
- Recommending adaptive equipment as needed, such as wheelchairs or bars in the bathroom
- Finding ways to return to school or work
- Engaging in driving simulation training
- Screening for cognitive impairments
Physical therapists teach patients exercises to improve strength, flexibility, coordination, balance, and mobility skills. Treatments include:
- Mobility training
- Gait and balance training
- Vestibular and concussion rehabilitation
- Robotic-assisted strengthening
- Equipment prescription, such as mobility devices, orthopedic shoes and orthoses, and functional electrical stimulation (FES)
Speech and language pathologists suggest treatments to improve communication and other cognitive skills. They can also help patients who struggle to swallow after a TBI. Treatment includes:
- Speech and language retraining, including voice therapy
- Cognitive retraining
- Communication retraining for conditions such as aphasia, dysarthria, and dysphonia
- Swallow evaluation and treatment
In extreme cases, patients can also be referred to the Neurosurgery Program (part of Stanford Brain Performance Center), where a team of neurosurgeons treats both adult and pediatric patients with complex head injuries.
Cognitive FX
By comparison, the staff at Cognitive FX specializes in PCS patients who develop persistent cognitive, physical, and emotional symptoms for months or even years after their head injury.
To treat PCS patients, we have a diverse team of nurses, doctors, and therapists including:
- Neurosurgeon (neurosurgery specialists)
|
|
|
|
- Speech-language pathologists
|
- Clinical neuropsychologists
|
|
|
|
- Vision and vestibular specialists
|
|
|
- Athletic trainers and sports medicine specialists
|
|
|
- Licensed massage therapists
|
Our team has years of experience diagnosing and treating the main causes of PCS symptoms, including the common problems discussed above:
Thanks to our advanced imaging capabilities (described below), our team can determine exactly what areas were affected by the concussion and design a treatment plan tailored to each patient’s needs.
Summary
Stanford
- Their Neuropsychology Clinic is equipped to provide comprehensive neurological assessments and treatment recommendations for patients with a wide array of conditions, including concussions and TBIs.
- Their Outpatient Neurologic Rehabilitation Program has an experienced multidisciplinary team that is best suited for treating recently concussed patients.
- They do not currently have a dedicated department for treating patients with persistent symptoms lasting months or years after their injury.
Cognitive FX
- The team includes a wide range of medical specialties highly relevant to treating lingering symptoms of brain injury, such as neurosurgery, clinical neuropsychology, neuroscience, cognitive therapy, physical therapy, massage therapy, vestibular therapy, occupational therapy, and more.
- This team is entirely focused on treating persistent, long-term symptoms of brain injury. Cognitive FX is where you would go when you ‘graduate’ Stanford’s acute concussion or TBI program but your recovery is not complete and you still have limitations you’d like to overcome.
Patient Evaluation

Stanford
Stanford’s neuropsychological evaluation (offered through their Neuropsychology Clinic) starts with a series of clinical interviews with the patient and their family (or close friend) to review the patient’s medical history and understand how the concussion has affected their emotional and cognitive skills. Typically, this initial interview takes about an hour to complete.
The second step involves a series of standardized cognitive and behavioral tests to check the patient’s:
- Attention and concentration
- Mental efficiency
- Learning and memory
- Problem-solving, reasoning, planning, and organization
- Language and speech
- Visual-perceptual and spatial abilities
- Sensory-perceptual and motor abilities
- Emotions, behavior, and personality
All the information is then gathered and used to design personalized treatment recommendations for the patient. Results can help therapists at their Outpatient Neurologic Rehabilitation Program assess whether patients are ready to return to work/school and engage in important life activities, such as managing their finances and driving. If needed, they can also suggest adaptations at home or work to optimize their chance of a successful return.
Cognitive FX
All our patients receive a comprehensive evaluation, starting with the patient’s medical history and symptoms. Patients undergo a variety of exams, including:
- A physical exam that assesses balance, hand-eye coordination, functional vision, reaction times, and other physical abilities. For example, patients have to perform a series of tests using digital eye-tracking software to help our therapists identify vision deficits, such as difficulty tracking or poor peripheral vision.
- A cognitive assessment that checks memory, focus, thinking, and other cognitive skills.
- A psychological evaluation intended to spot symptoms of mental health problems, such as anxiety and depression.
![EPIC Treatment Yellow Puzzle [V1]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20Yellow%20Puzzle%20%5BV1%5D.jpg?width=1999&height=1241&name=EPIC%20Treatment%20Yellow%20Puzzle%20%5BV1%5D.jpg) One of the timed exercises included in patient evaluations at Cognitive FX.
One of the timed exercises included in patient evaluations at Cognitive FX.
During the initial evaluation, our team also looks for signs of ANS dysfunction, and a neurointegration specialist evaluates how well the patient’s inner ear, eyes, and body communicate with each other. We repeat the same tests at the end of the treatment week to assess how much the patient has improved.
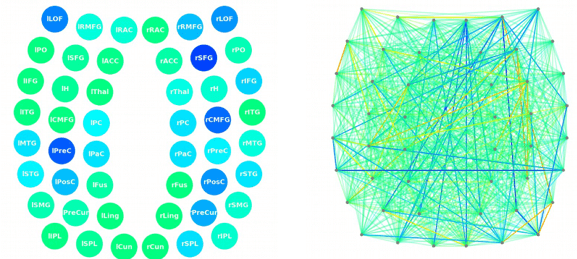
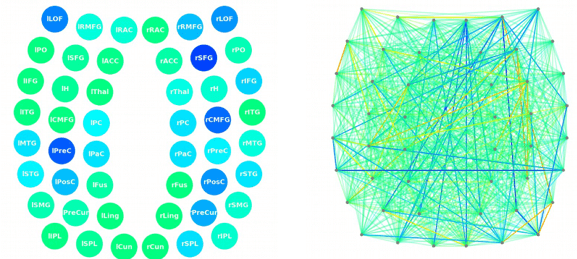
Patients also complete a specialized brain scan called functional Neurocognitive Imaging (fNCI). This scan assesses blood flow in 100 different regions in the brain while patients complete a set of predetermined cognitive tasks. The resultant near-real-time images are then combined and compared to a healthy control database to identify the areas where NVC dysfunction is disrupting normal functioning. Key regions of the brain each receive a score that reflects their performance. Scores in the yellow to red sections indicate neurovascular coupling dysfunction in the areas of the brain responsible for that particular cognitive function.
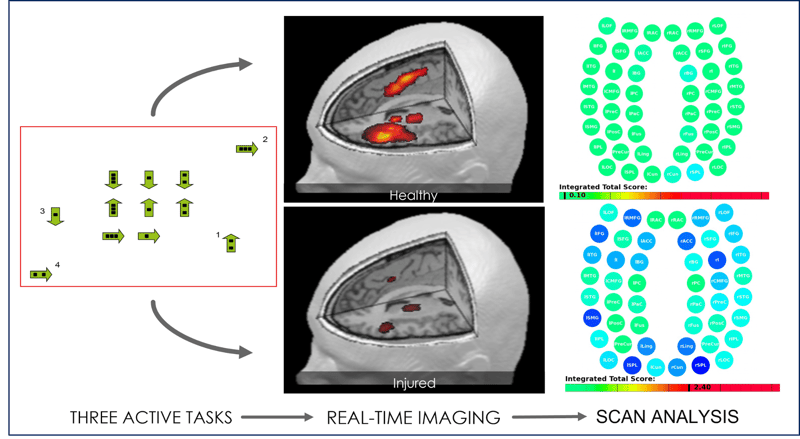

The scan also measures how different brain regions communicate with each other. In this case, regions in green are normal, whereas areas in blue are less active than expected. For example, in the image below, rACC (the right anterior cingulate cortex) shows less activity than usual. This area is crucial for attention and could contribute to memory problems if not functioning normally.
This scan is a key part of our patient evaluation and is something Stanford does not offer.
Patient story: How a former figure skater learned years of chronic illness was due to post-concussion syndrome
Once all assessments are complete, our team can design a personalized treatment plan to target exactly the areas of the brain that showed dysfunction.
Summary
Stanford
- Patients complete a neuropsychological evaluation, which includes an interview with the patient, a review of their medical history, and a series of tests to assess physical, cognitive, and emotional symptoms.
- While Stanford’s concussion evaluation may be sufficient for recently concussed patients, it’s not an ideal fit for PCS patients with persistent and lasting symptoms. These types of paper and pencil neuropsychology tests often do not have the sensitivity to capture the cognitive changes that PCS patients have experienced. For example, they may score within normal limits on these tests while having significant functional issues that can only be seen on specialized brain imaging scans (like what we offer at Cognitive FX).
Cognitive FX
- Cognitive FX follows a detailed patient evaluation that considers medical history, the patient’s list of symptoms, and the results of physical, cognitive, and emotional evaluations.
- All patients undergo an fNCI brain scan which reveals blood flow patterns (an approximation for brain function) in 100 brain regions. This data is used to design a custom-made treatment plan for each patient.
Treatments Offered

Stanford Clinic
Because Stanford’s Neuropsychology Clinic only offers assessment and treatment recommendations, their treatment is limited to what they offer through their Outpatient Neurologic Rehabilitation Program, which typically includes occupational, physical, and speech therapy.
Some of their facilities include:
- Gym space
- Private treatment rooms
- Outdoor spaces to practice mobility skills on varied terrains
- Equipment for body weight support, standing and walking, balance and vestibular rehabilitation, and return to driving
- Equipment for strengthening, balance, standing and gait training, visual-perceptual testing and training, and speech and voice therapies
Treatment options offered for concussion patients include:
- Body-weight support gait and balance training: Patients use motorized adjustable parallel bars to support their upper body and reduce the weight on their legs. The aim is to train weak leg muscles and improve standing, walking, and running.
- Occupational therapy: Occupational therapists help concussed patients through techniques that enable them to return to work or a normal daily routine.
- Physical therapy: Physical therapists design an exercise plan to help patients maximize function in specific body parts and relieve muscle pain.
- Speech-language pathology: Speech-language therapists help patients improve communication, cognition, and swallowing. Typically, these sessions are conducted in soundproof rooms to ensure the patient’s privacy.
- Vestibular rehabilitation: Patients with vestibular issues receive a customized exercise program to improve balance and reduce dizziness.
- Functional mobility training: These sessions involve a number of exercises to help patients navigate different types of surfaces like ramps, stairs, mulch, cobblestones, and sand.
- Driving simulation training: Driver simulation programs enable patients to practice their driving skills after their concussion. Patients can also use an accessible parking area for practicing transfers in and out of a car.
- Functional electrical stimulation devices: Some patients are treated with electrical stimulation devices to improve neuromuscular symptoms.
- Robotic-assisted strengthening: For severe injuries, patients can be treated with robot-assisted therapy to help increase their range of motion and improve posture.
After treatment, the team at Stanford also provides patients with a list of exercises to do at home. This program is gradually adapted as patients improve and reach their goals. If needed, the therapists also discuss with patients the options for continuing treatment in a community-based setting.
Cognitive FX
At Cognitive FX, our therapists use a cutting-edge combination of aerobic exercise and multidisciplinary therapies to target the root causes of PCS symptoms in patients, including neurovascular coupling disruption, autonomic dysfunction, vision changes, and vestibular issues.
Once patients complete the patient evaluation, they are ready to start treatment. Typically, this involves a three-step cycle that is repeated throughout treatment: Prepare, Activate, and Recover.

Prepare
Treatment starts with short sessions of aerobic exercise intervals, typically on a stationary bike or treadmill. Physical exercise promotes healthy blood flow within the brain and triggers the release of many helpful neurochemicals, including one called brain-derived neurotrophic factor (BDNF). BDNF helps the brain to learn new information and boosts the efficacy of subsequent therapies.
 Lauren Taylor Brem during neurointegration (advanced vision and vestibular) therapy.
Lauren Taylor Brem during neurointegration (advanced vision and vestibular) therapy.
Activate
During the second step, patients attend therapy to treat their PCS symptoms. While patients receive most of the therapies we offer, the exact combination of exercises within each therapy varies considerably depending on the results of the brain scan. This level of personalized treatment is something that Stanford does not offer.
|
Therapies Offered at Cognitive FX
At Cognitive FX, the primary purpose of each therapy is to stimulate healthier NVC in the brain regions identified as underperforming for each patient. Different therapies excel at helping different brain regions. All therapies are conducted in-house with close, daily communication between therapists to ensure they are fine-tuned for your needs.
|
|
Cognitive therapy
|
- The aim is to engage key brain regions and rehabilitate cognitive skills, such as memory, attention, decision-making, and reasoning.
- Patients engage in cognitive activities, such as solving logic puzzles and identifying word patterns.
|
|
Occupational therapy
|
- Patients engage in exercises that help the brain, body, and eyes coordinate with each other.
- Therapists help patients readjust to their daily activities by focusing on difficulties identified on their fNCI scan, including compensatory strategies for work and school as they recover.
|
|
Neuromuscular therapy
|
- The aim is to relieve headaches and neck pain, rehabilitate balance, improve body-brain coordination, and promote physical activity.
- Patients receive massages, stretches, and soft tissue manipulation to increase blood flow.
- Patients also engage in cognitive games and physical therapy exercises.
|
|
Sensorimotor therapy
|
- The aim is to improve cognitive and physical skills and reduce symptoms of depression.
- Patients follow simple movement patterns in time with a metronome to address cognitive, visual, and vestibular symptoms.
|
|
Vision therapy
|
- The aim is to address vision problems, such as blurred vision, difficulty focusing, and light sensitivity.
- Patients engage in different exercises, including Dynavision, visual tracking exercises, the Brock String, and some other computerized technologies.
- If patients need further therapy after treatment, our therapists can help find a suitable neuro-optometric rehabilitation program.
|
|
Neurointegration therapy (vestibular therapy)
|
- The aim is to help with a variety of vestibular issues, including poor posture, dizziness, and vertigo. Vision exercises are often incorporated as well.
- Patients engage in gaze stabilization and balance exercises. For example, patients catch a ball while standing on a balance board or walk in a figure eight pattern while keeping their eyes focused on a point.
|
|
Psychotherapy
|
- Patients meet with a clinical psychologist to evaluate their mental health status.
- For patients suffering from depression and anxiety, our therapists recommend cognitive behavioral therapy (CBT). We do not offer this type of therapy but can refer them to a specialist.
- Patients learn mindfulness exercises and other relaxation strategies.
|
Note: While care for pediatric post-concussion syndrome patients is similar to that for adults, we tailor our approach based on age.
For further information, see our post on post-concussion syndrome in children.
 Patient Scotty Allen (from the Strange Parts YouTube channel) tries Dynavision therapy.
Patient Scotty Allen (from the Strange Parts YouTube channel) tries Dynavision therapy.
Rest
The final step involves time to unwind in between therapies. Patients learn a variety of breathing and mindfulness exercises, listen to brainwaves, or receive a neuromuscular massage of the neck and shoulders.
At the end of treatment, patients undergo a second scan to see how their brain is responding to therapy. Then, patients meet with one of our therapists to discuss their progress and how to continue recovery at home.
Patients receive a series of exercises to do at home, typically including aerobic exercises, cognitive games, and relaxation techniques. These exercises take about one hour every day, five days a week. When patients start to feel better, they can gradually do these exercises less often. If needed, we refer patients to additional specialists, such as endocrinologists, psychologists, and vision therapists.
Summary
Stanford Clinic
- Treatments offered include traditional physical, occupational, and speech therapy, as well as options to address some specific problems experienced by concussed patients, including mobility training, driving simulation, and robotic-assisted training.
- Treatments are likely to help patients with acute concussions but will be less effective for patients with post-concussion syndrome.
Cognitive FX
- Offers a combination of aerobic exercise and multidisciplinary therapies backed by years of research (both independent research and in-house research). Therapies offered include cognitive therapy, vision and vestibular (neurointegration) therapy, sensorimotor therapy, neuromuscular and physical therapy, occupational therapy, psychotherapy, and more.
- Therapies used during treatment are tailored based on the fNCI brain scan results for each patient, which allows for a more targeted treatment.
- Patients engage in exercises that target more than one symptom at the same time to maximize recovery.
- Our team is in constant communication with each other to discuss each patient’s progress and adapt their treatment as needed.
Pricing and Insurance

Stanford
At Stanford, patients receive a pricing range for their treatment, but estimated prices are not guaranteed. The actual therapies that patients receive may differ from the services used to compile the estimated price. This is especially true if doctors need to order more tests than originally thought. Patients can use the Cost Estimator to estimate out-of-pocket costs for some of the services offered by Stanford Health Care.
Stanford Health Care is contracted with most major health insurance carriers including CalPERS, Medi-Cal, Medicare, TRICARE and TriWest. Financial counseling is available to help patients identify possible ways to pay for their care if they do not have adequate funds or health insurance.
Cognitive FX
Cognitive FX is not an in-network provider with any insurance providers, but we can provide CPT codes (see the full list on our pricing page), and some of our patients may obtain partial reimbursement when filing with their insurance companies.
One advantage that we have over Stanford is that patients know exactly how much their treatment is going to cost. There are no hidden or extra costs. We offer four packages for patients to choose from, ranging from $2,500 to $24,700. If patients choose one of the packages with just the brain scan — “fNCI only” or the “fNCI + Action plan” — but then decide to continue treatment with us, the initial cost is credited to the cost of treatment. For example, if you choose the fNCI scan only but then decide to attend one week of treatment, your treatment plan cost would be $10,500 ($13,000 less the $2,500 you already paid for the scan).
.jpg?width=1472&height=1999&name=Comparing%20Treatment%20Plans%20at%20Cognitive%20FX%20(2024).jpg)
Final Comparison Between Stanford and Cognitive FX
Patient Evaluation: Patient evaluation starts similarly between both clinics, but Cognitive FX then goes one step further by using a functional brain scan to identify the exact areas affected by the concussion. Results from the scan are then used to design a customized treatment for each patient.
Treatments Offered: Both clinics cover some of the same therapies, but at Stanford, each therapy is offered in isolation by different therapists. At Cognitive FX, we know the key to treating PCS patients is integration between therapies. Our team members are close collaborators who constantly communicate with each other to monitor patients and adjust treatment as needed.
In conclusion, the treatments offered by the Stanford team may be enough to treat patients shortly after their concussion, but their methods are not ideal for patients with persistent PCS symptoms lasting more than three months. We understand that PCS patients have unique needs and offer them multidisciplinary, evidence-based methods and cutting-edge technology to give them the best chance at recovery.
The average symptom improvement reported by our patients is 60 percent. To see if you’re a good fit for our program, sign up for a consultation.




![EPIC Treatment Yellow Puzzle [V1]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20Yellow%20Puzzle%20%5BV1%5D.jpg?width=1999&height=1241&name=EPIC%20Treatment%20Yellow%20Puzzle%20%5BV1%5D.jpg)




 Patient Scotty Allen (from the
Patient Scotty Allen (from the
.jpg?width=1472&height=1999&name=Comparing%20Treatment%20Plans%20at%20Cognitive%20FX%20(2024).jpg)








