Why is a concussion called a "mild" TBI?
A concussion is a result of the head receiving a significant blow or jolt causing the brain to impact with the skull. This sudden movement will cause the brain to bounce or twist in the skull,...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Many viral and bacterial infections are capable of affecting the brain and causing widespread dysfunction that may outlast the acute disease symptoms. Patients with long-term symptoms after viral encephalitis or meningitis may suffer from fatigue, headaches, difficulty concentrating, sleep issues, memory problems, emotional changes, and more.
The good news is that, in many cases, these symptoms are treatable if you know where to turn for help. While we primarily treat concussion patients whose symptoms never went away with time and rest, we’ve also treated patients who have recovered from conditions like bacterial and viral meningitis and carbon monoxide (CO) poisoning. The brain dysfunction they experienced was identical to that of concussion patients because the effect of inflammation on the brain is the same whether it’s from a viral illness or a mild traumatic brain injury. Because of that, the same therapy that works for the concussion patients works for them as well.
Now that we’re years into the pandemic, we also have more information about how COVID-19 affects the brain. While it doesn’t frequently cause encephalitis, it can and does affect the brain and nervous system for many patients, resulting in long COVID.
To help you better understand how viral infections lead to long-term effects, we’ll explain…
Have your symptoms lingered for weeks or months after an infection? If you’ve experienced concussion, viral encephalitis, meningitis, hypoxia, carbon monoxide poisoning, or another source of brain trauma, sign up for a free consultation. We’ll discuss your medical history and determine if you’re a good candidate for treatment. Over 90% of our patients show significant improvement from just one week of treatment.
Yes, a viral infection can affect the brain, directly and indirectly. Bacterial infections and parasites can do so via similar mechanisms, but we’ll focus on viruses for the purposes of this post.
There’s a well-known cohort of viruses known to be capable of causing brain damage, such as herpesviruses (like herpes simplex virus [HSV], Epstein-Barr virus, and the varicella-zoster virus, which you know from chicken pox), mumps, rubella, and West Nile virus. But there’s more than one way to affect the brain, and more common viruses (even, on occasion, the common flu) are capable of causing brain trauma as well.
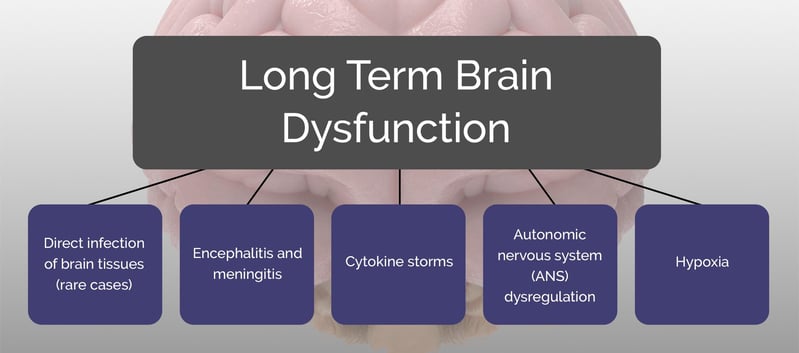
There are five main ways we see patients suffering from neurological symptoms due to infection:
Some patients may suffer from one; some may have more than one causing problems jointly. Here’s a quick explanation of each.
Some viruses are capable of crossing the blood-brain barrier to infect brain cells (neurons, astrocytes, and so forth). It’s the least common of the methods listed in this post. But when an infectious disease is capable of directly infecting brain tissue, it’s a hard fight for survival. The virus (or your immune system attempting to fight the virus) could cause the death of infected brain cells, which is often permanent damage (and not something we can fix).
Patients who do survive will likely have lingering health issues to unravel and work through — something that we can help with. In fact, we’ve already helped many people with lasting brain damage from severe TBI (in which there was permanent damage we could see on the scan). We can’t reverse that damage, but we can help the rest of the brain adjust.
Encephalitis is swelling and inflammation of the brain; meningitis is swelling and inflammation of the protective membrane that covers the brain and spinal cord (meninges). Encephalopathy is the term used to describe when the damage from either (or both) is permanent. All three can be caused by a virus. Someone with encephalopathy typically experiences long-term symptoms of encephalitis (sequelae).
Swelling and inflammation can interfere with the connection between brain cells and the blood vessels that supply them (neurovascular coupling, or NVC). Dysfunctional neurovascular coupling is at the heart of lingering symptoms for post-concussion patients, which is why we’re often able to help viral encephalitis survivors, too.
This is an example of indirect brain damage from a virus. The virus causes encephalitis (or meningitis), which in turn causes long-term brain dysfunction that can often only be resolved with treatment.
Cytokines are chemicals your body produces for several jobs, including to help guide your immune response. Certain cytokines can ramp up your inflammation response to infection; others latch on to infected cells to mark them for death.
When cytokines overreact and harm — or even kill — healthy cells, that’s called a cytokine storm (or cytokine soup). It’s one of the more serious reactions you can have to a virus; many patients with a cytokine storm end up in the ICU (intensive care unit) at their local hospital. The results are widespread dysregulation and inflammation; one of the long-term effects can be concussion-like symptoms.
Almost any trauma can affect our autonomic nervous system, and viruses are no exception. For some patients, the sympathetic nervous system (think fight-or-flight response) may not relax after the threat (the virus) has been eliminated.
An overactivated nervous system can cause all kinds of symptoms, such as headaches, blood pressure issues, heart palpitations, light and noise sensitivity, gastrointestinal issues, and more.
Further reading: Nervous system dysfunction following COVID-19
Hypoxia — having low oxygen in some or all body tissues — can also cause long-term symptoms if it occurs in the brain. If a virus causes difficulty breathing (like COVID-19) or directly infects and interferes with lung cells, hypoxia could be the result.
Any disruption of oxygen to the brain could cause problems; for example, we’ve even seen and treated patients who had lingering symptoms from carbon monoxide poisoning (which deprived their brains of sufficient oxygen). When you disrupt the brain’s oxygen supply, dysregulation of neurovascular coupling (NVC) often follows.
Note: There is some disagreement in the literature as to whether NVC is directly damaged by hypoxia or whether there is another step in between (for example, perhaps the lack of oxygen in the brain leads to hypoxia-induced encephalopathy which leads to problems with NVC). Regardless, hypoxia is involved in leading to the decoupling, which in turn produces physical and cognitive impairment.
Acute encephalitis from COVID-19 is rare and has only been observed in severe cases. Researchers estimate that it is only present in 2% of patients who exhibit neurological symptoms. Most research into whether COVID-19 can directly infect brain cells has been gathered via lumbar puncture (spinal tap) for cerebrospinal fluid analysis. At this time, most evidence indicates that COVID is not directly infecting the central nervous system (unlike viruses that cause encephalitis via direct infection, such as enteroviruses).
Nevertheless, a notable number of patients have suffered neurological symptoms driven by immune activation, inflammation, and other dynamics. Doctors are using a variety of tests, including CT scans, MRI, blood tests, and EEG (electroencephalogram) to better understand what happens to COVID patients who suffer neurological complications. At our clinic, we use functional neurocognitive imaging (fNCI) to evaluate brain function changes in long COVID patients.
Further reading: Diagnosis and treatment for long-haul COVID patients
Yes, concussion and post-concussion syndrome sufferers could be at risk for more severe symptoms. To clarify, they are no more likely to contract the illness than anyone else, but if they do contract COVID-19, then there are several reasons they may have a harder time handling the illness.
Many post-concussion patients have some level of ANS dysregulation. They can have problems with vasculature (blood vessels) regulation, and their breathing may be dysregulated as well. Therefore, they are more at risk for difficulty breathing and for an immune system overreaction — the cytokine storm mentioned earlier.
Keep in mind that the autonomic nervous system has some control over the cytokine response. In very general terms, the sympathetic nervous response(fight or flight) will promote the inflammatory cytokines; the parasympathetic nervous system(rest & digest) will promote anti-inflammatory chemicals. A nervous system skewed toward the first will be more likely to have serious difficulties during the fight against COVID-19.
In addition to following guidelines from the Centers for Disease Control and Prevention (CDC), there are some things you can do to give your body the best chance at fighting the coronavirus, should you get sick:
Many patients recovering from encephalitis, COVID, or other viral or bacterial infections report experiencing weeks or months of fatigue afterward. Fatigue after an infection isn’t abnormal, but it shouldn’t drag on past the first few weeks after initial recovery, regardless of the cause of encephalitis. If you haven’t made a full recovery, there may be some long-term symptoms you need to get in check.
We’ve seen and treated patients who have recovered from meningitis, CO poisoning, and even hypoxia induced by sleep apnea! Their brains looked like the brains of post-concussion patients, with hyperactive and hypoactive brain regions appearing on their fNCI scans (a type of fMRI, or functional magnetic resonance imaging).
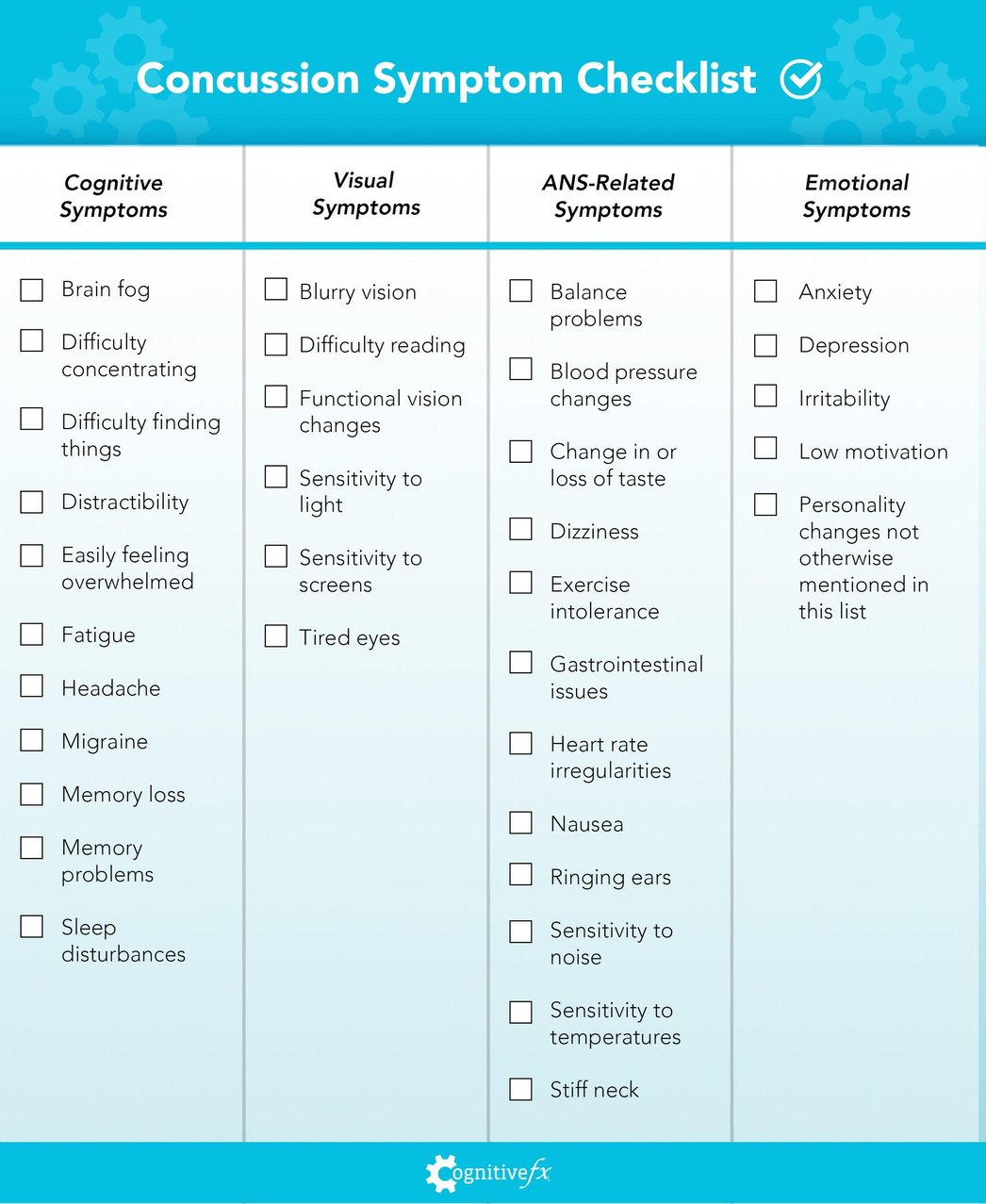
Some common persistent post-illness symptoms include…
Cognitive Symptoms
Visual Symptoms
ANS-Related Symptoms
Emotional Symptoms
Be attentive to your body. If you think something is wrong, don’t let other people brush you off, especially when it comes to your mental health. Well-meaning people can say things like, “Oh, you’re just stressed right now.” But a common cause of depression in brain injury survivors, in addition to trauma or situational issues, is a chemical imbalance. If you think there’s something more to your post-illness mood changes, it’s worth seeking help rather than trying to wait it out on your own.
If you’re experiencing the above symptoms long after your battle with the virus has ended, seek help from a trained medical professional who can either provide therapy or refer you to a knowledgeable provider.
Here is some additional reading for long-COVID patients:
It is incredibly frustrating to experience lingering symptoms and not know why. Some of our patients suffered for decades before finding our clinic and undergoing treatment. Many doctors simply don’t know what causes these symptoms and are therefore poorly equipped to diagnose and treat them. Sometimes, our patients have been told by other doctors that they’re imagining their pain or making up symptoms to get attention.
Lingering symptoms after a viral infection, concussion, or another source of brain trauma are real, and we can see the changes in your brain to prove it using functional neurocognitive imaging (fNCI). This imaging technique allows us to see which regions of your brain were affected and how.
fNCI looks at blood flow dynamics throughout 56 brain regions while the patient performs a series of standardized cognitive tasks. Our protocol also examines the health of connections between those brain regions.
We’re then able to infer the health of brain regions involved in specific tasks, such as multitasking, logical reasoning, attention shifting, and visual feature detection. Here’s an example report showing unhealthy neurovascular coupling dynamics: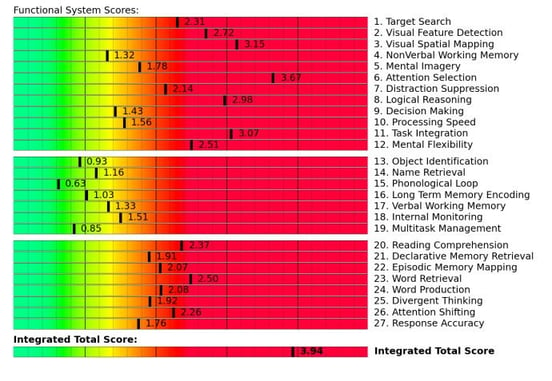
Scores in the yellow and red zones indicate neurovascular coupling dysfunction. Brain regions that score poorly on the fNCI are a focus during treatment because they’re most in need of rehabilitation. Using that information, we then administer a regimen of therapy designed to kickstart the brain’s inherent neuroplasticity (its ability to adapt and improve based on external and internal stimuli).
Before diving into complex therapies, patients engage in short bursts of cardio followed by measured breathing. This step improves blood flow within the brain and releases neurochemicals that help you benefit more from therapy. One of those neurochemicals, brain-derived neurotrophic factor (BDNF), improves cognitive flexibility and has been shown to improve therapy outcomes in brain injury patients. The same principles apply for patients whose brain dysfunction stemmed from viral infection.%20(7).jpg?width=800&height=533&name=Yes%2c%20COVID%20Affects%20the%20Nervous%20System%20(%26%20What%20to%20Do%20About%20It)%20(7).jpg)
Post-viral patients, especially those who are recovering from long-COVID, may need shorter bursts of exercise with a longer recovery period and more training via breathing exercises. Their breathing dynamics are often altered during the acute phase of viral infection and need to be rehabilitated..jpg?width=800&height=533&name=Why%20Most%20Post-Trauma%20Vision%20Syndrome%20Treatment%20Falls%20Short%20(4).jpg)
Therapy — consisting of neuromuscular therapy, sensorimotor therapy, cognitive therapy, occupational therapy, psychotherapy, vision therapy, vestibular therapy, and more — is tailored to your specific needs, as identified during the fNCI and other in-person examinations. These therapies work together to encourage healthier neurovascular coupling in affected brain regions. They also serve to help rebalance the autonomic nervous system and improve vision and vestibular function.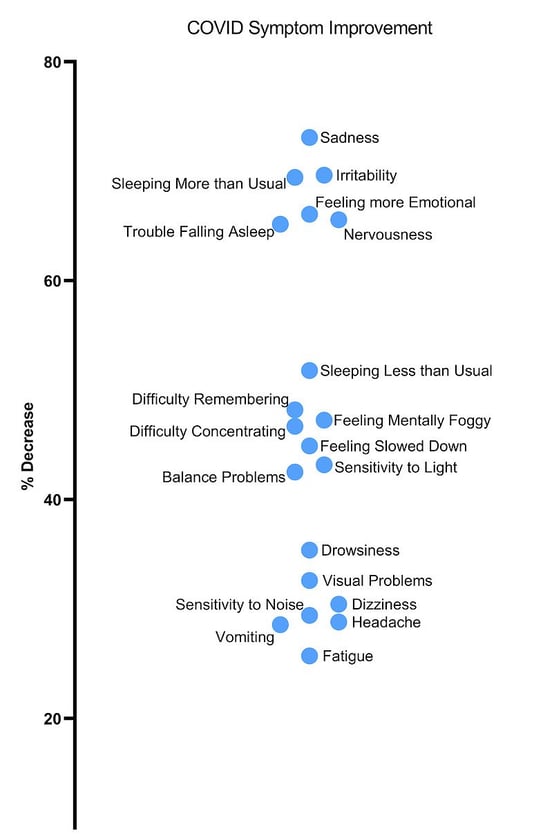
Average percent decrease in symptom severity across 43 long COVID patients. As we collect results from more patients these numbers may change.
Exercises our patients complete are often multidisciplinary. For example, you might balance on a Bosu board (exercising your vestibular system and the part of the brain governing balance) while tossing a football back and forth (hand-eye coordination and reflex response) and naming a city for each letter of the alphabet (word recall). Or, during neurointegration therapy, you might trace the mirror image of a geometric shape while solving mental math problems.
These exercises activate brain regions and encourage recovery in ways that siloed therapy cannot. With our extensive, multidisciplinary staff, we’re able to help you achieve better long-term outcomes from your illness than many other healthcare providers.
Want to learn more? Read about our EPIC treatment program, or see what our patients have said about their journey to recovery.
If you want to learn if you are a good candidate for treatment, schedule a consultation.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

A concussion is a result of the head receiving a significant blow or jolt causing the brain to impact with the skull. This sudden movement will cause the brain to bounce or twist in the skull,...

You hit your head five, ten, maybe twenty years ago. The doctors said you were fine. The scans came back normal. Everyone told you it was "just a concussion" and you'd bounce back in a few weeks.

Many hospitals offer robust medical treatment to help patients survive traumatic brain injuries (TBIs). It’s common for those same hospitals, or affiliated care providers, to offer rehabilitation to...

Brain injury recovery is hard. The severity of your injury, which parts of your brain were affected, and how they were affected, all factor into things such as how much you can recover and how long...

Between 80,000-90,000 people who suffer traumatic brain injuries (TBIs) each year develop long-term disabilities related to their TBI. Many others suffer from a variety of long-term, problematic...

"All I remember is hearing screeching and then blackness," Anthony Loubet said as he talked about the car accident that changed his life.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY