If you’ve experienced a traumatic brain injury (TBI), it’s natural to want to know how long and how difficult your recovery is going to be. There are so many factors affecting recovery time — such as the specifics of the injury, gender, treatment options, and more. Remember, the length and extent of your recovery is unique to you. Recovery stories vary even between patients with similar injuries.
But the good news is that — with the right support — TBI patients with long-term symptoms can continue to show improvement even many years after the injury.
To some extent, the success you see during recovery is linked to your willingness to engage in therapy and persist with treatment recommendations. But it’s also possible to try so hard that you wear out your brain and slow down recovery progress. Or, your brain might only respond to a type of therapy to a point, and then need something else to move forward. Recovering from a TBI is a “work smarter, not harder” situation. You need the right professional guidance at each stage of your recovery.
At our clinic, Cognitive FX, we’ve treated numerous TBI patients who stalled in their long-term recovery before reaching out to us. They were working hard, trying their best, but not seeing the improvements they wanted to see. That’s because they had reached the limit of what their current providers could help them through.

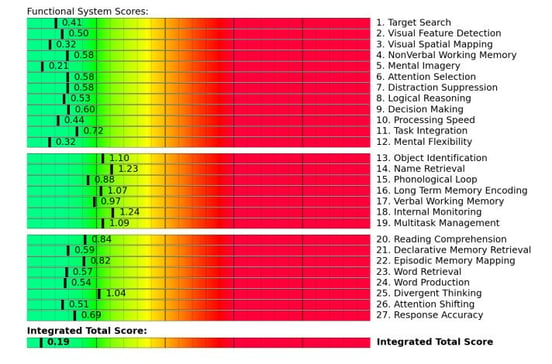
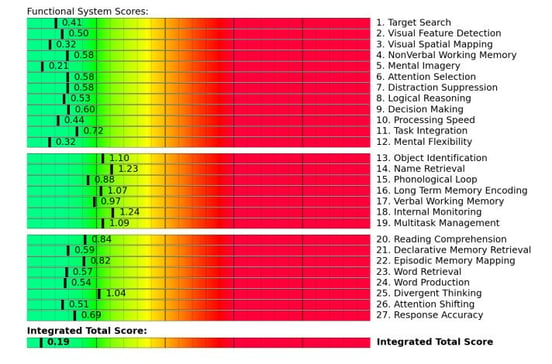
But with our advanced imaging techniques (functional Neurocognitive Imaging, or fNCI for short), we can “see” which parts of the brain are underperforming compared to a database of healthy brain images. Armed with this insight, we can tailor the many therapies at our disposal to target your unique brain injury (more on this in a bit).
Although we cannot guarantee a full recovery for every patient, we’ve seen many of our patients with severe traumatic brain injuries improve beyond their initial prognosis. While you might never return to the level of functioning you enjoyed before the injury, you can still make great progress and find significant symptom relief.
In this article, we’ll explain our treatment approach and other aspects of brain injury recovery you should know, including:
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
Neuroplasticity: How the Brain Recovers after a Traumatic Brain Injury
Before we dive in, it’s helpful to know how the brain attempts to repair itself after a traumatic brain injury.
Unlike some animals that can grow new nerve cells to repair damaged portions of their brains, our capacity for regeneration is more limited. We can repair a cut by growing new skin cells, but we can’t recover from a brain injury in the same way.
Nevertheless, our brain has an incredible ability to use nerve cells that are still healthy after the injury. It can reorganize communication pathways in the brain through a mechanism called neuroplasticity. Because each nerve cell has thousands of different connections, your brain can use some of these connections to find alternative pathways to accomplish what the damaged nerve cells used to do.
In practical terms, when the brain is injured, it can bypass the damaged cells by forming new connections between neurons to regain lost functions.
Think about neuroplasticity as your brain using Google Maps: If the quickest route is blocked, Google Maps will find you an alternative route. It may take you longer, but you will get to your destination.
The problem is that neuroplasticity doesn’t always kick in strongly after an injury. And when it does, it doesn’t always result in the best new pathways. If our brains automatically forged the best new communication routes everytime they became available, we wouldn’t ever need rehabilitation therapies! Instead, most people have lingering symptoms that can be improved by therapies that encourage better neuroplasticity — such as cognitive therapy, sensorimotor therapy, physical therapy, vision therapy, and more.
The other issue is that your brain doesn’t operate in isolation. A traumatic brain injury can cause a host of issues throughout your body. TBIs can also lead to autonomic nervous system dysfunction, vestibular dysfunction, hormone dysfunction, and more.
A recovery plan needs to take all of those systems into account, too, which means you may need to see a variety of specialists who can collaborate to provide you with a cohesive care plan. Your care team will need to know which long-term symptoms you’ve developed so they can use that information, along with any objective testing data, to treat you appropriately.
What Persistent Symptoms May Develop after a Traumatic Brain Injury (TBI)?

Long-term symptoms after a traumatic brain injury are a mixture of symptoms that develop immediately after the incident and persist for a long time (e.g., headaches and dizziness) and symptoms that might appear weeks or even months later (e.g. depression and insomnia).
Here’s a look at some of the more common long-term symptoms, including physical, cognitive, and emotional symptoms.
Physical Symptoms
One of the most common complaints we hear is fatigue. This is not surprising at all: Your brain is working double time to perform even simple tasks! Recovering from a brain injury takes energy, as does every effort you make to function normally. Fortunately, fatigue is also one of the easier symptoms to fix.
Other physical issues caused by a brain injury can include:
Cognitive Impairments
Cognitive complaints are more difficult for most healthcare providers to diagnose and treat. If you’re struggling to read, for example, is it because of vision problems? Is it because you struggle with attention? Is your short-term memory at fault? Or is it because you suffer from constant brain fog? There are many possible causes of cognitive problems, and it takes an experienced practitioner with neurological experience and access to the right diagnostic tools to pinpoint the causes.
Some common cognitive complaints include:
- Long or short-term memory loss or other memory problems
- Short attention span
- Difficulty concentrating
- Poor decision making
- Poor spatial orientation
- Poor safety awareness
- Difficulty processing new information
- Difficulty finding the right word in a conversation
- Difficulty expressing ideas
- Difficulty following a conversation
- Brain fog
- Feeling overwhelmed
Emotional and Behavioral Symptoms
Emotional and behavioral symptoms can be very confusing. You might feel happy one minute, then fly into a rage over what would previously have been a minor inconvenience or annoyance (such as a child banging on a pan or the fridge ice machine breaking). You might have mood swings throughout the day or feel depressed all the time.
Mental health changes can have a number of possible causes — they could stem directly from the damage to your brain tissue, they might stem from your brain’s overwhelmed state, they might be tied into nervous system overactivation, or another cause. Emotional changes can be tricky to treat and require considerable patience and understanding from yourself and others.
Changes in mood or behavior after a TBI may include:
Treatment for Persistent TBI Symptoms at Cognitive FX

Finding the right treatment to address long-term TBI symptoms is a crucial part of your recovery, but for many patients, this aspect of recovery is not as simple as it sounds.
If you need treatment immediately after a brain injury — in ER or an urgent care clinic — doctors and other healthcare professionals will treat any serious or even life-threatening injuries that need immediate medical care, such as bleeding in the brain, a blood clot, or a skull fracture. And once that’s done, the hospital can provide some inpatient or outpatient rehabilitation as required by your injury severity.
But that brain injury rehabilitation is primarily focused on activities of daily living. Your therapists want to make sure you can speak, walk, and care for yourself as much as possible. They provide much-needed support if you need to relearn how to tie your shoes and wash your face. But where do you go when you’ve recovered these abilities?
Most family doctors are not well-educated about long-term symptoms after a traumatic injury. And even if they are, they may or may not know local therapists who are capable of helping. If you do find good therapists, they’re often scattered across multiple medical practices, so you have to drive (or more likely, be driven to) many appointments in inconvenient locations. And even then, most of them aren’t talking to each other, so they only see one piece of your condition — not the whole picture.
At Cognitive FX, we understand that all of your persistent symptoms are interconnected. Instead of addressing each symptom separately, we aim to treat the root of the problem by treating the parts of the brain that are injured.
Our process starts with a functional Neurocognitive Imaging (fNCI) scan.
This is a special type of MRI that can measure how the blood flows in 56 regions of the brain. During the scan, patients perform cognitive tasks that allow our doctors to see how specific parts of the brain react when they need to complete a task. The scan reveals which parts of the brain function normally and which were affected by the injury. The scan also evaluates the connections between brain regions.
In a healthy brain, nerve cells receive oxygen and nutrients from the surrounding blood vessels. This relationship is called neurovascular coupling, and it ensures that each cluster of neurons receives the right amount of resources at the right time, allowing brain cells to function normally.
After a brain injury, however, this connection between brain cells and the blood vessels is disrupted, making it difficult for certain parts of the brain to function properly. This condition, known as neurovascular coupling dysfunction, is one of the main causes of persistent brain injury symptoms.
After your fNCI scan, we design and explain your customized treatment plan at Cognitive FX. At this stage, we’ll also discuss with you what level of recovery you should expect. We often see patients recover beyond what even we expect (and we have more optimistic expectations than most providers). Most patients make significant progress, but a complete return to pre-injury ability is rare.
During treatment week — which we call Enhanced Performance in Cognitive (EPIC) Treatment — we use a combination of aerobic exercise and a range of multidisciplinary therapies, including neuromuscular therapy, occupational therapy, cognitive therapy, psychotherapy, neurointegration therapy, sensorimotor therapy, and vestibular therapy, to name a few.

Patients cycle through periods of aerobic exercise (to boost beneficial neurochemicals like BDNF and prime the brain for therapy), multidisciplinary therapy appointments, and rest.
For example, you might start the morning with cardio intervals on a stationary bike while a therapist monitors your vitals and ensures that you exercise enough to get the boost but not so much that you trigger a serious increase in symptoms. Afterward, they might perform neuromuscular massage to relax your neck muscles and alleviate headache and vision symptoms.
From there, you might progress to cognitive therapy and sensorimotor therapy. In one session, you’ll be memorizing images and solving logic puzzles; the next, you’ll be clapping in time with a metronome while finding Taboo words. As the day progresses, you’ll continue to alternate between active therapy, cardio, and periods of rest.

The specific therapies you complete are tailored to your symptoms and the specific issues we identified during your fNCI scan.
At the end of the treatment, each patient undergoes a second fNCI scan to see how their brain is adjusting. Some scans show marked improvement, and others reveal a brain that is still reorganizing its connections. Most patients feel their brain improving and their symptoms fading throughout treatment.
At this stage, our therapists meet with you again again to organize a post-care plan. This includes a range of exercises to do at home to continue recovering at home, plus any recommendations for follow-up care in your area of residence.
90% of our patients show symptom improvement after just one week at our clinic. To see if you are eligible for treatment, sign up for a consultation.
How Long Does Traumatic Brain Injury (TBI) Recovery Take?

Unfortunately, there isn’t a one-size-fits-all answer. Some patients experience a fast recovery in a short period of time, while others recover more gradually. The good news is that — thanks to neuroplasticity — recovery after brain trauma is possible even for patients with severe injuries.
For example, one study showed that 13% of patients with a severe injury managed significant improvements within the first six months. In a separate study, 28% of patients with a severe injury made a full recovery four years after the injury, and 79% were capable of independent living.
But numbers from study to study vary considerably.
For example, according to the Centers for Disease Control and Prevention (CDC), only 26% of patients over the age of 16 who received inpatient hospital care in the U.S. for a TBI showed improvement during the five-year post-injury span of time.
In the past, many doctors and rehab specialists believed that recovery was limited to a two-year window after the injury. After that, they thought the brain was no longer capable of improving. But researchers now know this idea is incorrect. Traumatic brain injury patients can continue to recover long after the two-year mark. For example, this study showed that patients were still improving five years after their injury, even if the injury was severe.
Obviously, not all TBI patients recover at the same rate. Generally, patients with more severe brain damage who experienced lengthy loss of consciousness, a coma, or were in a vegetative state need a longer recovery time and may not make a full recovery. Most patients with a mild traumatic brain injury — commonly known as a concussion — recover fully within a few weeks, but some do not recover within the expected two-week to three-month timeframe. Up to 30% of patients continue to experience symptoms for months or even years after the concussion. This is called post-concussion syndrome (PCS), and it can be debilitating for the injured person.
While injury severity (often quantified with a Glasgow Coma Scale score) plays a major role in predicting recovery after an injury, it’s not the only factor involved. Other factors that can affect the brain’s chances of recovery include:
- Post-traumatic amnesia. Sometimes patients go through a period of amnesia after their injury. Typically, the shorter this period of amnesia, the better the prognosis.
- Age. Usually, patients over 60 or very young infants have the poorest prognosis after an injury.
- Location of injury. Chances of recovery are generally higher for those with localized head injuries compared to diffuse injuries, as the damage is limited to one area of the brain. This is not always the case. For example, if the affected area is involved in vital functions, such as the brain stem (which regulates activities essential for life), a full recovery may be more challenging.
- Pre-existing health conditions. Patients with a history of health conditions like anxiety, depression, headaches, and seizures may need more time to recover from a brain injury.
- Motivation and support. Recovery outcomes are best when the patient is highly motivated to continue treatment and pursue recovery, even during times when there are no significant improvements. Having a good support system of friends, family, and treatment providers makes a big difference, too.
- Gender. On average, females take longer to recover from a traumatic brain injury than males. For these patients, long-term symptoms are more likely to develop if the injury occurs during the luteal phase of their cycles (the roughly 14 days between ovulation and menstruation). Some studies suggest that this happens because of changes in hormones, namely estrogen and progesterone.
Click here to read more about how a brain injury affects women.
By the time patients come to our clinic, they’re often several years into their recovery journey. In just one week with us, they make remarkable progress, which they can continue building upon at home. But as we’ve said before, how much you improve and how long that improvement takes is unique to you.
What Else Can You Do to Maximize Recovery?

A good treatment plan goes a long way to ensure your recovery, but there’s more you can do:
- Get support from family and friends.
- Get help with emotional symptoms.
- Follow best practices at home.
- Read recovery stories from past patients.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation.
Get Support from Family and Friends

Getting family involvement is paramount to your recovery after a brain injury. Rehabilitation is more than just recovering from physical symptoms; emotional support from friends and family can do wonders for anyone recovering from an injury.
Studies show that support from a loved one encourages patients to stick to their treatment plan and increases their chances of recovery better than those who are getting the same rehabilitation without family support. Family and close friends can also detect subtle changes in your behavior that medical professionals may miss because they don’t have a close connection with you.
We’ve put together a resource for family members, friends, and caregivers to learn more about how to help you. You can send them our post about how to help someone with a TBI if they’d like to learn more.
Here are few ways for you to help them help you:
Explain what you’re going through: You may find it difficult to put into words what you’re feeling and how your symptoms affect your life. It’s worth trying, though, because having a better understanding of brain injury and its effects can help your loved ones understand what you need and be more patient when you act in ways they’re not used to.
Ask for support: Friends and family may be willing to help but don’t necessarily know what you need. You might ask them to do your shopping or accompany you and take notes at important medical appointments.
Share your frustrations: A traumatic brain injury can affect the entire family in different ways. There’s a range of emotions: worry, guilt, anger, helplessness, and grief, among others. Family members may need to adjust to new routines and adopt new responsibilities, at least for a while. This may create some tension and frustrations between you and your family. It’s better to have a frank and open discussion about the situation before it turns into resentment. Many people find talking to a therapist helps them through this time.
Address changes in your relationship: A traumatic brain injury can have a significant impact on your relationship with your partner. Despite all the pressures of recovery, take some time not only for needed serious conversations, but also for some lighthearted fun. Even just a quiet night in or a romantic stroll can do wonders to boost your morale and reaffirm your commitment to each other.
Get Help with Emotional Symptoms

As described earlier, traumatic brain injuries can often cause emotional and psychological changes, including serious mental health disorders such as depression, anxiety, and PTSD. Studies show that about 20% of patients experience mental health symptoms up to six months after a mild TBI, and this value increases to 50% during the first year after more severe injuries.
In addition, there’s a higher risk of developing mental health problems for patients who suffered from psychiatric illnesses before the injury, but every patient is different. You can develop depression and anxiety after a brain injury even if you never experienced them before.
If you notice that you’re having problems with your emotions, it’s time to talk to your physician or neuropsychologist. There are several types of therapy that can help you, with cognitive behavioral therapy being the most effective.
If absolutely necessary, you can also try medications to help improve or stabilize your mood. That said, most medications were never tested in brain-injured patients and often do not help or have bad side effects.
Your counselor may be able to help you:
Develop a treatment plan: A mental health professional can develop a suitable treatment plan. Look for someone who can offer concrete strategies for both coping in the moment and long-term recovery.
Grieve and sort through your feelings: TBIs can have lifelong implications. Your life, including your career and relationships, may change in unexpected ways. It’s healthy and normal to grieve after a TBI. Your counselor can help you process your feelings about the injury — sadness, anger, guilt, or otherwise — and help you move toward emotional healing.
Balance hope and realism: Part of your emotional recovery involves having a clear idea of what healing looks like. Your therapist can guide you towards hopeful yet realistic expectations. For example, patients are more likely to learn to cope with recurrent headaches if they know they will experience them for a while, but they can still hope they will subside after enough treatment.
Adjust back to life: Mental health counselors can help you reintegrate into your life. This includes, for example, making sure athletes are mentally ready to return to their sport or slowly reintroducing students into the classroom.
Though traumatic brain injuries can have far-reaching effects on a patient, therapists and psychologists can help them adapt to changes and return to a healthy life.
You can find more information about ways to navigate mental health problems after a traumatic brain injury in some of our previous posts.
In addition, we have resources on how to find a support group for post-concussion syndrome, which many TBI patients will find relevant.
Ways to Maximize Recovery at Home

As you navigate the months (or years) of TBI recovery, there are many adjustments you can make at home to maximize the extent of your recovery:
- Complete the exercises that our therapists recommend at the end of your treatment. Typically, this includes some aerobic exercise, cognitive activities, and breathing exercises.
- Follow your doctor’s advice about when it’s safe to drive a car or play sports.
- Avoid both alcohol and caffeine, at least initially. Both of them can slow down your recovery.
- Follow a brain-friendly diet.
- If you’re experiencing problems with short-term memory, write yourself notes or use an app on your phone to remind you of what you have to do. Build up your skills by trying to remember each task before checking your notes.
- Focus on one task at a time rather than attempting to multitask. Look for a quiet environment with minimal distractions when you need to focus (if possible).
- If you feel irritated or angry, walk away from the situation and try relaxation or breathing techniques to help your brain destimulate.
- Follow a set sleep schedule (see this article on sleep after TBI for help with sleep problems), and take short breaks during the day when you feel tired.
- Pace yourself on tasks that trigger your symptoms, whether it’s heavy house cleaning or financial decisions.
- Consult with family members or close friends when making important decisions.
- Avoid sustained computer use, including video games, early in the recovery process.
Other Patients’ Recovery Stories

A traumatic brain injury can feel isolating. But you’re not as alone as you might feel. While the majority of our patients come to us with persistent post-concussion symptoms, we’ve also treated many patients with severe TBI and other types of brain injury.
Here are a few of their stories…
Jamie’s Story
During a competition in 2015, professional athlete Jamie suffered a severe brain injury after a skiing accident. As a result, she lost the use of the right side of her body. With the help of her family, she began the hard journey to relearn to perform even simple tasks, like drinking water or climbing stairs. She made some improvements but felt that she was always on the verge of depression.
Finally, in 2019, Jamie found Cognitive FX. During her week-long treatment, she noticed that attending different therapies made her very tired and she needed to sleep more. She was a little nervous to receive the results of the second scan, but then was ecstatic to see how much her brain had improved. She’s since noticed benefits in her daily life, including finding it easier to hold a conversation.
Click here to read more about Jamie’s story.
Samuel’s Story
After years of suffering fatigue, "brain fog“, short-term memory loss, and depression, Samuel finally traced back these symptoms to a brain bleed he had when he was 11 years old.
During his assessment at Cognitive FX, he learned that several areas of his brain were still affected by that injury. He found treatment particularly grueling, but now he feels like he woke up from a bad dream. Everyone around him noticed a difference in him.
If you want to find out more about Sam’s recovery journey, you can read the full story here.
Aimee’s Story
Aimee suffered a severe traumatic brain injury in a car accident in 2001. For seventeen years, Aimee experienced headaches, memory loss, personality changes, exercise intolerance, dizziness, and light and sound sensitivity.
Aimee had some reservations about the treatment at Cognitive FX at first, but soon after starting treatment, she changed her mind. The therapies that stood out for her were occupational therapy, neuromuscular therapy, and Dynavision. Now, Aimee can multitask, and both her memory and vocabulary are much better.
Click here to read more about Aimee’s incredible recovery.
Abigail’s Story
Abigail suffered a brain injury after falling 70 feet off a cliff in the summer of 2016. She was unconscious and in a critical condition when she was admitted to hospital, and doctors placed her in an induced coma for three months. Afterwards, Abigail worked hard to improve and slowly began to regain her motor skills.
She made a remarkable recovery and even managed to return to college after just two years. However, Abigail continued to look for ways to improve. When she found Cognitive FX, the first scan revealed several areas in the brain that were still affected. After treatment, she noticed significant improvements in sleep and cognitive function. She feels that she’s 95% recovered and is very optimistic about the future.
Click here to learn more about Abigail’s amazing and inspirational story.
Ryan’s Story
As a teenager, Ryan suffered a severe brain injury during a car accident. Following the accident, Ryan struggled with memory loss, trouble focusing, poor sleep, headaches, and fatigue.
Nothing seemed to make any difference until he found Cognitive FX, where he started to feel better after the first day of treatment. During the week, he also noticed an improvement in focus, multitasking, and memory.
For him, the genuine compassion from the therapists created a comforting and reassuring environment, which made a huge difference in his recovery process.
Click here to read more about Ryan’s success story.
90% of our patients show symptom improvement after just one week at our clinic. To see if you are eligible for treatment, sign up for a consultation.





















.jpg?height=175&name=Slow%20Concussion%20Recovery%20(6).jpg)