A Guide to Post-concussion Syndrome on Reddit
Post-concussion syndrome is downright frustrating to experience. Doctors often miss it during diagnosis, and even if they do make the diagnosis, treatment methods vary considerably from clinic to...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Recovering from a head injury is an emotional, difficult journey whether you’re male or female. On that journey, women face a few hurdles that men do not. Today, we’d like to talk about those hurdles and a few ways you can handle them as they come.
If you’re suffering from persistent post-concussion symptoms, you’re not alone, and you’re not crazy! Up to 30% of men and women who sustain a mild traumatic brain injury develop lasting symptoms (known as post-concussion syndrome, or PCS). If you know something is wrong, don’t let your doctor brush it off. Keep fighting for the healthcare and treatment you need.
We have treated thousands of patients at our post-concussion syndrome clinic. In this post, we cover common issues our female patients report, along with the background information you need to understand PCS in women. We cover:
This isn’t to say that men don’t have challenges to overcome in recovery, or that they never face some of the issues covered here. But we’ve treated hundreds of women who struggled with these same issues for years without getting the support they needed. We hope this resource will help you understand that you’re not alone and that there is help.
If nothing else, just knowing these problems exist can help you approach each one with a better knowledge of your options, which makes a difference in treatment outcomes and your emotional well-being.
If you’ve been suffering from symptoms connected to a possible brain injury, we may be able to help. 95% of our patients show statistically verified restoration of brain function. Schedule a consultation to discuss your symptoms with a member of our team.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.

You can sustain a concussion (mild traumatic brain injury, or mTBI) from a blow to the head, severe jostling, or whiplash. During the injury, your brain hits the skull, resulting in the bruising and inflammation responsible for your initial symptoms.
Women athletes tend to get the most attention in concussion research because sports-related concussions impact an athlete's ability to play in addition to their effect on quality of life. But you can also sustain head trauma from a non-violent source, such as carbon monoxide poisoning, infections and viral disease, chemical treatments (like chemotherapy), and more. One patient we treated developed post-concussion syndrome from a hysterectomy! (More on that in a bit.)
On average, concussion patients recover within two weeks. But up to 30% of concussion patients have symptoms that persist for months or even years after their injury. Those symptoms stem from two issues following injury:
Neurovascular coupling (NVC) is the relationship between your brain’s neurons and the blood vessels that supply them. Concussions disrupt NVC, causing symptoms such as brain fog, headaches, mood swings, difficulty concentrating, sleep problems, and vision problems. Read more about neurovascular coupling here.
An injury or illness might also affect your autonomic nervous system (ANS). Symptoms of ANS dysregulation include headaches, changes in blood pressure or temperature, gastrointestinal issues, exercise intolerance, muscle tension, and more. Read more about ANS dysfunction (dysautonomia) here.
While a regular MRI won’t typically detect post-concussion syndrome, we’re able to pinpoint affected areas of your brain using functional Neurocognitive Imaging (fNCI, a special application of fMRI). You can learn more about how that works (and why regular MRI doesn't work) here.
fNCI is how we were able to diagnose and treat post-concussion syndrome for the woman who had a hysterectomy but no history of head injury. Her symptoms could have come from multiple causes: The hysterectomy itself likely put strain on her autonomic nervous system. But the sudden drop in sex hormones circulating throughout her body could have contributed, too.
If the idea of a surgery causing brain dysfunction sounds unbelievable, consider this: We've known for decades that changes in hormones can affect the brain. Loss of hormone signaling due to menopause, hysterectomy, or oophorectomy (removal of ovaries), etc., can increase your risk for cognitive disorders such as Alzheimers.
Research done in humans and animal models shows that the sudden loss of female reproductive organ signalling (through hormones) leads to reduced activation in frontal and hippocampal areas of the brain, which is associated with cognitive problems. These issues can be seen with fMRI. Not only this, but loss of ovaries can lead to neurovascular dysfunction and lowered BDNF levels (BDNF, or brain-derived neurotrophic factor, is a key player in healthy brain function). Interestingly, research also shows exercise can improve some of these symptoms.
So if you’ve had any physical trauma (be it a blow to the head, an illness, a major surgery ... ) and you’re having long-lasting symptoms, investigate post-concussion syndrome as a possible cause. It may not be the answer — but if it is, we can treat it.
(Note: We don’t intend this discussion to scare you or prevent you from getting a needed hysterectomy. If you need a hysterectomy, then you should get one. But when you do, look for an endocrinologist who will help your body adjust instead of going off those hormones cold turkey. And push for follow-up care if your needs [such as pain or other symptoms] are being ignored.)
Women have a higher risk of concussion from physical causes. Our neck muscles and cervical spine are weaker than men’s. That decreased neck strength and stability are what makes us more prone to injury, be it via whiplash, head impacts, or jostling. It’s the reason that women’s soccer and ice hockey are among the five contact sports that cause the most concussions every year.
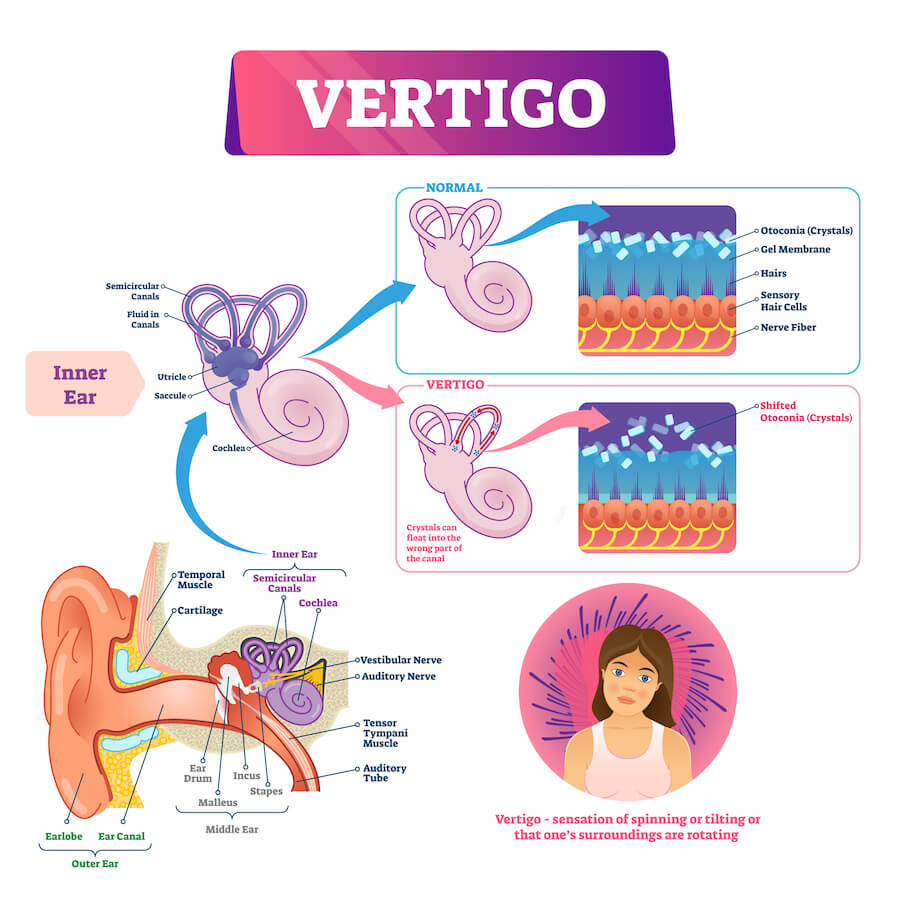
In addition, due to female physiology, physical head injuries are more likely to affect the inner ear crystals that control the vestibular system (how we balance and judge our position in 3D space). We know this because female athletes perform worse on tests of vestibular ocular reflex (VOR) than male athletes after concussion. So physiologically, it’s easier for women to get concussed than men.
Unfortunately, disruption of regular brain function and vestibular function mean we have more opportunities to develop post-concussion syndrome.
While some researchers think that the numbers are skewed due to reporting bias (many still believe that women are more likely to report symptoms and at a higher severity than men), objective measures (such as the VOR test mentioned above) still indicate higher symptom severity and increased occurrence of concussion. This leads to higher rates of post-concussion syndrome as well.
But there are more factors in play.
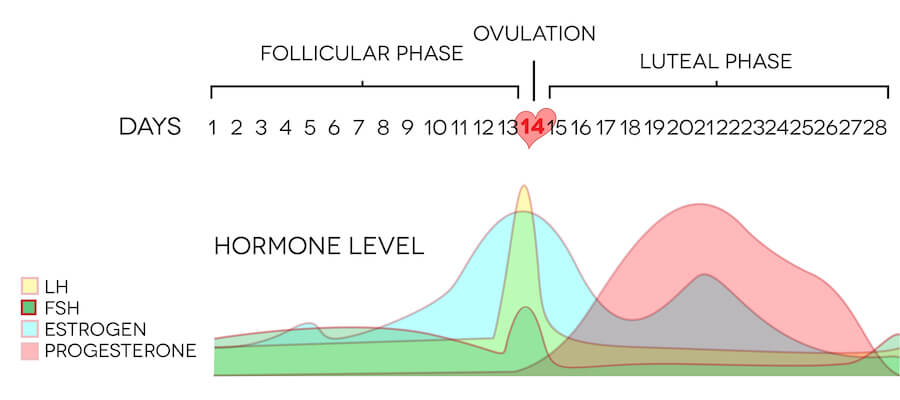
Women are at increased risk of developing PCS if their TBI happens during the luteal phase of their cycles (post-ovulation but before menstruation). It has to do with how our hormone levels change over the course of each cycle. While we need more research to understand why, it appears to be the drop in estrogen and changing progesterone levels that produce increased symptom longevity.
Early medical intervention may play a role as well. We’ve heard from many patients whose doctors either recommended rest or nothing at all in response to a possible concussion. Doctors have said things like, “You don’t have a concussion; you’re just depressed that you lost the game.” or “You’re just being emotional; you probably don’t have a concussion.” That lack of treatment might contribute to developing post-concussion syndrome.
For a deeper look into why women are at increased risk of concussion, read this article on the topic from the BBC.
Here are five common issues that women face during their recovery. Just knowing they exist will help you handle them if they arise, but we’ve also included what advice we can give for each.

Until recently, most research on the brain and concussions was done on men. Football concussions captured more attention, men’s brains are easier to study, and many doctors didn’t consider that gender differences could factor into brain injury and recovery.
The biggest issue is our lack of knowledge regarding the female brain.
The female brain is difficult to study because of our constant hormone fluctuations. Traditionally, scientists used male animal models for their research because the constancy of hormones made it easier to get predictable results. Same goes for patients in clinical trials for drugs. As of 2014, the NIH now requires the preclinical research they fund to be conducted in male and female animal models. And they’ve only been requiring female participation in NIH-funded clinical trials since 1993.
Unfortunately, that means that our knowledge of concussions, pharmaceuticals, and almost everything else in medicine is based on male physiology. So how does this headache medicine or that anti-nausea pill affect a woman’s brain? In many cases, we don’t know because sex differences weren’t studied. (Adding insult to injury, most pharmaceuticals have only been tested on neurotypical brains, i.e., not those suffering from brain trauma.)
Meanwhile, we do know there are notable differences between men and women’s brains. For example, women have different microglia than men. Microglia are cells at the frontlines of your brain’s inflammation and injury response — which means they play an important role in concussion outcomes. Shouldn’t we know more about their role in women’s concussion?
We can’t undo years of missed research. The good news is that most studies are required to have male and female subjects now. But the discipline as a whole hasn’t recovered from the dearth of research on women, which makes it harder to get good diagnoses and treatment.
Some patients have been told by their doctor, “You’re too complicated for me to treat; sorry.” The reality is that post-concussion syndrome is complicated no matter what gender you are, but female hormone fluctuations make it even harder to tease out exactly what’s happening.
If you have a doctor who can’t figure it out, keep looking. Find someone who is willing to look for a root cause instead of treating symptoms as isolated issues. Look for a provider who will order additional testing when the answer isn’t immediately apparent, consider more treatment options than just pharmaceuticals, and troubleshoot dosing and brands when you do need pharmaceutical intervention.
If you know you’ve suffered a concussion, here’s a guide on how to find a good concussion clinic near you. For young women, pediatric doctors may not have the expertise necessary to diagnose and treat lingering issues from concussion. Sports medicine doctors might be more helpful, but it depends on their specialty. Unfortunately, not many doctors understand post-concussion syndrome and how to treat it.
We hear so many stories of female concussion patients whose doctors didn’t take them seriously.
“You’re just depressed. Try this SSRI.”
“Have you tried taking a pregnancy test?”
“That’s just a stress headache.”
“You gained 20 pounds. How much are you eating every day? You need to exercise more.”
“It’s psychosomatic.”
Most doctors aren’t intentionally hostile or unhelpful. But many fixate on one or two symptoms instead of digging for the root cause. There are many reasons why women have trouble getting a post-concussion syndrome diagnosis:
This isn’t to say that all doctors are bad and treat female patients dismissively. But we’ve heard so many stories from our female patients of doctors who fail to listen and don’t provide the care that they need. It happens far too often.

It’s hard to stand up for yourself in the doctor’s office. It’s even harder if your symptoms (such as difficulty finding words or anxiety) are working against you. The best thing you can do to keep your doctor on track and accountable is to bring an advocate with you.
The best person to bring along is someone who’s known you for a long time and can compare your behavior before and after your injury (or even just before your health started declining). And as frustrating as it may be, bringing a male (such as a boyfriend, husband, good friend, father, or father figure) could get you taken seriously.
In addition, make sure you come to each appointment prepared with a list of your medications and symptoms. Write down the questions you want to ask so you don’t forget during the appointment.
If you’re still having trouble even after all these steps, try to find a female doctor: They are known to take more time with their patients. It’s possible that willingness to have a discussion will yield better outcomes (or at least a more empathetic response).
A brain injury can cause dysfunction in the thalamus, hypothalamus, and pituitary gland, all of which control hormone production. Because of that, head trauma can cause over or underproduction of hormones.
You can read all about hormone dysfunction after a brain injury here. That article covers the most common kinds of hormone imbalance after a head injury: growth hormone deficiency, adrenal insufficiency, hypothyroidism, hypogonadism, hyperprolactinemia, and antidiuretic hormone (ADH) insufficiency.
Both men and women can suffer from hormone dysfunction after a concussion. Women’s health issues that could be connected to post-injury hormone dysregulation include:
These issues often center around changes in estrogen, thyroid hormones, and progesterone. We’ve seen a number of patients whose fertility was suppressed due to a host of factors, including ANS dysregulation, post-injury stress, hormone changes, and possibly the metabolic changes associated with PCS (which could make it harder to nourish a fetus).
Note: Sometimes we’ve seen patients conceive post-treatment babies! In most cases, they had been trying to have children for years without success. Post-concussion syndrome puts tremendous stress on our bodies. In a few cases, relieving that physical and emotional stress was enough for these women to become the mommas they dreamed of becoming. Treatment for PCS is not a guaranteed fix for infertility. But it can be a missing piece.
If you’ve developed PCOS, endometriosis, or menstrual cycle changes after your injury, finding a good doctor is key. You’ll need to work with a doctor who a) understands how to diagnose and treat those issues, but also b) is either knowledgeable enough to or willing to work with someone who can also keep your brain health in mind.
For example, estrogen has neuroprotective properties. It will help your brain stay healthier, longer. But estrogen also fuels endometriosis. Should you opt for a drug that decreases estrogen? One that increases estrogen? Should you have surgery to remove the endometriosis? Or get a hysterectomy? Those are difficult questions that require working closely with a knowledgeable physician.
By the way: Testosterone isn’t just a male hormone — women need it too! If you’re having problems with any other sex hormones, ask to get your testosterone levels tested as well.

If you have any of the symptoms of hormone dysfunction, ask your doctor to test your hormone levels. Read up ahead of time, find a good doctor, and get those tests done. If you’re not satisfied with how your doctor handled the situation, shop around. Here’s a guide to finding and talking to a doctor about hormone dysfunction. You may need a team of medical professionals: someone to treat your brain injury, an ObGyn, and (possibly) an endocrinologist.
If you’re not trying to get pregnant and you have symptoms related to your cycle, many doctors will prescribe hormonal birth control. While this is a viable option, it has some drawbacks. Many women are not told about benefits versus risks and what the alternatives are. Here’s a quick breakdown so you can make an informed decision about your care:
Pros:
Cons:
Alternatives:
There isn’t a one-size-fits-all solution to these health issues. Some women will need birth control; others will do well on bioidentical hormone replacement. Some may find that dietary changes and exercise are enough to control their symptoms.
If you do need to get on birth control, realize that generics are not necessarily equivalent to name brand options; you may have to try a few different ones. It’s like SSRIs: Some people just have a really bad reaction to certain brands. For example, some women we know have side effects such as mood swings, acne, or, when they stopped taking the pill, horrible cramps during their periods when they hadn’t had those symptoms before. It may take time to find the best one for your body.
It’s also worth knowing that some hormone levels can’t be tested while you’re on the pill. If you suspect hormone dysfunction, it’s best to get those tests done before taking birth control.
In summary, know your options and have a solid chat with your doctor before making a decision.
If you’ve been suffering from symptoms connected to a possible brain injury, we may be able to help. 95% of our patients show statistically verified restoration of brain function. Schedule a consultation to discuss your symptoms with a member of our team.

Whether you’re a stay-at-home mom or juggling kids and a career, a brain injury will impact your ability to manage affairs at home. Many women still shoulder over 50% of housework and caring for their children, regardless of work status.
But that might come to a screeching halt after a brain injury. Your brain and ANS need time and space to recover, so it’s unrealistic to keep doing everything you were before. The COVID-19 pandemic makes it even harder to get that space to recover because not everyone is comfortable sending their kids to day camp, getting a nanny, etc. (and that’s if you can afford it).
If you have a significant other, have a serious discussion about who will shoulder which responsibilities so you can get the support you need to recover. You will need emotional, nutritional, and physical support. It can come from your S.O., from other family members, or friends. Don’t be afraid to ask for help when you need it.
Have a sit-down discussion with your kids (and any other household members) so they all understand what’s happening to your brain and how they can help. If your kids are struggling emotionally with the way you’ve changed after your injury, consider getting them to counseling. You might need counseling as well — post-concussion syndrome is hard on mental health!
We’ve treated many mothers. Most of their families were super supportive and excited to help once they understood what would be helpful. We send moms home with cognitive exercises they can do with their kids to make continued recovery at home a family affair.
Women are disproportionately engaged in dieting and monitoring their weight. Post-concussion recovery takes time and effort — a lot of it. And that means reprioritizing, whether it be our work, family obligations, or weight goals.
It is super important to eat enough and feed your brain the right nutrients. You might have to be OK with eating more than before, which is psychologically difficult if you’ve been in the mindset of actively dieting.

You can read our guide to post-concussion nutrition here. It’s so important to give your body the nutrients it needs to recover.
For women, it’s especially important to get plenty of omega-3’s, vitamins, and minerals. We especially recommend getting 400 micrograms of folic acid per day; it’s important for everyone’s brain health, but it’s key if pregnancy is on your agenda. If one of your symptoms is heavy periods, consider an iron supplement during your time of the month.
Women actually have a higher need for vitamins than our male counterparts! We don’t know for sure whether females will always need more vitamins, but research indicates that we metabolize them differently due to our hormones. Furthermore, getting the recommended daily vitamin intake can help prevent the development of nervous system diseases.
Very little research has been done on concussion during pregnancy. Here are a few things to keep in mind:
The only good thing about a concussion during pregnancy is that pregnancy hormones are highly neuroprotective, so that might help prevent or reduce long term symptoms from your injury.

Women face many challenges after brain injury, and the solutions to those problems aren’t always good or easy. It helps to know what’s happening so you can take action and control what you’re able to.
There is at least some good news: Male and female brains both make the same improvements in our treatment program. Yes, you might struggle to find a good provider to handle hormone dysfunction. You might struggle to get the right diagnosis. But once you start a good treatment program, your brain has a perfectly good chance at recovery: We’ve found no statistical difference in outcomes for our male and female patients.
At CognitiveFX, we take a multidisciplinary approach to PCS treatment, including neuromuscular therapy, cognitive therapy, Dynavision exercises, sensorimotor therapy, occupational therapy, and more. You can read more about our methods here
You can also read about some of the amazing women we’ve treated over the years:
Despite dismissive doctors and debilitating symptoms, they pushed forward and found the right treatment for their injuries. We hope that, like them, you will never give up on getting the care you need to feel better and pursue your dreams with vigor.
If you’ve been suffering from symptoms connected to a possible brain injury, we may be able to help. 95% of our patients show statistically verified restoration of brain function. Schedule a consultation to discuss your symptoms with a member of our team.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

Post-concussion syndrome is downright frustrating to experience. Doctors often miss it during diagnosis, and even if they do make the diagnosis, treatment methods vary considerably from clinic to...

If you notice symptoms after a concussion, it’s best not to wait to seek treatment. If you’re the type to “wait it out” and see if things get better, then we recommend waiting no longer than three...

Cognitive FX pioneers accelerated TMS protocol that reduces concussion symptoms by 63% in just three days

After a concussion or any hit to the head, you go to the doctor, and they tell you might have a concussion, but that it is no big deal because your...

Concussions can have long-term physical, cognitive, and emotional effects. Symptoms such as brain fog, headaches, and depression can last for months or years after the initial injury. When the...

If you’re struggling to recover after a brain injury, dealing with healthcare providers is often a frustrating process. Unless you have a clear, severe injury, they might be dismissive of your...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY