Can Post-Concussion Syndrome Cause Stuttering?
Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
What should you do when your concussion symptoms don’t go away?
While there’s no precise timeline for concussion recovery, most people who sustain a mild traumatic brain injury (mTBI) are usually symptom free within a few days to a few weeks after their head injury. But that’s not the case for everyone.
For some people, despite following doctor’s orders to rest and give it time, the headaches continue. The brain fog doesn’t clear up. The dizziness, light sensitivity, or feelings of overwhelm in a noisy crowd make a return to pre-concussion life impossible.
Many of the patients who come to us at Cognitive FX have told us that when their symptoms didn’t go away, their doctors kept advising them to rest for a few more months. A few months later, when their symptoms hadn’t improved, they went back ... only to be told again to “Give it a few more months.”
For some patients, those months turn into years as they go from doctor to doctor, seeking answers, empathy, and a solution.
Some patients are told there’s nothing wrong with them, even though they’re struggling with debilitating symptoms. For example, Myrthe van Boon was injured in a skiing accident and told she’d be fine after a couple of weeks of bed rest.
She wasn’t.
Myrthe came to us 13 years after her accident. Most of the health care providers she visited either said they couldn’t help or that she was making things up. Incredibly, one neurologist she visited even said, “You just like to be taken care of,” and told Myrthe she would get better when she decided to get better.
While Myrthe did see a neurologist before coming to our clinic, many others suffering from persistent symptoms haven’t. If you’re looking for help beyond the endless “rest some more” advice cycle, you might be wondering: What can a neurologist do for post concussion syndrome (PCS)? Could a neurologist help?
It’s a reasonable question. A concussion is a brain injury, and neurologists deal with the brain.
While you definitely want to consult a neurologist if you have a stroke or symptoms of a neurodegenerative disease, such as Alzheimer’s or Parkinson’s, they might not be the best choice to help with post-concussion syndrome.
The results of a survey of 289 neurologists attending a 2017 Texas Neurological Society meeting demonstrate this. The participants were asked to agree or disagree with various statements relating to PCS. The majority of neurologists who responded said they didn’t believe effective treatment was available for post-concussion syndrome.
If they don’t know about treatment options for post-concussion syndrome, let alone practice those methods themselves, then the ways they can help you are limited.
Note: There is an effective treatment protocol for post-concussion syndrome, and we’ll talk about it later in this post. If you want to skip straight to treatment information, click here.
In this article, we will explore what neurologists do and what someone with a mild or moderate neurotrauma can expect from seeing a neurologist. We will cover:
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, sign up for a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.

A neurologist is a medical doctor who specializes in disorders of the brain and nervous system, such as Alzheimer's disease, multiple sclerosis, epilepsy, Parkinson’s disease, and stroke.
The education required to become a neurologist is extensive. A student must complete a four-year university degree, medical school, a one-year residency in internal medicine, and then at least three years of a specialized residency in neurology. They must then pass a written exam to become board-certified by the American Board of Psychiatry and Neurology. Many neurologists continue their education in an even more specialized area of neurology, such as vascular neurology, neuroimaging, or geriatric neurology.
Neurologists diagnose, treat, and manage diseases and disorders of the nervous system. They use many tools to diagnose and manage these conditions, such as brain scans, genetic testing, cerebrospinal fluid analysis, and blood tests. They perform neurological examinations in which they examine motor skills, balance, vision, speech, sensory function (smell and touch), and cognitive function, among other things.
Neurologists can also prescribe medicine, order rehabilitation, and refer patients to other specialists.They do not perform brain or spinal cord surgery.
A patient might initially encounter a neurologist if there’s any possibility they’ve sustained a traumatic brain injury (TBI).
For example, if they’ve been in a car accident, had a bad fall, or had a serious sporting injury and are experiencing symptoms such as loss of consciousness, bleeding, seizures, or vomiting, then their injury warrants a trip to the emergency department (ED). A neurologist might be called in to examine the patient and to determine the severity of the injury.
However, not all incidents that cause a concussion call for a trip to the ED. It’s more typical for a patient to go to an urgent care facility or to their family doctor within a day or two of the injury. They might never see a neurologist unless their doctor refers them to a specialist.
If a patient does see a neurologist after head trauma, the neurologist will perform a neurological exam — checking mental status, speech, balance, reflexes, and vision for indications of a mild TBI or a more severe brain injury.

The neurologist might order a computerized tomography (CT) scan to check for skull fractures or bleeding that could become life threatening and require surgical intervention. Concussions, however, can’t be detected by a CT scan or a regular MRI because those tests only show structural damage, which is not the type of damage a concussion causes in the brain.
Unfortunately, most neurologists have very little training in treating acute concussions beyond the initial injury assessment. However, there are some neurology specialists who are more familiar with concussions, including sports neurologists.
The field of sports neurology is a relatively new and growing specialty. It’s becoming more common for sports neurologists to be on the staff of sports medicine practices or on the sidelines of athletic events — especially contact sports events — thanks to the increasing awareness of the danger of concussions from sports injuries in recent years.
So while it’s uncommon for patients to see a neurologist for a concussion, what about when the symptoms just won’t go away?
As we noted earlier, many people suffering from post concussion syndrome endure months and even years of living with persistent symptoms of concussion. They often go from doctor to doctor seeking help for symptoms such as frequent headaches, difficulty concentrating, memory problems, dizziness or balance issues, sleep disturbances, and chronic pain. These are all compelling reasons for consulting a neurologist.
If you decide to see a neurologist for post concussion syndrome, here are three things they might do:
A neurologist can rule out alternative causes of your symptoms.
They can order imaging to see if there’s evidence of any other undiagnosed problem within the brain. A CT scan could detect evidence of a previously undiagnosed skull fracture, bleeding, a brain tumor, or evidence of a stroke. An MRI of the brain or spine could detect excessive fluid, any malformations within the brain, a brain tumor, an aneurysm, or even evidence of dementia.
The neurological exam and other tests, such as blood and genetic tests, could also indicate other neurological disorders that might cause some of the same symptoms.
A neurologist can prescribe medication to manage neurological conditions such as pain, nerve issues, and neuromuscular disorders, including migraines and persistent headaches.
Medication is a mixed bag: For some conditions, like post-traumatic migraines, it can significantly increase quality-of-life. But it’s not a solution for every concussion symptom. Medication often comes with unpleasant side effects that can affect your future health. It’s a complex balancing act between the possible symptom relief and the detrimental effects of the medication.
If, after a thorough exam and testing, the neurologist sees the need to refer you to another specialist, they can provide that referral. For example, a patient suffering from dizziness or balance issues might be referred for vestibular rehabilitation therapy. Someone experiencing light sensitivity and/or eye tracking problems might be referred for vision therapy.
As with medication, however, these individual therapies may help with one symptom, but they might not treat the underlying cause of the symptoms you’re experiencing if they are from a concussion.
Ultimately, there’s very little a neurologist can do for postconcussive syndrome besides managing some of your symptoms with medication.
The authors of a Practical Neurology article about concussion admit that even though neurologists know some concussion symptoms can linger for years, most neurologists assume the symptoms are “benign” and that they will eventually resolve over time. They don’t really have any treatment options and instead try to reassure patients their symptoms aren’t harmful and will eventually go away on their own.
As you’re likely aware, this isn’t a satisfying answer. Post-concussion syndrome isn’t harmless: the symptoms can keep you from work, socialization, and even family life if they’re bad enough.
The good news is that many neurologists are starting to research concussion mechanisms, diagnostics, and treatment in academic research or in collaboration with treatment clinics like ours. Just because many neurologists don’t know how to treat post-concussion syndrome effectively at the moment doesn’t mean they won’t a few years from now.
In the meantime, we’ve made significant strides in understanding and treating post-concussion syndrome. In the next section, we’ll explain what causes lingering concussion symptoms and what you can do to start recovering.

At Cognitive FX, we’re not going to tell you your symptoms are imaginary or that you have to wait it out any longer. We’ve successfully treated thousands of patients with PCS from all over the United States and around the world. And while we can’t guarantee you an immediate, 100% end to all of your symptoms, we can tell you that 95% of patients who complete our Enhanced Performance in Cognition (EPIC) Treatment program show statistically verified improvement of brain function.
How do we know that? Through the results of patients’ pre- and post-treatment fNCI scans (we’ll explain what those are below). The average patient’s improvement after one week is 77.5%.
Our unique, multidisciplinary treatment program is designed to find and target the source of each patient’s post concussion syndrome symptoms. Our active rehabilitation method leverages the brain’s natural neuroplasticity, which is the ability of the brain to change, grow, and form new connections.
In this section, we’ll explain what causes post-concussion symptoms, how we image patients’ brains, and how we approach treatment.
To understand how treatment works, it helps to understand what happens inside the brain after an injury.
A concussion happens when the soft tissue of the brain crashes into the skull. The impact of the brain against the skull can cause minor swelling, bruising, and localized nerve cell damage. While this damage isn’t life threatening, it disrupts the normal brain function.
Neurovascular coupling is the connection between neurons (brain cells) and blood vessels. When an area of the brain needs to perform a task, the neurons in that area call for a specific amount of oxygen at just the right time to get the job done. Dysfunction of this efficient call and delivery system is what’s behind most concussion symptoms.
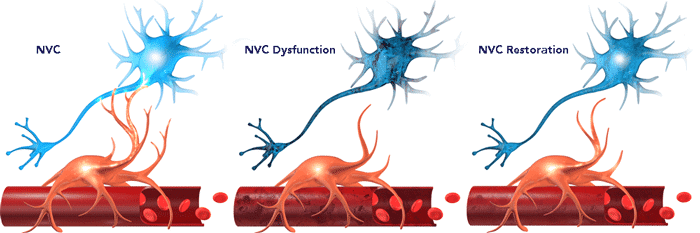
This dysfunction results in some areas of the brain being unable to properly do what they’re trying to do, or in others, working overtime to try to compensate for the struggling areas. For you, this scenario might result in symptoms such as a recurring post-traumatic headache or the inability to read a sentence and remember what you just read.
The goal of our program is not merely management of concussion symptoms but to identify exactly where this breakdown is occurring and push the brain to return to healthy neurovascular coupling.
Standard MRIs can’t see evidence of dysfunctional neurovascular coupling, but a functional MRI (fMRI) is more useful. An fMRI can see and map blood flow in the brain as it responds to cognitive demands. We use this technology to take images of the brain as a patient performs a series of very specific cognitive tasks, a process called functional neurocognitive imaging (fNCI).
Using fNCI, we’ve developed an extensive database of images from people who have and have not had a brain injury. By comparing our patients’ neurovascular coupling to the normative spread, we are able to see biomarkers that indicate which areas of the brain are experiencing neurovascular coupling dysfunction. Dysfunctional areas have either too much or too little blood flow to specific areas for the task they’re trying to do. This tells us exactly which areas of the brain to target for treatment.
In addition to the fNCI, every patient gets a standard structural MRI of the brain and cervical spine. We want to be sure there are no underlying, undiagnosed conditions that could be causing problems or that might interfere with treatment. We have a neurosurgeon on our team who can assess any issues that come up in these scans, and we refer patients to the proper specialists when necessary.
Now that we’ve explained what causes concussion symptoms and how we use fNCI to pinpoint the dysfunctional areas behind them, we’ll describe what treatment at Cognitive FX looks like.
Before you even arrive, we communicate with you about how to prepare for your treatment at Cognitive FX. For example, we encourage patients to slowly increase their physical activity and learn measured breathing techniques. Our treatment is very active, and some patients have referred to it as “boot camp”. Many of our patients are on multiple medications. We’ll discuss these with you and let you know if you need to taper off any that could interfere with treatment.
Our treatment team includes a neuropsychologist, a neuroscientist, a neuroradiologist, a psychologist, neuromuscular therapists, neurocognitive therapists, neurological occupational therapists, and others. All of these specialists work together to create an intense, individualized treatment regimen based on your fNCI results and the specific symptoms you’re experiencing.
 A therapist prepares a patient for eye testing.
A therapist prepares a patient for eye testing.
You’ll begin each therapy session with cardio activity to stimulate blood flow to the brain. (Many of our patients suffer from exercise intolerance. If that’s you, don’t worry. We’ll help you through all cardio and physical therapy.) After cardio, you’ll go through a mix of neuromuscular, cognitive, occupational, sensorimotor, and vision therapies — all designed to target your specific areas of injury.
Treatment usually runs from Monday through Friday, with the most intense days occurring on Tuesday through Thursday. Monday is usually an introductory day. You’ll get a tour of the facility, meet the staff, and start therapy. Therapists will work one on one with you to assess your specific abilities and needs to serve as a starting point. They will constantly monitor and modify therapies throughout treatment as you progress.
Some patients come to us after having gone to other concussion clinics and done some of these therapies in isolation with limited (or no) success. Cognitive FX combines therapies in a way that other clinics do not; this multidisciplinary approach is more effective at helping the brain use healthy neural pathways.
One of our patients, Sam Pembleton, had been exposed to some of these therapies without success at other clinics before coming to Cognitive FX. She explained, “The biggest difference was, at Cognitive FX, they were doing a bunch of different treatments at the same time, working different parts of your brain all at once.”
She gave this example of a session that challenged her in particular: “It was an hour-long therapy, and it was just one on one with someone. You’d do a cognitive activity, like sorting through a deck of cards, but at the same time someone would give you a four-letter sentence and you'd have to arrange it alphabetically while you were still sorting through the cards. It was a lot of multitasking!”
 A patient receiving instructions on how to use the Dynavision board.
A patient receiving instructions on how to use the Dynavision board.
Another example is therapy using the Dynavision board. Dynavision therapy uses a board that lights up in varying patterns and speeds. Patients touch the lights as they illuminate. This therapy helps with visual field deficits, eye-hand coordination, quick response times, and more.
Chris Nicastro described his experience of Dynavision therapy during his EPIC week. “You stand on the Bosu ball, and you have to hit the lights when they light up, but you're doing things like reciting the alphabet backwards and all this crazy stuff at the same time. It's hard. Your body and your brain are a lot more powerful than people give them credit for,” he reflected. “You can do something like that and push your brain to the point where it rewires.”
During treatment, you’ll also spend time learning mindfulness, relaxation, and proper breathing techniques. Many patients enjoy the quiet time they spend listening to Brainwaves. Writing about her week at Cognitive FX, Aimee Francom said, “My brainwave time was my favorite! I loved being forced to relax. I’m a Type A personality and don’t relax enough. Falling asleep was an option I looked forward to as well, though I never actually napped.”
Patients also meet with our psychologist during their time with us. She checks in on patients as treatment progresses to evaluate any emotional difficulties they’re experiencing.
At the end of treatment, every patient goes through another complete fNCI. We compare the pre-treatment and post-treatment fNCI results to measure the amount of improvement that happened.
We provide patients with a comprehensive report detailing the performance of sixty brain regions during testing. Patients also receive an overall score of the brain’s performance in comparison to a healthy brain. We call this report the Severity Index Score (SIS).
Zero is the mean severity score for a non-injured brain, while 2.5 is the mean severity score for concussion patients. We shade areas of the chart to make it easier to see a range of standard deviations from the norm (+/- 0.75). Green can be within the normal range, yellow indicates moderate impairment, and red indicates a severely struggling brain.
Here’s a look at Myrthe van Boon’s before and after SIS scores:
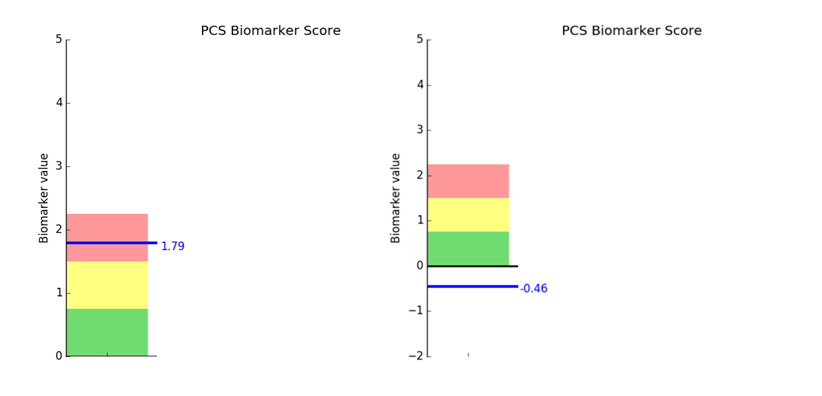
The chart on the left shows her pre-treatment SIS score. She was clearly in the dysfunctional red zone at 1.79. On the right is her post-treatment score. It’s actually below 0, but it’s within the standard deviation at -0.46, so it’s perfectly normal.
Myrthe’s before and after scores are typical of what we see every day in our clinic. Over 77% of our patients see improvement of between 60-100%, and 43% improve between 80-100% on the Severity Index Score (SIS).
Even better, patients also report a significant reduction in symptoms by the end of treatment — 60% improvement in one week on average. (Check out the Patient Stories on our website to hear first-hand accounts from some of the patients who have been through EPIC Treatment.)

EPIC Treatment isn’t a magical cure for PCS. Recovery takes work. It’s a process. For the most improvement, you’ll need to keep working hard at home after treatment.
We give you the tools to do that during your time at Cognitive FX. We teach you how to do specific exercises that you can do at home. Then, we give you an individualized post-treatment plan to follow week by week.
A typical post-treatment plan includes at least 30 minutes of some cardio exercise daily, plus a few cognitive exercises that we’ve taught you how to do. Some patients are advised to seek additional therapy, such as vision therapy or psychological counseling. We can help connect you to professionals in your area of residence.
During the first six months after treatment, we’ll periodically check in with you, answer your questions, and suggest alterations to your homework if you encounter any problems. And patients can always call or email if they have concerns or questions after treatment.
Read the linked post if you’d like more information about recovering from post concussion syndrome after treatment.
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, sign up for a consultation.

Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.

Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...

After suffering a mild traumatic brain injury, you might expect to feel off for a few days before being able to function at your normal level again. However, a rapid return to normal is not the case...

If you’ve suffered a concussion, you may have already encountered the Post-Concussion Symptom Scale (PCSS). This self-report questionnaire is one of the most widely used tools for documenting...


Post-concussion syndrome (PCS) is a complex condition in which concussion symptoms persist for weeks, months, or even years after the initial head injury. While most people recover from a concussion...

Recovering from post-concussion syndrome (PCS) is challenging, but with the right guidance, substantial progress and symptom relief are possible, even years after the initial injury.
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY