Brain Injury and Exercise: How Cardio Intervals Help Patients Recover

If you’ve been struggling with lingering symptoms after a brain injury and even a mild jog is enough to trigger misery, then you might flinch at the idea of high-intensity interval training as a recovery method. But there is a way to exercise while keeping your symptom levels down.
At our clinic, Cognitive FX, physical activity is not just about fitness: It’s a vital part of the treatment we offer patients with persistent post-concussion symptoms (PCS).
If you’re not sure what this means, read our complete guide to post-concussion syndrome.
This same approach works for survivors of moderate to severe traumatic brain injury (TBI), transient ischemic attack, chemotherapy, long-term COVID-19, and other causes of brain dysfunction.
Why does it work for different types of acquired brain injury? Because all of these conditions disrupt healthy oxygen flow in the brain by damaging the connection between neurons and blood vessels. As a result, some parts of the brain function less than they should, while others take on the extra load. This is known as neurovascular coupling (NVC) dysfunction. In practical terms, we measure this dysregulation with a special type of brain scan: functional neurocognitive imaging (fNCI). fNCI spots problems with blood flow in the brain and helps us see areas of higher or lower activity.
To effectively treat PCS, we must restore healthy neurovascular coupling throughout the brain, re-establishing healthy cognitive function in the areas highlighted by fNCl. To achieve this, we’ve designed a treatment plan known as EPIC Treatment, which combines a series of physical and cognitive exercises to coax the brain to engage in specific activities. All this is customized to each patient’s brain and symptoms.
Therapy follows a pattern of Prepare, Activate, Recover:
- Prepare: As preparation for cognitive therapies, patients undergo short bursts of intense cardio to encourage healthier blood flow in the brain. Exercise also generates a boost of crucial neurochemicals in the brain as well as affecting the autonomic nervous system (ANS).
- Activate: Both mechanisms promote the brain’s ability to heal prompted by the right stimuli coming from different types of therapies, including cognitive therapy, sensorimotor therapy, massage therapy, neurointegration therapy, and more.
- Recover: Finally, we build in periods of rest and relaxation throughout the day so the brain has time to recover before the next round of therapy.
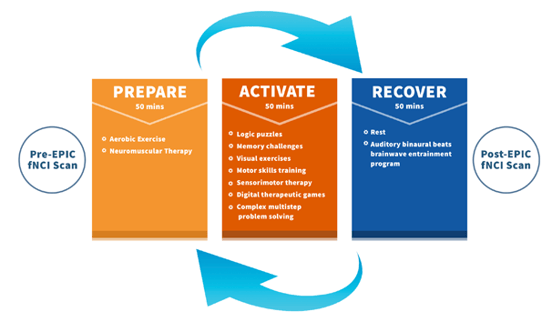
By repeating this sequence throughout treatment, patients’ healthy neurovascular coupling is restored, which in turn reduces the incidence of concussion symptoms lingering after a mild traumatic brain injury.
At the end of treatment, patients receive a set of exercises to do at home to keep the momentum started during their EPIC treatment. These are designed not only to improve fitness and wellbeing in general, but most importantly to continue their recovery in the months ahead.
On average, our patients improve by 77% during their week of treatment. That improvement is due to a combination of the therapies as a whole, but it would be a lot lower without the aerobic exercise component.
In this post, we’d like to explain why aerobic exercise is so important to treatment. We share the two key benefits of cardio on post-concussion syndrome recovery, along with why it’s so important for us to monitor patients while they exercise in the clinic.
If you have lingering symptoms from a concussion, you’re not alone. As many as 30% of concussion patients do not recover without treatment. 95% of our patients experience statistically verified restoration of brain function after natural therapy at our clinic. To learn if you’re eligible for the program, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
Benefit #1: Exercise Boosts BDNF and Promotes Neuroplasticity
Every time you exercise, you get a boost of essential neurotransmitters and proteins along with improved blood flow in the brain. All of those neurochemicals are helpful, but one is especially important for patients struggling with brain trauma: Brain Derived Neurotrophic Factor (or BDNF for short).
Scientists used to think that once we stopped growing, our brain would lose the ability to change and adapt. It turns out, this is not the case at all. The brain can adapt, grow, and change in the face of even severe head injuries. This ability to adapt is known as neuroplasticity, and BDNF is a key player in this process.
In practical terms, BDNF can promote the growth of nerve cells as well as stimulate communication between cells in the brain in response to a particular experience. This can alter neural function and modify thoughts, feelings, cognition, and even behavior. BDNF also helps to regulate the autonomic nervous system (which we’ll discuss more in the next section).
What’s incredible about BDNF is how much control we have over its levels. There are many factors that directly regulate how much BDNF is released in the brain — if you know how to control these, then you can directly improve your brain’s ability to adapt when needed.
Physical exercise is by far the fastest and most efficient way to increase BDNF levels. It doesn’t matter if you’re an elite athlete or an absolute beginner, you always get a BDNF boost after exercise. If you engage in regular exercise — adjusted to your own abilities, of course — even your resting BDNF levels (the amount circulating in your brain even when you haven’t just exercised) will increase over time.
To maximize these BDNF boosts during brain injury rehabilitation, we’ve found that short bursts of intense cardio are the best option for our patients. It’s a win-win situation: Not only is high-intensity aerobic exercise much better than continuous moderate intensity exercise to stimulate BDNF, but larger muscles (such as the quadriceps in the legs) provide a larger BDNF response. Most of our patients achieve this via intervals on a stationary bike or treadmill during treatment.
Since BDNF promotes neuroplasticity, increasing it helps make therapy more effective. During treatment, our patients engage in a cycle of cardio exercise, cognitively challenging therapies, and rest. This pattern helps the brain get the most out of treatments such as cognitive therapy, sensorimotor therapy, neurointegration therapy, and more.
Sometimes, we also guide patients through cardio at the end of the treatment day to help them feel better as they wind down after a long day of treatment.
Benefit #2: High-Intensity Intervals Help Regulate the Autonomic Nervous System

If you’ve tried to exercise but found it virtually impossible, you’re not alone. It’s a common symptom for many brain injury patients. Nausea, dizziness, or headaches during exercise could mean some exercises are not suitable for you at this stage. Even if you feel fine while out on a jog but experience brain fog or extreme fatigue a few hours later, the type or intensity of exercise you’re doing may be responsible for these symptoms. The symptoms can be so unpleasant that most people with PCS just avoid exercise altogether.
Concussions alter the way your nervous system works. Traumatic brain injuries can cause visible injuries such as bruising and damage to the blood vessels, but they can also cause a type of damage that is harder to see: dysregulation of the autonomic nervous system (ANS).
The ANS controls body processes that occur without conscious effort, such as heartbeat, blood flow, breathing, and digestion. It contains two anatomically distinct sections: the sympathetic (SNS) and the parasympathetic (PNS) nervous systems, which have essentially opposing roles.
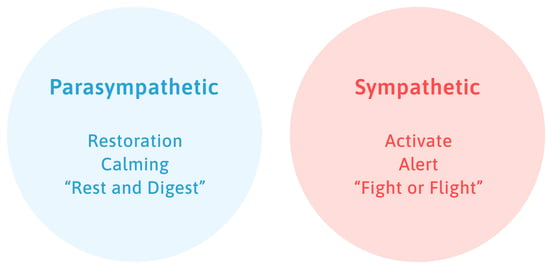
The sympathetic nervous system is often considered the “fight or flight” system. It is a quickly responding system that mobilizes the body for action by releasing the stress hormone cortisol and increasing heart rate.
On the other hand, the parasympathetic nervous system is often considered the “rest and digest” or “feed and breed” system. It has the ability to dampen responses, such as slowing down heart rate and returning to normal levels after a stressful episode.
In a healthy person, the two halves of the ANS balance each other throughout the day. For example, the sympathetic system dominates while you’re running, but when it’s time to calm down, you need the parasympathetic system. These adjustments are key to your wellbeing.
However, after a brain injury, the SNS is often stuck in a state of overreacting. To counteract this sympathetic dominance, the team at CFX developed a series of short intervals of cardio and breathing exercises based on scientific research to encourage the parasympathetic to become active. These exercises retrain the brain so that eventually, both the PNS and SNS are able to respond to the needs of the moment rather than being “stuck” with one or the other in control. It also strengthens the connection between heart and lungs (cardiorespiratory system), which is closely connected to the ANS.
So what does that look like in clinic?
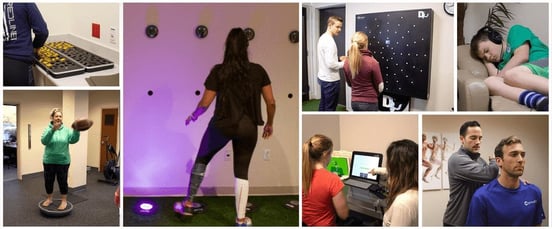
Cardio exercises: This involves short bursts on a stationary bike or treadmill, with intensity and duration adjusted to each patient. Aerobic activity is key to raise the heart rate just enough to benefit the brain through BDNF but without increasing symptoms. Finding the right amount of cardio — enough to boost BDNF and engage the nervous system, but not enough to cause severe symptoms — is difficult for many patients, which is one reason it’s important to learn from an experienced physical therapist. In this controlled environment, patients are safe and can endure intense cardio sessions to restore ANS function. It’s important to note that this does not mean the same intensity and frequency should be attempted after treatment.
Breathing exercises: After a burst of cardio, patients immediately sit down and begin breathing according to a set pattern. We often use a 4-6-1 pattern: Breathe in for four seconds, breathe out for six seconds, and hold for one second before repeating the pattern. Meanwhile, therapists are monitoring each patient for signs of the PNS activating. If it does not, they might introduce other techniques, like certain types of gargling (this stimulates the vagus nerve, which is a key activator of the PNS).
Why Do Therapists Need to Monitor You during Cardio Training?
As stated earlier, exercise is a crucial part of treatment. However, the way in which physical activity is used to coax the brain out of its “flight or flight” mode is not the same for every patient.
This is why our in-house treatment is tailored to each person based on their medical history, symptoms, physical evaluations, and MRI scans. We identify exactly which parts of the brain are not working correctly and develop a treatment plan that gets to the root cause of the dysfunction, instead of just treating isolated symptoms of a concussion.
That doesn’t mean treatment is without difficulty, however. Some patients experience a resurgence of old symptoms or increased intensity of symptoms during cognitive and physical therapy. Therapists know how to adapt your sessions based on how your brain and body react to treatment. Having a trained therapist with you is the best way to ensure you can recognize what’s happening with your body. It’s not just somebody teaching you cardio training.
For example, one aspect many patients struggle with is how to regulate their breathing. Some patients find it difficult to follow a 4-6-1 breathing rhythm. They hold their breath or breathe rapidly and shallowly. Because of their brain injury, many patients don’t even realize they are not breathing according to the recommended pattern. Therapists can notice the difference, however, and guide patients through the exercise when they struggle.
Patients also have their heart rate closely monitored. Patients need to achieve a high enough heart rate during the cardio interval, then have their heart rate come down low enough to start the cycle over again. How quickly the heart rate returns to normal is an indicator for the therapists to monitor nervous system activity.
Some patients experience a sudden drop in blood pressure and increased nausea when the PNS steps up. Therapists will monitor their condition and help them stabilize before the next set of exercises. Many patients find that subsequent cardio sessions are less and less difficult as they progress through treatment and as the balance between SNS and PNS is restored.
Our therapists also ensure that your exercises are not interfering with other areas of the brain, such as the vestibular or the visual tracking system. Some patients may need vestibular warm-ups before their cardio sessions, while others need to focus on a particular point (such as a big letter on the wall). After a few sessions, therapists can assess when it’s time to remove these extras, but only when they can see that communication between the brain, the vestibular system, and the visual system has improved.
One of our goals is for a patient to learn enough about their body’s response to cardio to the point that, by the end of treatment, they can go through cardio sessions without a heart monitor. This exercise training is the perfect way to practice for when they leave the CFX clinic and go back home.
But during treatment, therapists are essential to make sure patients are doing the exercises they specifically need in the way that they need. This ensures that not only are they recovering, but they’re also not inducing symptoms from doing the exercises incorrectly or at the wrong pace.
Pushing for Recovery

Rewiring the brain is not always a pleasant process. Therapy is hard work and produces rapid changes in the brain. These changes are good, but they may come with a temporary increase or change in symptoms. Though it may seem counterintuitive, aerobic exercise will actually help reduce these unwanted symptoms and help your brain better tolerate treatment.
Going through cardio at Cognitive FX teaches you how to exercise the most effectively for your body and injury so that you can get the most out of treatment and continue improving your quality of life at home. If you’ve tried to exercise and struggled with dizziness or headaches, that doesn’t mean you should stop exercising. It just means you need the right treatment and a better understanding of how to exercise safely. Then you can not only boost your recovery but also gain the many other benefits of exercise (such as cardiovascular health, improved mental health, and more).
If you have lingering symptoms from a concussion, you’re not alone. As many as 30% of concussion patients do not recover without treatment. 95% of our patients experience statistically verified restoration of brain function after natural therapy at our clinic. To learn if you’re eligible for the program, schedule a consultation.

About the author
Dr. Alina Fong, Ph.D.Alina Fong, Ph.D. is a clinical neuropsychologist and the Clinical Director and Co-Founder of Cognitive FX. She earned her Ph.D. in Clinical Neuropsychology with an emphasis in Neuroimaging from Brigham Young University, where she received the American Psychological Association Division 40 Graduate Student Research Award for her neuroimaging research. Dr. Fong has over 17 years of clinical experience treating traumatic brain injury, beginning with her work at the VA Salt Lake City Healthcare System and Utah Valley Regional Medical Center, where she directed the neurotrauma rehabilitation and sports concussion clinics. She developed the EPIC Treatment protocol and has personally overseen treatment for nearly 8,000 brain injury patients, including professional athletes from the NFL, NHL, and Olympics. She serves as Vice President of the Brain Injury Alliance of Utah, sits on the board of the United States Brain Injury Alliance, and advises PINK Concussions. Dr. Fong has authored peer-reviewed research on functional MRI and concussion treatment and has presented at over 60 medical conferences, including the Federal Interagency Conference on TBI and the American Medical Society for Sports Medicine.


.png?height=175&name=childhood%20head%20injuries%20(11).png)

.png?height=175&name=image2%20(5).png)



