There is a whole world of hurt and pain for patients who experience mental health symptoms after a concussion. Not all of them realize that concussions can cause anxiety, and those who do know it don’t know why it’s happening or how to fix it. Many visit psychiatrists who prescribe medication that may just make things worse (something we’ll explain in depth later in the post).
So first of all, we see you. We see your suffering and we want you to know that you’re not “all wrong.” Anxiety is a common response when the body experiences trauma from a concussive event, especially if your symptoms aren’t resolving quickly.
Over 80% of the patients we see at our post-concussion clinic in Provo, Utah report at least one emotional symptom; anxiety and depression are the most common. In this post, we’ll review…
Post-concussion anxiety is real, as are many other frustrating post-concussion symptoms. Read on to learn why this is happening to you ... and how to get help.
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion, we can help. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, sign up for a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
What Post-Concussion Anxiety Feels Like
Anxiety is an internal state of nervousness and restlessness often accompanied by ruminative or repetitive worrisome thoughts and a hypervigilant/hyperaware state. That’s a bit of a mouthful, so here’s what the symptoms of anxiety feel like for someone experiencing them:
- Feeling like you can’t relax
- Feeling like you can’t stop worrying
- Worrying about worrying
- Constantly imagining how something can go wrong (‘What if ... ?’ thinking)
- Difficulty falling asleep (because of worry)
- Feeling uncomfortable and being unable to fix it
- Feeling tense, such as tight shoulders or stomach knots.
You may also (or alternatively) experience situational anxiety or overstimulation after a concussion. For example, you might dread going to the grocery store because you always get overwhelmed or feel bad because your concussive symptoms flare.
In contrast, some patients experience sensations such as unprompted panic, a racing heartbeat, dizziness, fear about something they can’t explain, and so forth.
Both of those difficulties — worrying about places or activities you know will trigger your concussive symptoms, or an inexplicably strong fear response — may not actually be anxiety per se but can be mistaken as such. In the next section, we’ll explain what causes each and how to tell the difference between them and classic anxiety.
Why Do Concussions Cause Anxiety in Some Patients?
Anxiety after a concussion (also known as mild traumatic brain injury, or mTBI) typically comes from overactivation of the anxiety system, which is part of how our bodies respond to perceived threats. We’ll explain how that system works and then talk about how concussions can mess things up.
Fear, Anxiety, Anger: The Three Ways Our Bodies Perceive Threats

Our bodies have what you might call a threat response system. That system has three prongs: fear, anxiety, and anger. Everyone has it because it’s designed to protect us; we all have instinctual reactions to perceived threats.
The fear prong handles our response to threats in the present moment. It’s the system that urges you to run for your life when a bear jumps out of the bushes. Because it’s designed for immediate, rapid action, the fear response results in physiological (i.e., bodily) changes such as increased heart rate, rapid breathing, or clammy palms.
The anxiety prong handles potential future challenges, working to prepare us for dangers we might face. The physiological changes are accordingly subdued compared to the fear response. You might experience anxiety as tight neck muscles, some stomach discomfort, or a clenched jaw. You’ll likely experience ruminative thinking or worry as you probe through scenarios that could arise.
The anger prong, like the fear prong, is usually a response to a present situation but could be a response to something that happened in the past. Anger is how your body responds when you feel violated or offended. It’s preparing your body to fight or stand your ground rather than run away. Some physiological effects include muscle tension in the arms, hands, and jaw; flushing; or heat. You may have thoughts about injustice or wanting to right a wrong.
Two Ways Concussions Promote Anxiety
Anxiety is a secondary condition that can stem from concussions, meaning it doesn’t result directly from brain injury. As far as we know, there isn’t a mechanical or chemical failure behind most post-concussion anxiety or other post-concussion psychiatric disorders. But concussions can prompt our anxiety system to over-activate, sometimes leading to generalized anxiety disorder.
Think of your anxiety system as being on a gradient (such as a scale from 1-5 where 1 is the fear state and 5 is totally relaxed). A normal state for most people would be a 4 or a 5.
Let’s say, for example, that a psychologist is sent to a war zone to work with the troops stationed there. She would be more alert and perhaps on edge. She might, without even noticing her own behavior, start scanning rooftops for signs of snipers, or flinch if someone with a big trench coat approached. Her anxiety system’s level would increase because of a perceived increase in potential threats.
Now, what would happen when she returns to her hometown? She might gradually return to a less heightened state of vigilance, but it wouldn’t happen overnight. It would take time for her system to settle down. But for some people, that system doesn’t settle down; it keeps worrying about possible threats, even when the initial threat it responded to subsided.
If that state of preparedness and worry is persistent and severe enough, it becomes a generalized anxiety disorder. While any traumatic situation or event can trigger your anxiety system to over-activate, it’s more likely the more traumatic or unexpected the injury or event was. Even if you brushed off your concussion as a mild head injury, it is certainly capable of producing that increased anxiety response.
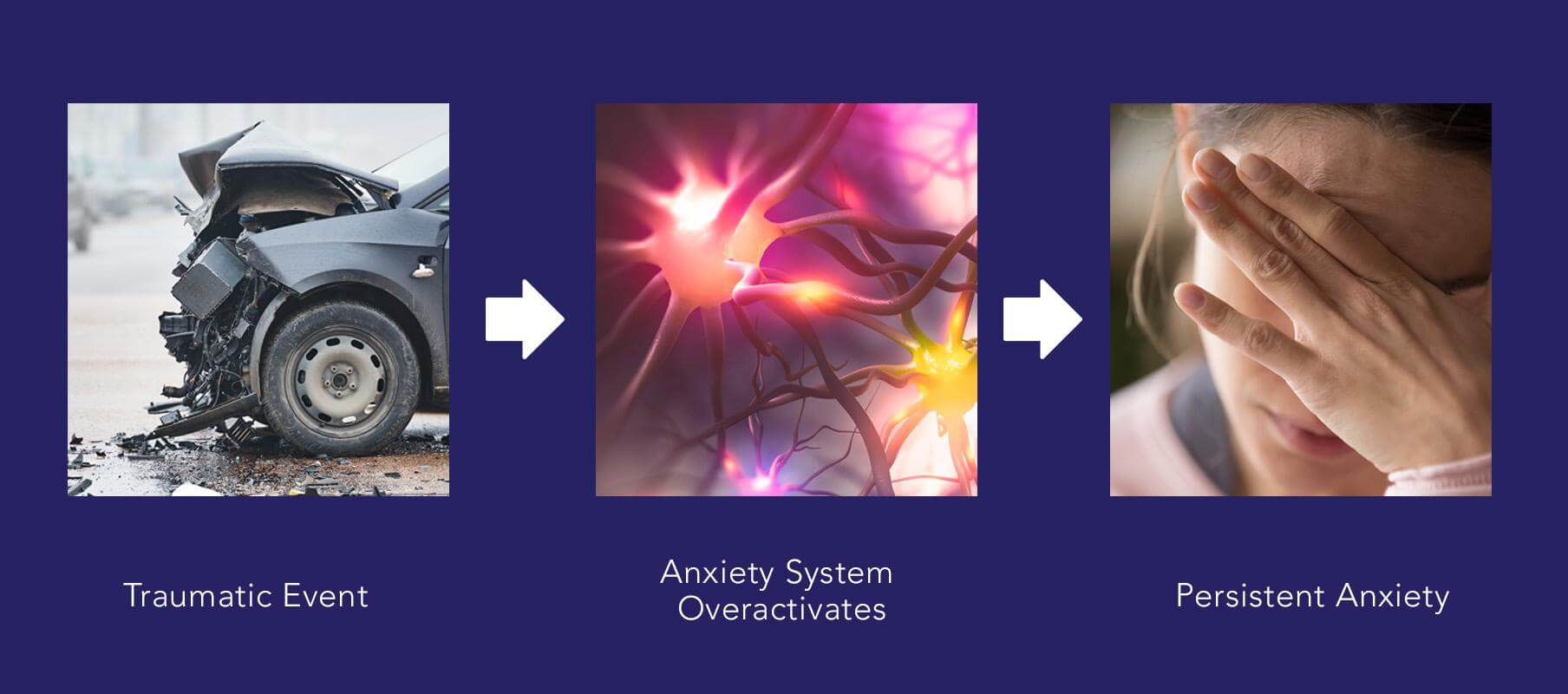
The second way patients may develop anxiety after a concussion is when they have post-concussion symptoms that don’t go away with time. These symptoms can make everyday life significantly more challenging. Additionally, you have to continually assess what you can do and how you can do it, and that ends up engaging the anxiety system more frequently than before. So it can become overactivated with time.
Finally, patients might also develop an anxiety reaction to the symptoms themselves. Headaches, vision problems, balance issues, sleep disorders, etc. are stressful and can lead to worry.
It’s not uncommon for a patient to experience some combination of the three causes we mentioned above.
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion, we can help. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, sign up for a consultation.
Is It Anxiety, Dysautonomia, or Overwhelm?
Many patients are confused by their symptoms and looking for the right words to describe their experience. Sometimes, they confuse their experiences for anxiety when there’s actually something else going on.
Two conditions that are easy to confuse with anxiety are autonomic nervous system (ANS) dysregulation (also known as dysautonomia) and feelings of overwhelm.
ANS Dysfunction: Dysregulation of the Fear Response
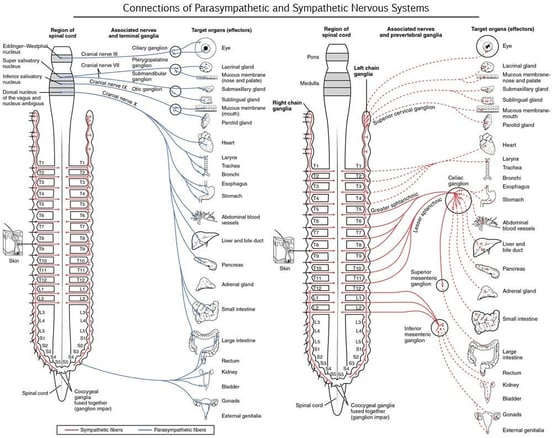
Your autonomic nervous system controls most of the automatic processes throughout your body and reaches into many of your organ systems. The parasympathetic branch of the ANS controls what you might consider “rest and digest” processes; the sympathetic branch controls the “fight or flight” processes.
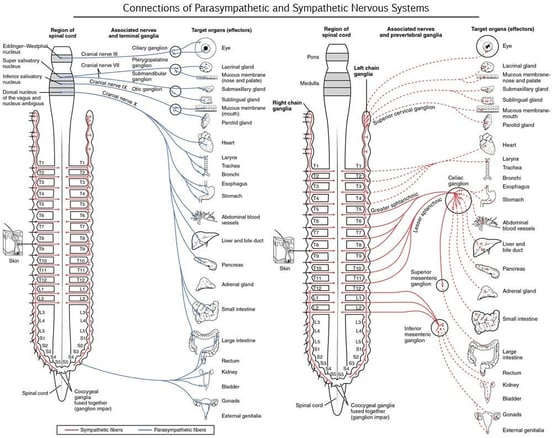
Image credit: Diffen
Dysregulation of the ANS in concussion patients often skews toward the overactivation of the sympathetic nervous system. But because the sympathetic system controls are segmented (see image above), not every patient experiences every possible symptom. Some will have eyesight issues, others will have issues with heart rate and blood pressure, and others might have digestive problems. Some will have all of the above and then some!
ANS dysregulation also occurs on a gradient: Some patients experience very mild dysregulation, and others experience extensive issues with ANS functioning.
ANS dysregulation can cause physical symptoms that feel like anxiety symptoms (such as tense muscles and heightened awareness of your surroundings), but the two are not the same. ANS dysregulation, when it affects your threat perception, typically affects the “fear” branch rather than anxiety.
ANS dysregulation and anxiety present themselves in very different ways. For example, say you’re in the kitchen and you drop a dish, causing it to shatter.
If you’re suffering from anxiety (but not dysautonomia), you might momentarily jump at the sound, but physiologically, you’ll likely feel OK in a moment. However, you might start worrying about breaking more dishes, or worrying about the cost of replacing the whole dish set, and so forth. And once the ruminative worry cycle starts, you may find it hard to stop worrying about breaking dishes.
If you’re suffering from dysautonomia (but not anxiety), you might experience a strong physiological response to dropping the dish: increased heart rate, clammy hands, and generally feeling like you’re under attack. It may take minutes or even hours for you to fully calm down. But once that reaction has passed, you probably won’t keep worrying or thinking about dropping dishes.
Both reactions are more severe than what a healthy person should experience, just in different ways.
All this isn’t to say that anxiety patients can’t have a dysregulated fear response and vice-versa; some have both. But they’re distinct symptoms caused by different problems, so the treatment approach for each is not the same.
What About Post-Concussion Panic Attacks?
It’s not uncommon for patients with anxiety to also have panic attacks; however, one is not the cause of the other. Panic attacks are a dysfunction of the fear system rather than the anxiety system. They involve a fear reaction when there’s nothing actually present to fear.
Panic attacks can happen due to a physiological reason (like dysautonomia) or a psychological reason (such as post-traumatic stress disorder). During panic attacks, many patients develop a fear of their physical sensations, which perpetuates and worsens the panic.
Even though the cause of each is not the same, having anxiety can make it easier for you to panic. Remember how the anxiety system is on a gradient? When your anxiety is already high, it’s easier to move up into the fear response and panic.
Since panic attacks can be caused by physiological or psychological factors, it’s important to have a psychologist or other health care professional sort out which one is causing your difficulties so you can receive the right kind of treatment.
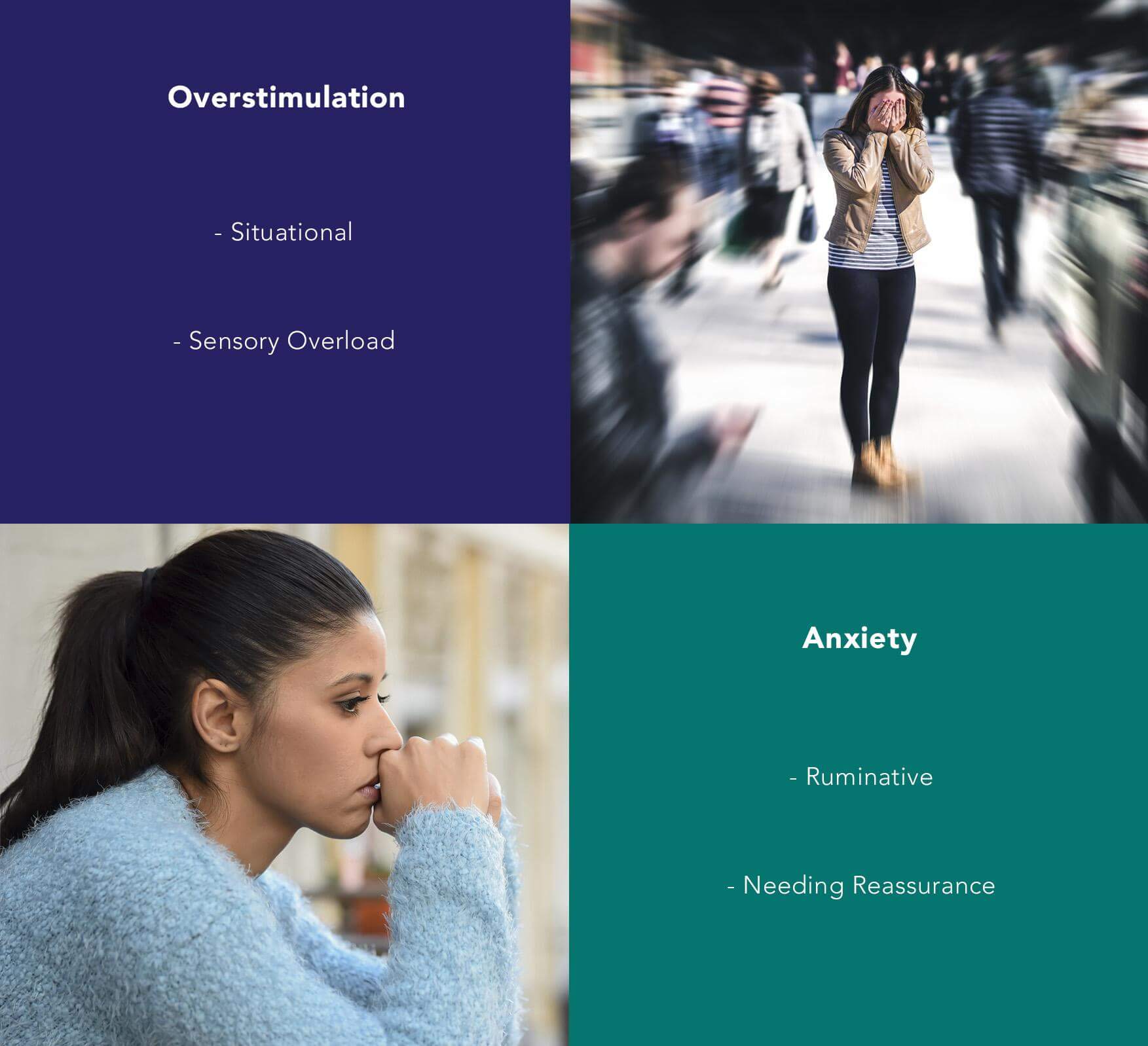
Overwhelm and Overstimulation: A Primary Concussion Symptom

Post-concussion symptoms can make certain situations unmanageable. You may find yourself feeling overwhelmed and wanting to escape from things like crowded places, bright lights, and loud noises. Or you may just hit a point in the day when you just can’t keep doing what you set out to do, and it feels impossible to try.
As a result, you might experience some dread around those times and places, be reluctant to put yourself in those situations, think through ways to escape or at least cope when you’re there, and so forth.
But the dreading and planning usually go away when a patient isn’t actively faced with a triggering situation. In between, they can relax and put aside their worries.
So, situational feelings of overwhelm or overstimulation are not the same as the ruminative anxiety we discussed earlier in the post. Anxiety extends beyond just discomfort or painful situations that trigger symptoms. Anxiety can latch onto everything from “What if I hit my head again?” and “What if the stores get completely wiped out of food and we all starve?” to “What if my child who’s playing next to me suddenly lurches forward and cracks her head open on my desk?”
To differentiate between the two, remember that overstimulation is:
- mainly limited to the situations that trigger your symptoms
- not accompanied by ruminative thinking
- not accompanied by reassurance-seeking behavior.
Why does the difference matter? Once again, anxiety and feelings of overwhelm are not caused by the same thing. Those feelings of overwhelm are caused directly by brain dysfunction following neurotrauma. The anxiety is a secondary condition that may improve somewhat from post-concussion syndrome treatment but which may not completely resolve without psychotherapy.
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion, we can help. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, sign up for a consultation.
Getting Help for Long-Term Anxiety After a Concussion
If you’re experiencing anxiety, panic attacks, or autonomic nervous system dysfunction after a head injury, you can get help. It’s important to start by treating the post-concussion symptoms themselves, then follow up with additional psychotherapy as needed.
In this section, we’ll explain how we treat post-concussion syndrome, talk about what you can further do for anxiety, and discuss when medication for anxiety makes sense.
Treating the Post-Concussion Symptoms First

During and after a concussion (or other brain injury), the immune system causes inflammation where you were injured. The affected brain regions may not get the oxygen they need during that time and may be forced to use alternate communication pathways to accomplish their tasks.
Most people heal and return to normal after about two weeks. But up to 30% of concussion patients experience lingering symptoms that stem from their brain not returning to “normal” after the immediate injury healed. Unfortunately, those persistent symptoms don’t usually go away without treatment.
Patients can experience physical symptoms (such as sleep disturbances, nausea, light sensitivity, and trouble with physical activity) and cognitive symptoms (such as difficulty concentrating, headaches, brain fog, and memory loss).
At Cognitive FX, we use functional neurocognitive imaging (fNCI) to pinpoint which brain regions are experiencing dysfunction. We can see if they are hyperactive (activating more than they should be for a given task) or hypoactive (activating less than they should be for a given task).
We use the scan results, your medical history, and a series of in-person tests to tailor your treatment program specifically to your injury and symptoms. Our patients go through intense therapy — aerobic training, neuromuscular therapy, occupational therapy, sensorimotor therapy, cognitive therapy, and more — designed to help their brains relearn efficient and healthy functioning.
At the end of treatment, we conclude with another fNCI to confirm whether the desired changes in the brain have occurred. 95% of our patients experience statistically verified restoration of brain function!
If your post-concussion anxiety is accompanied by other post-concussion symptoms, we strongly recommend you get treatment for post-concussion syndrome first. Those symptoms can play a significant role in perpetuating your anxiety; resolving them gives you the breathing room to focus on any further psychological treatment needed.
Getting Counseling
All Cognitive FX patients meet with a psychologist for an assessment and guidance on what to do after treatment. Patients receive education about what’s affecting them, what they can do on their own, and what needs to be addressed with a professional (we’re happy to give you referrals to treatment providers in your hometown).
Here are a few things anxiety patients can do to help themselves (detailed descriptions can be found in our post on anxiety during the COVID-19 pandemic):
- Limit your exposure to worry triggers (such as watching the news at night).
- Set aside 30 minutes of worry time each day. Write down your worries and then try to ignore them until worry time.
- Dedicate time to activities that help you unwind and relax each day (such as playing guitar, going for a walk outside, or reading a book).
- Practice gratitude mindfulness.
Evaluating the Need for Anxiety Medication

Most anxiety medication falls under either two categories: SSRIs (selective serotonin reuptake inhibitors) and beta-blockers. If you’re considering anxiety medication, here are a few things to think about:
The literature on SSRIs is fairly controversial.
Most SSRIs are only impactful for roughly 30% of the people who take them. Another 30% show minimal improvement while taking them, and anywhere from 30-50% show no improvement while taking them.
Anxiety medication can be a trial-and-error process. Most prescribing physicians will give you a medication to try, wait 6-8 weeks to see how it goes, adjust the dosage if needed (and wait to see if that helps), and continue with new medication until you’ve either found something that works or given up. And that’s not to mention the medications you may have to quit taking throughout the process because the side effects were too unpleasant or dangerous.
Anti-anxiety medications can have many side effects.
Speaking of side effects, anxiety meds can cause several unpleasant side effects. Many of them can overlap with common symptoms of post-concussion syndrome and may make your other symptoms worse. Even experienced medical professionals can have a difficult time knowing what’s being caused by your concussion and what’s from the medication.
Beta-blockers are only intended for short-term use.
Beta-blockers are commonly prescribed for patients to use in the moment. They’re meant to be a fallback for when you’re agitated and ruminative to the extent that you can’t sleep or do your job. They can be used in conjunction with a therapy treatment plan.
That said, they are only intended to be used in the short term. This class of medications has an overall dampening effect on your nervous system that could interfere with therapeutic efforts if taken all the time.
So what should you do?
Whether or not you take anxiety medication is a personal choice. You have to weigh how much anxiety is affecting your ability to function with the possible consequences of taking that medication.
We do recommend that our patients try not to be on anxiety medication when attending our clinic for post-concussion treatment. It may interfere with treatment effectiveness (by altering the brain’s chemistry and confusing it as to what’s “normal”). Many patients find that, with a combination of post-concussion syndrome treatment and psychotherapy, they can overcome their anxiety without medication.
Moving Forward
Understanding what causes your anxiety (or any other emotional symptoms) is worthwhile because it enables you to find the right treatment methods. Generalized anxiety, autonomic nervous system dysfunction, and overwhelm caused by post-concussion dysfunction in your brain are all approached in very different ways therapeutically.
If you’re suffering from anxiety and other symptoms after sustaining some form of head trauma (be it a concussion or something else), sign up for a consultation with our staff. We can help you understand your options and make a plan for post-concussion recovery.