Living with the mental health effects of a traumatic brain injury (TBI) can be an isolating and overwhelming journey. Not all patients realize that brain injuries can cause significant emotional changes, and those who do often don't understand why it's happening or how to fix it. Many see psychiatrists who prescribe medication that may actually make things worse (we'll explain why later in the post).
We want you to know this above all else: You're not alone in this. Your experience is legitimate, and these feelings are a real part of brain injury. Emotional symptoms are a common response when the body experiences trauma from a brain injury, especially if your physical and cognitive symptoms aren't resolving quickly.
Over 80% of the patients we see at our brain injury rehabilitation clinic in Provo, Utah, report at least one emotional symptom; anxiety and depression are the most common. In this post, we'll review:
If you’re experiencing emotional and physical symptoms that won’t resolve after a head injury, we can help. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, sign up for a consultation.
Can a Traumatic Brain Injury Cause Anxiety?
Yes, TBIs can trigger anxiety. These symptoms can develop after a mild traumatic brain injury (mild TBI) or more severe injuries (moderate TBI and severe TBI). It’s one of the most common psychological impairments, and around 20% of TBI patients experience some form of anxious feelings within the first 12 months after a head injury. This represents a 2-fold increase compared to patients without a brain injury. If left untreated, patients may continue to experience symptoms for years after the TBI.
Furthermore, a personal history of mental health issues before the neurotrauma increases the risk of developing elevated anxiety after a head injury. Patients who previously suffered from anxiety are 9 times more likely to suffer from an anxiety disorder after their TBI compared with those who never had an anxiety disorder.
How Do TBIs Cause Anxiety?
There are multiple causes for post-TBI anxiety, including:
Direct Damage to Areas of the Brain That Regulate Emotion
Damage to parts of the brain responsible for emotional and hormonal regulation can cause TBI patients to feel anxious.
These areas include the amygdala, hippocampus, and cingulate gyrus, which together make up a structure called the limbic system. Damage to the limbic system can make it harder for patients to regulate emotions, which in turn can result in feelings of anxiety.
In addition, damage to parts of the brain involved in hormonal regulation — including the pituitary gland and the hypothalamus — can affect the production and release of several hormones, such as cortisol and adrenaline, which can trigger feelings of anxiety.
Neurovascular Coupling (NVC) Disruption
Under normal conditions, nerve cells can request oxygen and nutrients from a network of blood vessels in the brain. In turn, these blood vessels deliver these resources to the right place at the right time, allowing the brain to complete that particular task. This dynamic relationship is called neurovascular coupling (NVC).
TBIs can disrupt this connection, and affected brain regions can no longer “talk” to their surrounding blood vessels and receive the resources they need. If this happens, patients may struggle to regulate their emotions or recognize various emotions in others.
Autonomic Nervous System (ANS) Dysfunction
The autonomic nervous system (ANS) controls many of the automatic processes throughout your body, including breathing, heart rate, and blood pressure. The ANS includes two subsystems, each operating on a continuum:
-
The sympathetic nervous system (SNS) activates the body to meet challenges, triggering a so-called "fight or flight" response to perceived threats.
-
The parasympathetic nervous system (PNS) directs restorative functions in the body, also known as "rest and digest" functions.
Normally, these two systems work in tandem, allowing the body to respond appropriately to varying situations. However, head injuries disrupt this equilibrium. For some TBI patients, the SNS becomes dominant and forces the body to be in a heightened state of hypervigilance, triggering anxiety symptoms such as fast heart rate, palpitations, shortness of breath, and chest pain/tightness.
Further reading: Dysautonomia after a head injury
Living with the Effects of a Brain Injury
Living with the physical and cognitive effects of a brain injury can be very difficult. TBI symptoms can impact daily activities, relationships, employment, and more. Patients can feel especially anxious about whether or not they will return to their pre-injury independent self and whether they can return to important aspects of their life, such as work and family commitments.
This uncertainty can feel overwhelming, making it even harder to focus on recovery. However, understanding the challenges you face is the first step toward finding effective ways to manage anxiety and regain a sense of control over your life.
Next, we’ll explain the symptoms of post-TBI anxiety, from emotional distress to physical sensations, and how they can affect your ability to function and heal.
Symptoms of Post-TBI Anxiety
TBI patients often describe feelings of nervousness and anxiety accompanied by ruminative or repetitive thoughts and a hypervigilant, on-guard state. Some patients also have physical signs of anxiety, including a racing heart, rapid breathing, dizziness, sweating, shaking, or the sensation of butterflies in their stomachs.
Some patients experience these symptoms constantly, often without knowing exactly why. For others, symptoms are triggered by specific situations that didn’t bother them previously.
For example, patients may feel anxious if they need to go to the grocery store because they get overstimulated in a crowded place or struggle when cognitive or physical symptoms flare. They may also feel overwhelmed and worry in situations that require attention, fast thinking, or processing a lot of information simultaneously.
There are cognitive, emotional, and physical symptoms of anxiety, including:
- Excessive worry and rumination
- Difficulty thinking, concentrating, and problem-solving
- A sense of doom
- Increased heart rate
- Trembling
- Breathing rapidly or shortness of breath
- Feeling tired or weak, with difficulty sleeping
- Feeling dizzy
- Muscle tension and headaches
- Hot and cold flushes
- Nausea
Types of Anxiety Disorders After a TBI
Anxiety symptoms are common after a TBI, but patients may develop different anxiety disorders, including:
-
Generalized anxiety disorder (GAD): Patients with GAD experience elevated hypervigilance, constant rumination, and worry. This is one of the most common forms of anxiety in TBI patients, and up to ⅓ of patients with anxiety develop this condition. Many of these patients also develop depressive symptoms.
-
Panic disorder: Patients with panic disorder experience recurrent and unexpected panic attacks with accompanying fear. Symptoms include shaking, dizziness, chest pain, and fear of dying. About 14% of TBI patients develop this condition.
-
Specific phobias: Phobias involve an intense fear of certain situations, including heights, darkness, or flying, for example. It’s not uncommon for TBI patients to develop a fear regarding the situation involving their incident. For example, a study found that 7% of TBI patients involved in a motor vehicle accident developed phobias related to traveling in a car.
-
Social anxiety: This type of anxiety disorder is experienced when anticipating or participating in social situations where individuals fear being judged or perceived negatively by others and have concerns that they’ll be unable to perform adequately in social situations. For TBI patients, cognitive (especially verbal processing) and physical impairments can heighten these concerns, leading to increased anxiety and self-consciousness in social interactions. Despite its prevalence among those with TBIs, social anxiety remains an under-researched aspect of post-TBI anxiety.
Other psychological disorders are not specifically classified as anxiety disorders but are also common in TBI patients and can be a source of anxiety. These include:
-
Post-traumatic stress disorder (PTSD): PTSD is characterized by re-experiencing an extremely traumatic event; for TBI patients, it tends to be the incident that led to their injury. TBI patients often experience dreams and nightmares about that event, even if they only have spotty memories. This can be a great source of anxiety. Studies show that about 13% of TBI patients develop PTSD within 3 months after the injury.
-
Obsessive-compulsive disorder (OCD): OCD is characterized by recurrent obsessions and compulsions that cause anxiety. This may include intrusive thoughts, the need to perform repetitive behaviors, or aggressive impulses. Studies show that about 14% of TBI patients meet the criteria for an OCD diagnosis. There’s some evidence to suggest that the development of OCD after a TBI starts as a way for patients to cope with their injuries. For example, repetitive behavior may help patients regain the feeling of control over their lives, or repetitive checking may allow them to compensate for memory deficits, but these eventually become a source of stress and anxiety.
Treatment Options for Anxiety After a TBI
The most common and effective treatment for TBI-related anxiety is cognitive behavioral therapy (CBT). Some patients may also benefit from medication for specific symptoms, but this is often not enough to treat anxiety in TBI patients.
It’s crucial that TBI patients experiencing anxiety symptoms seek treatment, as anxiety disorders can significantly lower quality of life and delay recovery from the TBI. TBI patients with anxiety often experience TBI symptoms more intensely and perceive their level of cognitive impairment to be more severe compared to TBI patients without anxiety.
Finding the right treatment not only helps patients deal with anxiety symptoms but also helps them cope with other TBI-related physical and cognitive symptoms, resulting in a significant improvement in their quality of life.
1. Cognitive Behavioral Therapy (CBT)
The evidence supporting the use of psychotherapy to address anxiety after a TBI has been steadily expanding over the last 20 years. To date, the most common and effective form of psychotherapy for anxiety disorders is cognitive behavioral therapy (CBT).
CBT is based on the premise that cognition or thinking patterns trigger anxiety and that changing thought and behavioral patterns will result in reduced anxiety. The aim is to help patients develop strategies to change anxiety-provoking thought and belief patterns, to address avoidant behaviors, and to develop more adaptive reactions to anxiety itself.
Multiple studies support the use of CBT to treat anxiety, which often produces results superior to medication. After a TBI, CBT can help patients reduce their anxiety symptoms and stay symptom-free, especially if they attend regular booster sessions. What’s more, CBT doesn’t just help with anxiety symptoms — it can also help TBI patients experience fewer post-TBI symptoms in general.
2. Medication for Anxiety
Although TBI patients are commonly prescribed medication for anxiety, there is some evidence that these interventions have limited efficacy. In addition, these patients are more susceptible to side effects and often experience worse cognitive difficulties.
Most anxiety medications fall under one of two categories: SSRIs (selective serotonin reuptake inhibitors) and beta-blockers.
-
SSRIs: Multiple studies show that TBI patients with neurological symptoms can be treated with SSRIs (a common type of antidepressant medication), of which sertraline is one of the most common drugs used. Despite this, it’s difficult to assess how effective these treatments are in addressing anxiety symptoms specifically, as most patients also experience depression and other mood disorders. In addition, finding the right medication can be challenging. Patients need to try a medication for 6-8 weeks to see if it works and then start again with a new one if it’s not effective.
-
Beta-blockers: Beta-blockers are typically prescribed for patients to use over a short period. They’re meant to be a fallback for when patients are agitated and anxious to the extent that they can’t sleep or do their job. This class of medications has an overall dampening effect on the SNS.
Whether or not you take anxiety medication is a personal choice. Patients need to consider how much anxiety is affecting their ability to function while considering the possible consequences and side effects associated with taking medication.
We do recommend that our patients try not to be on anxiety medication when attending our clinic for post-concussion treatment. It may interfere with treatment effectiveness by altering the brain’s chemistry and confusing it as to what’s “normal”. With a combination of post-concussion syndrome treatment and psychotherapy, many patients with head trauma find they can overcome their anxiety without medication.
Why Effective Treatment Requires Addressing Both Brain Dysfunction and Anxiety Disorders
Effectively treating anxiety after a traumatic brain injury (TBI) means addressing both the neurological dysfunction caused by the injury and any underlying or co-occurring anxiety disorder — whether or not that anxiety stems directly from the injury itself.
As discussed earlier, anxiety can arise from a range of sources. Some symptoms are the result of physical changes in the brain, such as neurovascular coupling disruption or autonomic nervous system dysfunction. Others stem from the emotional and psychological impact of living with post-TBI symptoms, including uncertainty about recovery, loss of independence, or disruption to work and social life.
In many cases, it’s difficult to pinpoint exactly which mechanism is causing a patient’s anxiety. More often, it’s a complex mix of neurological and psychological factors. That’s why patients benefit most from a dual-pathway approach: one that targets the brain dysfunction through rehabilitative treatment and another that addresses the anxiety disorder itself through evidence-based therapy such as cognitive behavioral therapy (CBT).
At Cognitive FX, we focus on treating the brain dysfunction caused by injury (more on this below), but we also encourage patients to pursue cognitive behavioral therapy to address anxiety symptoms that may be rooted in emotional, behavioral, or psychological factors. Treating both aspects is key to a full and lasting recovery.
Receiving TBI Treatment at Cognitive FX
At Cognitive FX, we specialize in treating brain injury. We begin with a comprehensive evaluation to understand how your TBI has affected your brain and body. A member of our team will review your medical history and symptoms, including anxiety and other emotional and psychological symptoms.
To understand your injury, we conduct a series of specialized tests, including:
-
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
-
A neurocognitive test to assess memory, concentration, reasoning, and other cognitive functions.
-
A psychological evaluation to assess symptoms of anxiety, depression, and other mental health problems.
-
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
-
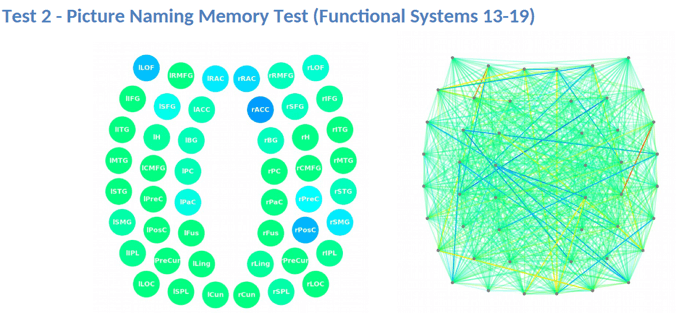
A brain imaging scan called functional Neurocognitive Imaging (fNCI) to determine where and how your brain was affected by the injury.
The fNCI scan measures blood flow in 100 brain regions while patients perform standardized cognitive tasks. These real-time images are then compared to scans from healthy individuals to identify areas with neurovascular coupling (NVC) dysfunction.
Brain regions are grouped by function and scored:
- Green indicates normal function.
- Yellow and red highlight areas with NVC dysfunction, signaling impaired brain activity.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
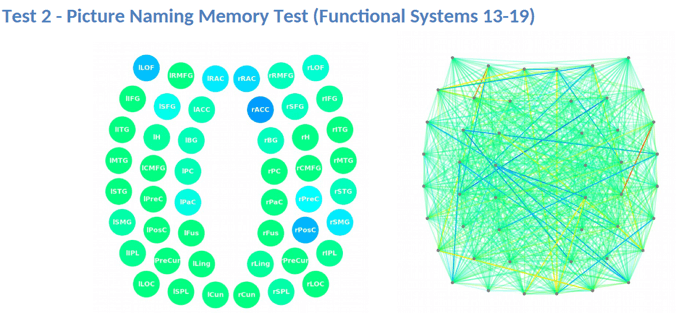
After the evaluation, our team analyzes the results and creates a customized treatment plan tailored to each patient’s specific areas of dysfunction. The goal is to restore normal neurovascular coupling and improve overall brain function.
What EPIC Treatment Is Like
During treatment week, patients follow a structured program combining aerobic exercise and targeted therapies to enhance brain function. Each session begins with aerobic exercise to boost blood flow, followed by a personalized mix of therapies designed to support brain healing. The specific treatments vary based on each patient’s scan results, ensuring a tailored approach to recovery.
Therapy typically consists of a mix of the following:
-
Cognitive therapy: Cognitive therapy aims to rehabilitate cognitive skills, such as memory, attention, decision-making, and reasoning. Sessions include cognitive activities, such as solving logic puzzles and identifying word patterns.
-
Occupational therapy: Patients engage in exercises that help the brain, body, and eyes coordinate with each other. The aim is to help patients readjust to their daily activities by focusing on difficulties identified on their fNCI scan, including compensatory strategies for work and school as they recover.
-
Neuromuscular therapy: The aim is to relieve headaches and neck pain, rehabilitate balance, improve body-brain coordination, and promote physical activity. Patients receive massages, stretches, and soft tissue manipulation to increase blood flow.
-
Sensorimotor therapy: Patients follow exercises to improve cognitive and physical skills. For example, this may involve performing simple movement patterns in time with a metronome to address cognitive, visual, and vestibular symptoms.
-
Vision therapy: The aim is to address vision problems, such as blurred vision, difficulty focusing, and light sensitivity. Our therapists use different exercises, such as Dynavision, visual tracking exercises, the Brock String, and other computerized technologies.
-
Neurointegration therapy: The aim is to assess the visual, vestibular, and proprioceptive systems and integrate them to improve patients’ ability to function in the world. Patients receive help with a variety of vestibular issues, including poor posture, dizziness, and vertigo. Vision exercises are often incorporated as well, such as saccades, near/far focusing, convergence/divergence, peripheral awareness, and hand/foot/eye coordination.
-
Psychotherapy: Patients meet with a clinical psychologist to evaluate their mental health status and learn cognitive, behavioral, and emotional regulation strategies to reduce problematic thought, behavioral, and emotional patterns that often accompany TBI. For those suffering from depression and anxiety disorders, our therapists recommend cognitive behavioral therapy (CBT).
At the end of treatment, patients undergo a follow-up scan to see how the brain is responding to therapy. While some experience immediate, significant improvements, others may need more time for changes to take effect. 90% of our patients report symptom improvements during treatment, with continued progress at home.
Following treatment, our team reviews your scan results and provides a personalized recovery plan, including aerobic exercise, cognitive games, and cognitive rest to support long-term healing.
You may find it helpful to read the recovery stories some of our other patients have shared. Here are a few links to get you started:
-
Myrthe van Boon is a mother of two who struggled with debilitating post-concussion symptoms for years before finding Cognitive FX.
-
Olivia Seitz is a former figure skater who found symptom relief after more than a decade of chronic illness.
-
Sam Pembleton was an adolescent hit by a soccer ball in the head; she tried treatment methods for five years before finding Cognitive FX.
-
These patients all completed video testimonials about their initial injury and their experience at Cognitive FX.
On average, our patients’ symptoms improve by 60% after just one week of treatment. To see if you are eligible for treatment, sign up for a consultation.
Self-Care Strategies for Managing Post-TBI Anxiety
Here are a few tips to help you cope with anxiety symptoms while you recover:
-
Talk to someone: Simply talking to someone about the things that make you anxious or worried may help reduce your anxiety. Share your feelings with someone you trust, such as a close friend, caregiver, or therapist.
-
Follow a healthy lifestyle: Our mood is affected by our physical health. Our advice is to follow a healthy lifestyle, including regular exercise, a balanced diet, and limited alcohol consumption after brain injury.
-
Identify your triggers: Identifying what makes you anxious (and when) can provide some insight into why you feel this way. Most patients find that certain situations or certain times of the day are more likely to make them anxious. The best way is to keep a diary to record when you feel worried and what you’re doing. This can be something just for you or something you may wish to share with friends, family, or a professional.
-
Practice breathing exercises: A common symptom of anxiety is feeling breathless. Several breathing exercises may help alleviate rapid breathing and lower your anxiety levels. For example, even just taking a few deep breaths when you feel anxious can help you calm down. Taking a deep breath and slowly exhaling activates the parasympathetic nervous system, which helps your body relax and calm down.
-
Use visualization techniques: Visualization techniques aim to reduce anxious thoughts by allowing the mind to focus on something more positive; you may wish to combine this with breathing exercises. If you’re anxious about a particular task, try to focus your mind on a relaxing scene or a happy memory.
-
Practice mindfulness: This is a technique that keeps you focused on the present moment rather than worrying unnecessarily about the future. Mindfulness meditation involves sitting quietly and simply observing rather than engaging in your thoughts, bringing your attention back whenever you start to feel anxious.
-
Find a distraction: When you’re anxious, you’re more likely to mull over your thoughts and worry, which can worsen anxious symptoms even further. One way to stop this is to find something as a distraction. This could include doing a puzzle, listening to music, or speaking to friends.
-
Avoid caffeinated drinks: Some people find that caffeinated drinks can make their symptoms of anxiety worse. Try finding a balance with how much caffeine you consume, or try decaffeinated drinks where possible. Remember that caffeine can also be found in chocolate, energy drinks, and some health supplements.
-
Set realistic expectations for your recovery: Remember that some symptoms of brain injury can take weeks, months, or years to improve, while others may recover faster. Be kind to yourself, and celebrate achievements where possible.
Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, sign up for a consultation.