Emotions are expressed in many ways—through gestures, facial expressions, and the tone of our voice. When you're happy or upset, others typically recognize those emotions by looking at you and hearing them in your speech. But after a traumatic brain injury (TBI), you may suddenly find that, despite feeling joy, sadness, or frustration, your face and voice don’t reflect what you’re experiencing inside. Instead, you may appear emotionless, indifferent, or disconnected, even when you desperately want to express how you feel.
Known as flat affect, this condition can confuse patients and their loved ones, making daily life frustrating and isolating. But it's not a sign that your personality has changed—it’s often a result of disrupted brain function from your head injury.
Treatment for flat affect in TBI patients is complex, as it often requires more than just practicing facial expressions or adjusting medication. In this article, we provide a detailed overview of what it’s like to live with flat affect after TBI, how brain injuries can cause flat affect, and what to know about your treatment options.
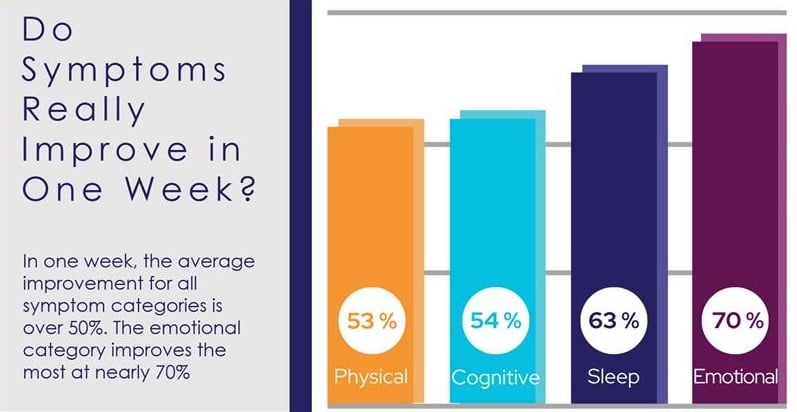
If you’re experiencing emotional and physical symptoms that won’t resolve after a head injury, we can help. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their brain injury symptoms. Cognitive FX is the only TBI treatment clinic with third-party validated outcomes. To see if you are eligible for treatment, sign up for a consultation.
What Is Flat Affect, and Can It Happen After Brain Injury?
“Affect” refers to the nonverbal ways we express emotions, including facial expressions, tone of voice, gestures, and body language. Under normal circumstances, people display a full range of emotions, from joy to sadness, in ways that align with their experiences. This is known as having a full or broad affect.
After a traumatic brain injury (TBI), some individuals lose the ability to express their emotions outwardly, even though they may still experience them internally. This condition is called flat affect. Rather than showing natural emotional highs and lows, a person with flat affect appears emotionally neutral, as if their emotions have been "flattened."
Crucially, flat affect does not mean a person lacks emotions—rather, their ability to express those emotions is impaired. This creates a mismatch between what they feel internally and how others perceive them.
Common Symptoms of Flat Affect
Indicators of flat affect include a lack of:
- Vocal variation (monotone voice)
- Body language (limited eye contact, facial expressions, and hand gestures)
- Laughter or crying
- Interest in social interactions
- Verbal and nonverbal responses
- Empathy or emotional reciprocity
What’s It Like to Live With Flat Affect?
Because individuals with flat affect do not outwardly display emotions, they may appear uninterested or detached, even in significant moments. For example:
-
If a friend shares exciting news, such as winning the lottery, a person with flat affect might respond with a neutral, “That’s nice.”
-
If told about the death of a loved one, they may simply say, “That’s sad,” with little visible emotion.
This emotional disconnect can be misinterpreted as indifference, making social interactions challenging. Loved ones may feel unappreciated when their smiles, jokes, or expressions of concern aren’t reciprocated. Over time, this deficit can lead to misunderstandings, strained relationships, and social withdrawal, increasing feelings of isolation and lowering the quality of life.
Flat Affect vs. Blunted Affect vs. Restricted Affect
Flat affect is not the only condition that affects emotional expression after a TBI. Some individuals experience less severe versions, including blunted affect and restricted affect.
Flat Affect vs. Blunted Affect
Blunted affect is often considered a less extreme form of flat affect. Individuals with blunted affect may show limited facial expressions and struggle to convey emotions, but they are not entirely devoid of outward emotion.
-
Flat affect: No visible emotional response, even in significant situations.
-
Blunted affect: Some emotional expression, but it is noticeably diminished or muted.
Restricted Affect
Restricted affect differs from flat and blunted affect in that it primarily affects the range of emotional reactions displayed rather than the intensity.
Individuals with restricted affect may express some emotions but tend to stay within a narrow emotional range, avoiding extreme highs or lows. For example, they might react to exciting or upsetting news in a similar, subdued manner, showing only minimal emotional expression.
Is Flat Affect the Same as Depression?
Flat affect is often mistaken for depression, but they are distinct conditions.
-
Flat affect occurs when the expression of emotions is impaired—but the person may still experience emotions internally.
-
Depression, on the other hand, often involves a reduced ability to feel a range of emotions and predominantly feeling down, sad, or apathetic.
-
Depression may also include anhedonia, or the loss of ability to experience pleasure and interest, which is distinct from emotional blunting, a broader reduction in the ability to feel most or all emotions.
Flat affect can result from brain injuries or neurological disorders, as well as mental health conditions like depression. However, individuals with depression may also exhibit flat or blunted affect, which is why the two conditions are sometimes confused.
Further reading: Depression after TBI
How Can a Brain Injury Cause Flat Affect?
There are multiple ways brain injuries can cause flat or blunted affect. In most patients, it’s difficult to determine the exact cause, and it’s often a combination of factors.
The most common causes include:
- Damage to the brain regions responsible for controlling emotions
- Neurovascular coupling disruption
- Autonomic nervous system dysfunction
- Facial paralysis
- Antidepressant medication
- Mood disorders
Direct Damage to Brain Regions Controlling Emotions
Flat affect can be the consequence of direct damage to the areas of the brain involved in regulating emotions, including the amygdala, brainstem, prefrontal cortex, and anterior cingulate cortex.
There are no studies directly with TBI patients, but patients with schizophrenia diagnosed with flat affect show marked differences in these areas in fMRI scans when presented with emotional stimuli compared to individuals with normal affect.
Neurovascular Coupling Disruption
Under normal conditions, nerve cells can request oxygen and nutrients from a network of blood vessels in the brain. In turn, these blood vessels deliver these resources to the right place at the right time, allowing the brain to complete that particular task. This dynamic relationship is called neurovascular coupling (NVC).
Brain injuries often disrupt NVC, leading to inadequate or mistimed delivery of essential resources to specific brain regions. If areas like the amygdala or prefrontal cortex are affected, patients may develop flat affect, struggling to express emotions despite still feeling them. Additionally, NVC disruption can cause headaches, fatigue, poor sleep, irritability, and sensory sensitivity, which may further hinder emotional expression.
Autonomic Nervous System Dysfunction
The autonomic nervous system (ANS) controls many of the automatic processes throughout your body, including breathing, heart rate, and blood pressure. The ANS includes two subsystems, which each operate on a continuum:
-
The sympathetic nervous system (SNS) activates the body to meet challenges and may trigger so-called "fight or flight" in response to perceived threats.
-
The parasympathetic nervous system (PNS) directs restorative functions in the body, or so-called "rest and digest" functions.
The SNS and PNS interact dynamically in response to emotional stimuli. The SNS is associated with arousal states—both positive (excitement and joy) and negative (fear and anger). The PNS facilitates relaxation and recovery, contributing to emotions like contentment and social bonding. However, both systems can be active in different emotional contexts depending on intensity and situation.
Brain injuries can disrupt the autonomic nervous system, leading to dysfunction in both the sympathetic and parasympathetic nervous systems. SNS dysfunction may impair arousal and emotional responsiveness, reducing facial expressions and vocal tone, while PNS dysfunction can limit emotional regulation and social engagement. This imbalance can contribute to experiencing flat affect.
Further reading: Dysautonomia after a head injury
Facial Paralysis
The inability to show facial expressions—an important part of how we show emotions—can also be triggered if the brain injury damages the facial nerve (also called the seventh cranial nerve), causing facial paralysis. Patients may also experience flat affect due to facial paralysis if the part of the brain that processes input from the facial nerve is affected.
Antidepressant Medication
Flat or blunted affect can occur as a side effect of taking antidepressant medication in some patients. The risk increases significantly in patients who are prescribed multiple antidepressant medications or taking both antidepressants and antipsychotics. Examples include Lexapro (escitalopram), Paxil (paroxetine), Prozac (fluoxetine), and Zoloft (sertraline). Interestingly, a study found that SSRIs are more likely to cause flat affect than SNRIs.
TBI-Related Mood Disorders
Finally, TBI patients may experience flat affect not directly caused by the brain injury, but as a consequence of developing mental health conditions, such as depression or post-traumatic stress disorder (PTSD), after their head injury. Flat affect is often a symptom of these conditions.
The good news is that, as depression and PTSD are treated with therapy and/or medication, patients can regain their emotional responsiveness.
Further reading: Concussions can cause PTSD
How Is Flat Affect Treated?
The treatment for flat affect depends on its underlying cause. While therapy and medication are common interventions, they may not be enough on their own. Since flat affect often stems from disrupted brain function, addressing the brain damage itself—rather than treating flat affect as an isolated symptom—is often essential for lasting improvement.
Common Treatments For Flat Affect
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) helps patients identify and understand the connection between their thoughts, emotions, and behaviors. For individuals with flat affect, CBT can also focus on improving emotional awareness and social skills by teaching them to recognize emotional cues in themselves and others.
Therapists may guide patients through structured exercises to practice facial expressions, interpret body language, and engage in appropriate social interactions. This might include learning when to smile, make eye contact, or greet a friend, even if the emotional response does not feel instinctive. These behaviors can become more automatic through repetition and reinforcement, helping patients improve their emotional expression and social connections over time.
Speech Therapy
Speech therapy can be beneficial for individuals with flat affect, particularly in addressing a monotone or robotic voice. Speech therapists help patients regain control over vocal pitch, tone, and inflection, making their speech sound more expressive.
Additionally, therapy can improve a patient’s ability to recognize emotional cues in others’ speech, enhancing social interactions. One common approach is melodic intonation therapy (MIT), which uses musical patterns to help patients develop more natural vocal modulation.
Marriage and Family Therapy
Flat affect can strain relationships, as family members, friends, and caregivers may struggle to understand how the affected person is feeling. This lack of emotion can lead to miscommunication and frustration on both sides. Marriage and family therapy with a trained therapist provides a neutral space to discuss these emotional problems, help bridge communication gaps, improve emotional understanding, and develop coping strategies to strengthen relationships.
Medication
Currently, no medications are specifically approved to treat flat affect. However, antipsychotic and antidepressant medications may help improve motivation and emotional responsiveness, particularly for patients whose flat affect is linked to conditions like depression or PTSD.
While research on medication for flat affect in traumatic brain injury (TBI) patients is limited, studies on schizophrenia patients with flat affect suggest that atypical antipsychotics, such as Clozaril (clozapine), may help alleviate some symptoms. However, the effectiveness of these treatments can vary, and further research is needed to determine their role in managing flat affect in different conditions.
Treating Underlying Brain Dysfunction That Causes Flat Affect In TBI Patients
The individual therapies described above may help you if you’re experiencing flat affect. However, the reality is that for most TBI patients, flat affect is not the only challenge. It occurs alongside fatigue, headaches, sensory sensitivity, cognitive impairments, and other physical, emotional, and psychological symptoms.
Unfortunately, most healthcare providers are not set up to treat brain injuries in a holistic, coordinated way that addresses patients’ underlying brain dysfunction. Patients are forced to seek care from many different doctors for individual symptoms, a process that can drag on for years without producing significant improvements in overall health and brain function.
This is the gap in our healthcare system that we’ve designed our clinic to fill. At Cognitive FX, we treat different types of brain injuries, including post-concussion syndrome, transient ischemic attacks (TIAs), carbon monoxide poisoning, and more.
Our treatment program, called Enhanced Performance In Cognition (EPIC), uses state-of-the-art imaging technology to pinpoint the exact areas of the brain that have been affected by your injury, and our multidisciplinary team provides customized therapies to address each patient's specific symptoms.
TBI Treatment at Cognitive FX
TBI treatment starts with an in-depth patient assessment. Patients undergo a variety of exams, including:
-
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
-
A neurocognitive test to assess memory, concentration, reasoning, and other cognitive functions.
-
A psychological evaluation to assess symptoms of anxiety, depression, and other mental health problems.
-
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
-
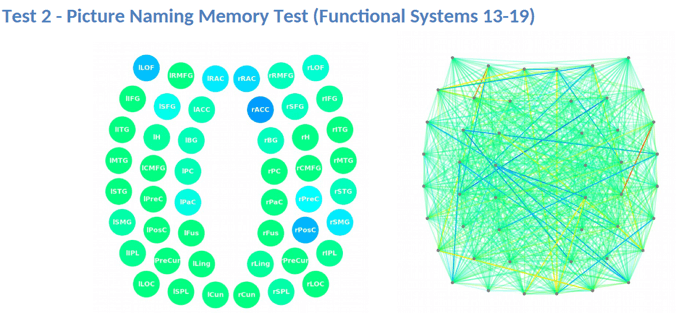
A brain imaging scan called functional Neurocognitive Imaging (fNCI) to determine where and how your brain was affected by the injury.
The fNCI scan measures blood flow in 100 brain regions while patients perform standardized cognitive tasks. These real-time images are then compared to scans from healthy individuals to identify areas with neurovascular coupling (NVC) dysfunction.
Brain regions are grouped by function and scored:
-
Green indicates normal function.
-
Yellow and red highlight areas with NVC dysfunction, signaling impaired brain activity.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
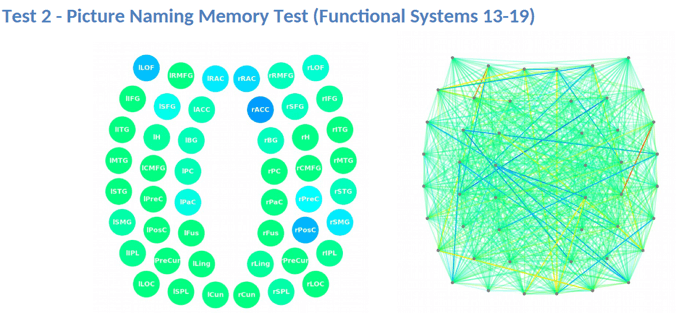
After the evaluation, our team analyzes the results and creates a customized treatment plan tailored to each patient’s specific areas of dysfunction. The goal is to restore normal neurovascular coupling and improve overall brain function.
Therapy typically consists of a mix of the following:
-
Cognitive therapy: Cognitive therapy aims to rehabilitate cognitive skills, such as memory, attention, decision-making, and reasoning. Sessions include cognitive activities, such as solving logic puzzles and identifying word patterns
-
Occupational therapy: Patients engage in exercises that help the brain, body, and eyes coordinate with each other. The aim is to help patients readjust to their daily activities by focusing on difficulties identified on their fNCI scan, including compensatory strategies for work and school as they recover.
-
Neuromuscular therapy: The aim is to relieve headaches and neck pain, rehabilitate balance, improve body-brain coordination, and promote physical activity. Patients receive massages, stretches, and soft tissue manipulation to increase blood flow.
-
Sensorimotor therapy: Patients follow exercises to improve cognitive and physical skills. This includes, for example, simple movement patterns in time with a metronome to address cognitive, visual, and vestibular symptoms
-
Vision therapy: The aim is to address vision problems, such as blurred vision, difficulty focusing, and light sensitivity. Our therapists use different exercises, including Dynavision, visual tracking exercises, the Brock String, and some other computerized technologies.
-
Neurointegration therapy: The aim is to assess the visual, vestibular, and proprioceptive systems and integrate them to improve patients’ ability to function in the world. Patients receive help with a variety of vestibular issues, including poor posture, dizziness, and vertigo. Vision exercises are often incorporated as well, such as saccades, near/far focusing, convergence/divergence, peripheral awareness, and hand/foot/eye coordination.
-
Psychotherapy: Patients meet with a clinical psychologist to evaluate their mental health status and learn cognitive, behavioral, and emotional regulation strategies to reduce problematic thought, behavioral, and emotional patterns that often accompany TBI. For those suffering from depression and anxiety disorders, our therapists recommend cognitive behavioral therapy (CBT).
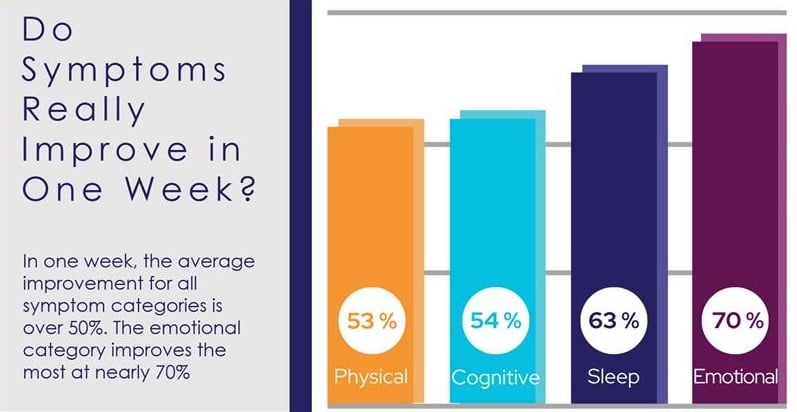
Patients undergo a follow-up scan at the end of treatment to see how the brain is responding to therapy. While some experience immediate, significant improvements, others may need more time for changes to take effect. 90% of our patients report symptom improvements during treatment, with continued progress at home.
Following treatment, our team reviews your scan results and provides a personalized recovery plan, including aerobic exercise, cognitive games, and cognitive rest to support long-term healing.
You may find it helpful to read the recovery stories some of our other patients have shared. Here are a few links to get you started:
-
Myrthe van Boon is a mother of two who struggled with debilitating post-concussion symptoms for years before finding Cognitive FX.
-
Olivia Seitz is a former figure skater who found symptom relief after more than a decade of chronic illness.
-
Sam Pembleton was an adolescent hit by a soccer ball in the head; she tried treatment methods for five years before finding Cognitive FX.
-
These patients all completed video testimonials about their initial injury and their experience at Cognitive FX.
On average, our patients’ symptoms improve by 60% after just one week of treatment. To see if you are eligible for treatment, sign up for a consultation.