Traumatic brain injuries (TBIs) can change how a person experiences and expresses their sexuality. For some, the effects are subtle. For others, head injuries can cause dramatic changes to their sex life—from reduced sex drive and erectile dysfunction to heightened or inappropriate sexual behaviors.
These changes often ripple into relationships, leading to anxiety, frustration, and emotional distance. Without intervention, they can strain partnerships and even lead to breakups.
Despite how common these issues are, talking about sexual health after a TBI can feel embarrassing. Many patients avoid discussing it with their doctors, even though sexuality is an important part of life—and like other health concerns, sexual problems can often be treated.
In this article, we’ll explore how TBIs can affect sexual function, the possible causes, and what treatment options are available. While Cognitive FX does not treat sexual dysfunction directly, our approach to brain injury treatment focuses on healing the brain as a whole, which can improve related symptoms.
Below, we cover:
How TBIs Can Affect Sexual Function
About 60% of patients experience some form of sexual dysfunction after a TBI. Alarmingly, around 20% still struggle to resume sexual activity a year after their injury.
Researchers believe these numbers may be underestimated because cultural and personal barriers make people less likely to self-report sexual difficulties.
Common symptoms of sexual dysfunction after a TBI include:
- Deficits in sex drive and desire
- Decreased frequency of sexual activity
- Erectile dysfunction or impotence
- Vaginal dryness and discomfort
- Difficulty reaching orgasm/ejaculation
- Decreased sexual satisfaction
- Sensory changes affecting arousal
- Loss of emotional connection
- Heightened sexual drive or inappropriate comments
- Difficulty controlling sexual behavior
- Menstrual cycle irregularities
- Trouble connecting with a sexual partner
Causes of Sexual Dysfunction After TBI
Sexual changes after an acquired brain injury can stem from a combination of neurological, hormonal, emotional, and physical factors.
Potential causes include:
1. Direct Damage to Brain Regions Involved in Sexual Function
Several parts of the brain regulate sexual activity and emotional connection. Damage to these regions can alter desire, arousal, and behavior:
-
Frontal lobes — Injury here can lead to inappropriate sexual behaviors, difficulty initiating sexual activity, or reduced ability to feel pleasure.
-
Temporal lobes — Damage can heighten sexual interest and make it harder to interpret social cues, such as mistaking friendliness for flirtation.
-
Parietal lobes — Some patients develop unusually heightened sexual arousal that may feel overwhelming rather than pleasurable.
-
Amygdala — Impairment can blunt the intensity of orgasm and reduce overall sexual sensations.
2. Neurovascular Coupling (NVC) Disruption
Healthy brain function relies on neurovascular coupling (NVC)—the process where nerve cells request oxygen and nutrients from nearby blood vessels, which then deliver these resources at the right time and place.
After a TBI, this system often breaks down. Regions involved in sexual desire, arousal, or emotional connection may not receive adequate support, contributing to dysfunction.
NVC disruption can also cause headaches, fatigue, sleep problems, and other symptoms that indirectly worsen sexual issues.
3. Autonomic Nervous System (ANS) Dysfunction
The autonomic nervous system regulates unconscious bodily functions, including blood pressure, heart rate, and sexual response.
Normally, the parasympathetic nervous system (PNS) promotes arousal—such as increasing blood flow during erections—while the sympathetic nervous system (SNS) activates during orgasm.
TBIs can disrupt this balance, causing the SNS to remain overactive when it shouldn’t. This can lead to:
- Difficulty achieving or maintaining arousal
- Erectile dysfunction
- Changes in libido (either reduced or heightened)
- Trouble reaching orgasm
For more, see our guide to post-concussion autonomic dysfunction.
4. Hormonal Imbalances
TBIs can affect the hypothalamus and pituitary gland, disrupting hormone production. Imbalances in estrogen, testosterone, progesterone, and thyroid hormones can affect sexual desire and function:
- Low estrogen may cause decreased libido, vaginal dryness, and pain during sex.
- Low testosterone can contribute to erectile dysfunction.
Hormonal issues can also trigger fatigue, mood swings, muscle weakness, sleep disturbances, and hair loss, all of which can indirectly impact sexual health.
5. Emotional and Psychological Symptoms
Depression, anxiety, and low self-esteem are common after TBIs—and they can dramatically affect intimacy.
- Anxiety may cause excessive worry about sexual performance.
- Low self-confidence or feelings of unattractiveness may reduce desire.
- Depression often leads to decreased libido and difficulties with arousal or orgasm.
These challenges can create a feedback loop: emotional distress worsens sexual dysfunction, and sexual dysfunction worsens emotional distress.
6. Other TBI Symptoms and Medications
Physical and cognitive symptoms after a TBI can also interfere with sexual activity. For example:
- Fatigue reduces stamina.
- Dizziness or balance issues can make sexual activity uncomfortable.
- Pain or headaches may lower interest in intimacy.
Additionally, many medications prescribed for TBI-related issues—such as antidepressants, antipsychotics, anti-seizure medications, muscle relaxants, and painkillers—can lead to side effects such as decreased libido, difficulty with arousal, and delayed orgasm.
Treatment Options for Sexual Dysfunction After a TBI
Effective treatment depends on identifying the root cause, which may be physical, emotional, or both.
Seek Support From a Healthcare Professional
Start by speaking openly with a doctor or other healthcare provider. It can feel uncomfortable, but sexuality is part of overall health, and professionals can help. You can also contact local brain injury associations for resources and referrals.
Get a Comprehensive Medical Exam
This may include:
- Blood work and hormone testing
- A urine screen
- A gynecological exam for women
- A urological exam for men
Checking hormone levels is especially important, as imbalances are treatable.
Explore Therapy Options
-
Psychotherapy can help address anxiety, depression, and self-esteem issues impacting sexual function.
-
Couples therapy may improve communication and intimacy.
-
Sex therapy, ideally with a provider experienced in TBIs, can address both physical and psychological challenges in sexual relationships.
Consider Lifestyle Changes
A healthy diet, regular exercise, stress management, and better sleep hygiene can improve both overall well-being and sexual health.
Discuss Medication Options
Medications like sildenafil (Viagra) may help men with erectile dysfunction. Interestingly, some evidence suggests Viagra could improve brain blood flow, potentially benefiting other TBI symptoms. Always consult your doctor before starting medication.
Our Unique Approach to TBI Treatment at Cognitive FX
While we do not directly treat sexual dysfunction, our work focuses on healing the root causes of TBI-related symptoms through our Enhanced Performance in Cognition (EPIC) program.
Most patients who experience sexual dysfunction after a TBI also face other issues — such as headaches, dizziness, brain fog, and depression. Our approach addresses the underlying brain dysfunction, which can improve multiple symptoms at once.
What Sets Cognitive FX Apart From Other Clinics
We specialize in treating patients with lingering symptoms from mild traumatic brain injury, including post-concussion syndrome (PCS), transient ischemic attack (TIA), carbon monoxide poisoning, and whiplash.
Our treatment program is unique from most other clinics in two key ways:
-
Use of Functional Neurocognitive Imaging (fNCI): Unlike CT and normal MRI scans, our advanced fMRI scan maps how different brain regions are functioning and communicating with each other, allowing our team to identify the exact areas of brain dysfunction for each patient and tailor treatment accordingly.
-
Coordinated multidisciplinary treatment under one roof: Many TBI patients have frustrating experiences piecing together care through different providers and therapists who don’t coordinate with each other. They often have to wait weeks between appointments, and progress is slow to nonexistent. At Cognitive FX, our multidisciplinary team includes a clinical psychologist, a neurosurgeon, a neuroradiologist, neuroscientists, neuromuscular therapists, cognitive therapists, occupational therapists, and others—all of whom coordinate closely to optimize care for each patient on an accelerated treatment schedule.
Note: We are also the only post-concussion clinic we know of with third-party validated, peer-reviewed outcome data showing that our treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants.
Patient Evaluation
Every treatment begins with an in-depth assessment, including:
-
A meeting with one of our doctors to review the patient’s medical history and symptoms.
-
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
-
A psychological evaluation to identify symptoms of anxiety, depression, and other mental health problems.
-
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
-
A brain imaging scan called Functional Neurocognitive Imaging (fNCI) to determine where and how the patient’s brain was affected by the injury.
The fNCI Scan
We use Functional Neurocognitive Imaging (fNCI), which measures two key things:
-
Regional brain activity: How much oxygen each brain region uses during specific cognitive tasks (indicating underactive, normal, or overactive function).
-
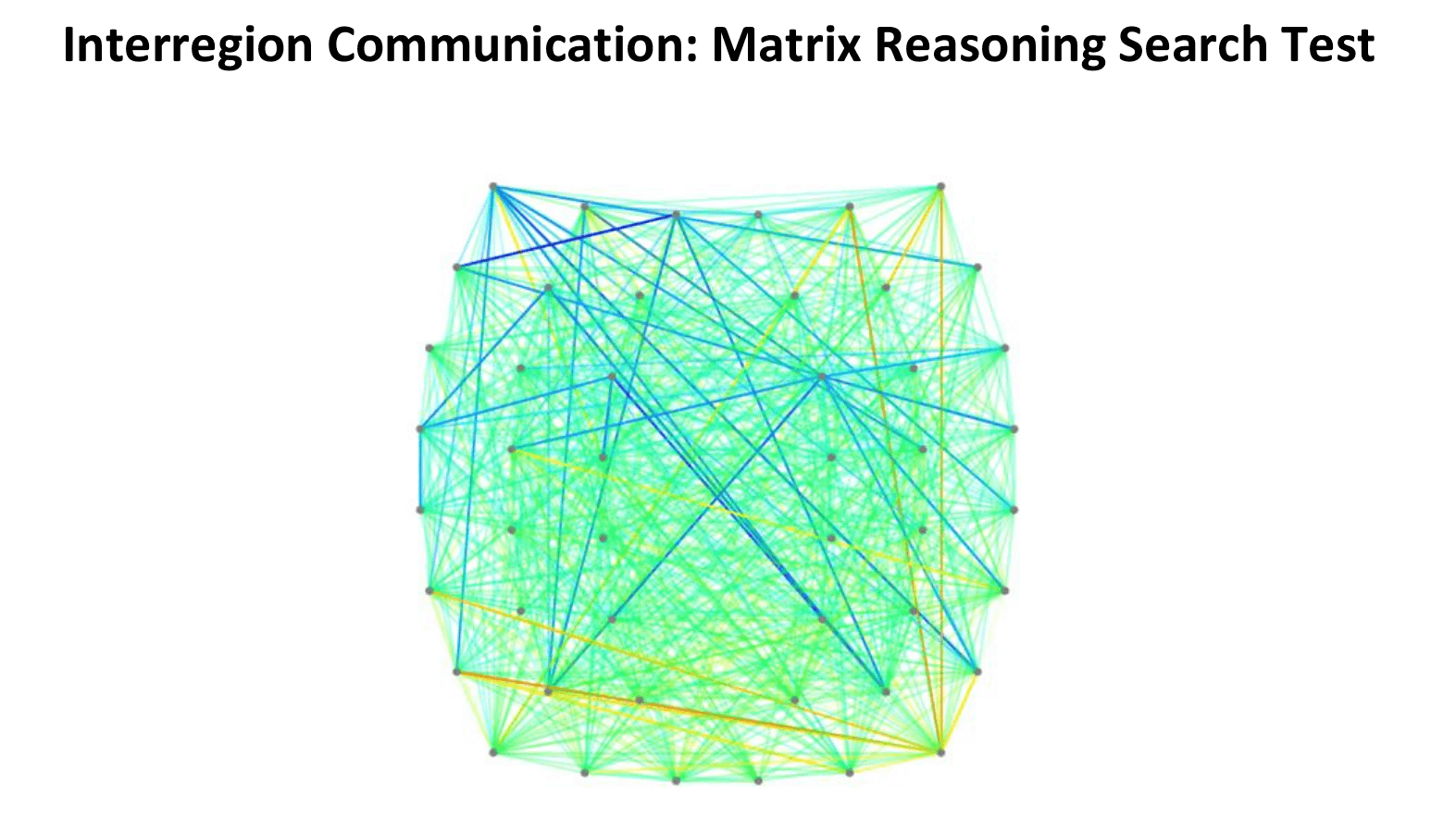
Connectivity between regions: How well different parts of the brain communicate with each other.
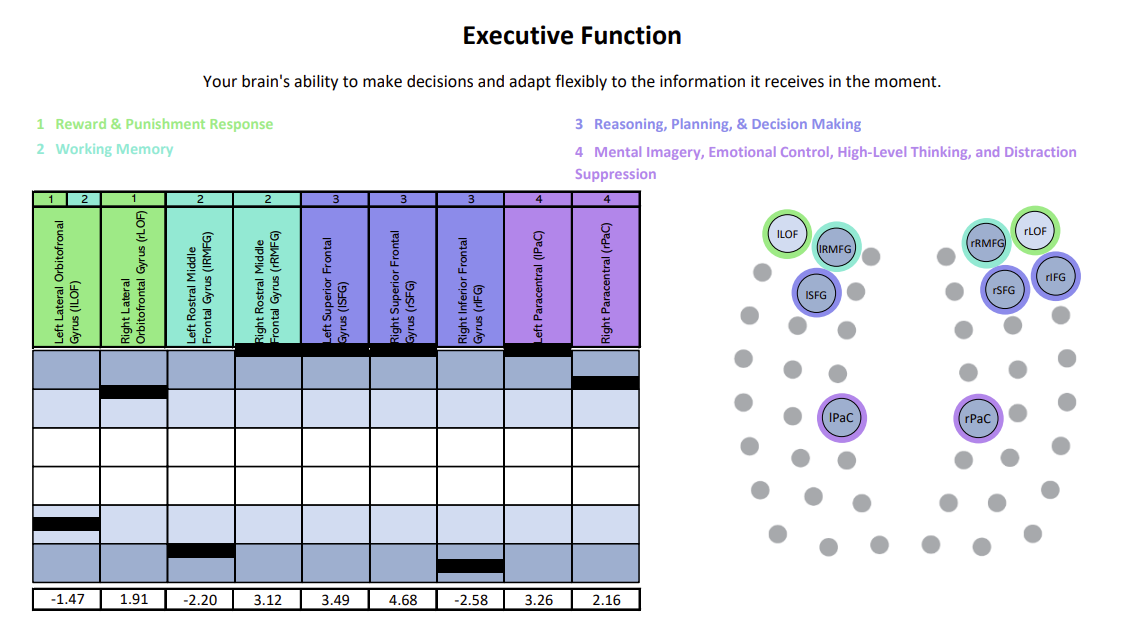
The scan results are visualized through intuitive charts and brain maps that help us identify whether a patient is experiencing hypoactivity (under-functioning), hyperactivity (over-functioning), or a mix of both—and where.
This detailed view of brain function allows us to tailor each person’s therapy precisely.
For example:
-
Someone with hypoactivity may need therapies that target various brain regions with stimulation and cognitive endurance training.
-
Someone with hyperactivity may benefit from therapies that reduce neural “noise” and promote regulation.
We’ve organized scan results for regional activity into six clear cognitive domains—like memory, attention, and executive function—to make them easier to understand and better guide individualized treatment.
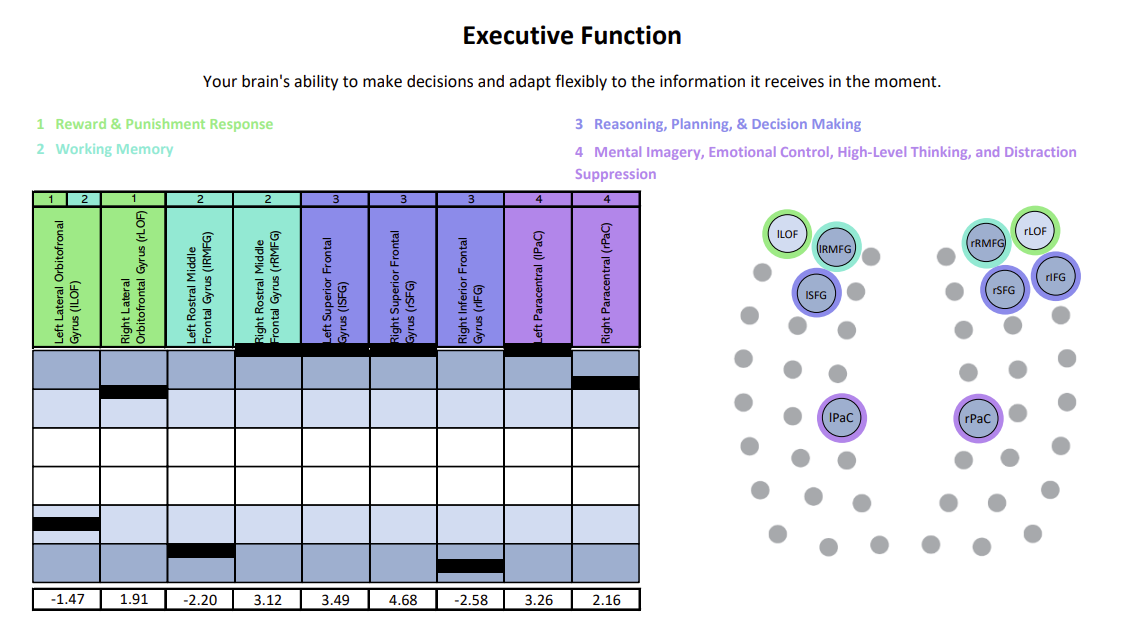
Each chart shows how specific brain regions are functioning compared to a normal brain. The white area represents the normal range, with the center line marking the average. Light and dark blue zones show increasing levels of abnormality. A black line marks the patient’s result for that region—ideally landing within the white. Lines in the light and dark blue zones suggest that region is either hyperactive (blue zones above the white) or hypoactive (blue zones beneath the white). In this example, the patient was experiencing both hypoactivity and hyperactivity within different key regions linked to executive function.
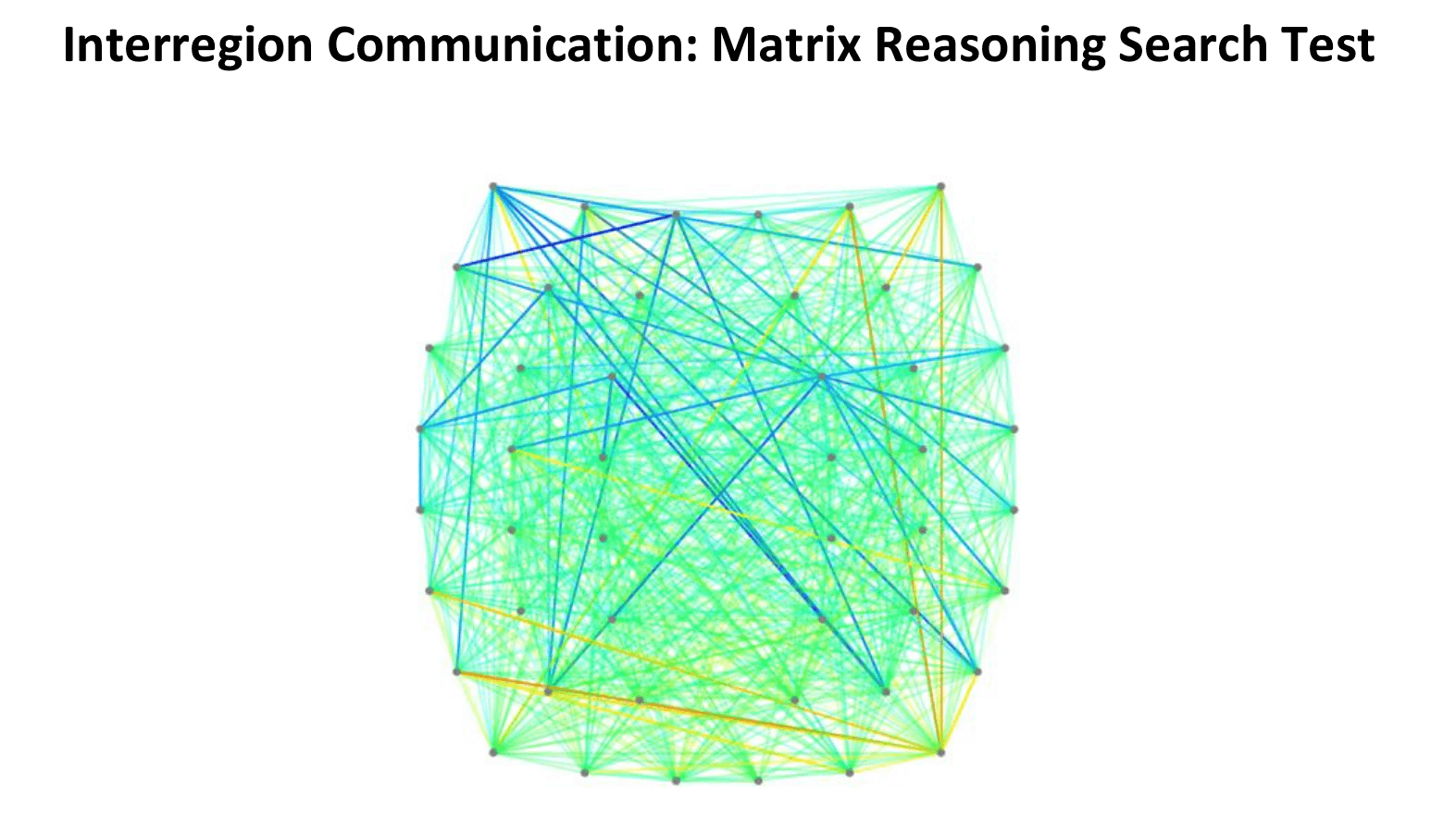
In this connectivity map, cooler colors (blues) indicate areas of hypoactivation (underactivity), while warmer colors (reds, oranges, yellows) indicate areas of hyperactivation (overactivity).
What Treatment Involves
After patients complete this evaluation, our team combines all the information and designs a customized treatment plan to target exactly the areas of the brain that show dysfunction for each patient.
Our brain injury treatment involves a three-step cycle that repeats: Prepare, Activate, and Recover.
Prepare

Therapy starts with short bursts of aerobic exercise, usually on the treadmill or stationary bike. As described earlier, exercise triggers the release of important chemicals in the brain, which help the patient's brain become more flexible and boost the effects of subsequent therapy.
Our therapists are trained to help patients exercise according to their needs without triggering severe symptoms. Even patients who struggle with physical activity due to balance problems can make remarkable progress in these sessions.
Activate

After exercise, patients attend a variety of therapies, including cognitive therapy, sensorimotor therapy, neuromuscular therapy, Dynavision therapy, occupational therapy, neurointegration therapy, vision and vestibular therapy, and psychotherapy, to name just a few. Patients receive all or most of these therapies during their visit, but the exact regimen for each one is unique to them.
Our therapists often combine exercises from different disciplines for greater effect.
For example, you might balance on a Bosu ball to engage your vestibular system and brain’s balance center while tossing color-coded tennis balls to work hand-eye coordination and reflexes. Meanwhile, you’ll add or subtract from a running tally based on which ball you catch, challenging memory, problem-solving, and attention.
During neurointegration therapy, you might draw a mirror image of a pattern while answering simple questions from your therapist.
Recover
Rest periods are an important part of our treatment. Some examples of scheduled brain breaks include:
-
Neuromuscular massage: Therapists massage the neck and shoulders to relieve chronic pain and tension, relax muscles involved in vision, improve circulation, and alleviate headache pain.
-
Brainwaves: The binaural beats app we use produces two frequencies that are very close together. If you listen to a different frequency in each ear, your brain will average them together to produce one frequency. We set the parameters so that the frequency your brain creates is the same frequency you would experience through meditation. This frequency will propagate in your brain waves as you listen. As a result, you gain some of the restorative benefits of meditation without being a meditation expert.
-
Mindfulness: Patients learn mindfulness techniques during their time at the clinic.
At the end of treatment, patients undergo a follow-up brain scan to check on their progress. Then, they meet with one of our therapists to review the results and receive a series of at-home exercises. These typically include physical activities, cognitive tasks, visual and vestibular exercises, and relaxation techniques. We recommend patients perform these exercises for about an hour, five times a week initially, with the frequency decreasing as symptoms improve.
For patients needing further therapy, we provide referrals to appropriate specialists.
Final Thoughts
Sexual dysfunction after a TBI is common but often overlooked due to stigma. It can stem from direct brain injury, hormonal changes, emotional struggles, or other TBI-related symptoms.
The good news is that help is available. With the right medical evaluation, therapy, and neurorehabilitation, many patients experience significant improvements in both their sexual health and overall quality of life.
Over 90% of our patients experience significant recovery after treatment in our clinic. To determine if our program is right for you, please schedule a consultation with our team.









.png?height=175&name=childhood%20head%20injuries%20(11).png)


