Most patients recover fully from a transient ischemic attack (TIA) — a term often used interchangeably with "mini-stroke" — within a few days. However, TIAs can cause symptoms that last for months or even years.
If you or a loved one has suffered a TIA, understanding both acute short-term recovery and therapies for longer-term symptoms is crucial.
This article provides an overview of the TIA recovery process, including:
If you’ve been suffering from lingering symptoms after a TIA, you’re not alone and you’re not imagining it. TIA can cause persistent symptoms that won’t resolve without treatment. 95% of our patients experience statistically verified restoration of brain function after treatment at our clinic. Book a free consultation with our team to learn if we can help you.
The Process of Recovering From a Mini-Stroke
Transient ischemic attacks (TIAs) resolve on their own, so no specific treatments are required during the event. The recovery process varies based on factors such as the severity of the episode, the patient’s overall health, and other medical conditions.
It is crucial for patients to seek medical attention promptly to implement preventative measures and reduce the risk of a future stroke. While most patients recover fully, a small percentage may experience lingering symptoms, such as memory loss, balance issues, vision or speech problems, and emotional challenges. These individuals often benefit from multidisciplinary therapy tailored to their needs. Close collaboration between healthcare providers and patients is vital for achieving the best outcomes.
Immediate Evaluation at the Hospital
The recovery journey starts as soon as patients seek medical care after their TIA. This is crucial to prevent and minimize long-term or permanent damage.
Here are some of things patients can expect at the hospital:
-
Immediate evaluation: Once admitted, doctors thoroughly evaluate the patient’s symptoms to determine the extent of the damage and decide on the appropriate treatment.
-
Diagnostic tests: The only way to differentiate between a TIA and a full stroke is through a comprehensive evaluation by a doctor. This assessment may involve a brain imaging scan, such as a CT scan or MRI. If significant damage is suspected, doctors may also order an ultrasound or echocardiogram to check for blockages or plaque in the patient’s arteries.
-
Monitoring: The healthcare team closely monitors patients to ensure that their blood pressure, heart rate, and oxygen levels remain stable. These values help determine the best course of action, which may include continuous monitoring with an ECG machine or telemetry.
-
Referral for further treatment: Patients may be referred to a specialist for additional evaluation and treatment. This is likely to be a cerebrovascular neurosurgeon, who will perform a series of diagnostic tests to evaluate the underlying cause and severity of the mini-stroke.
Preventative Measures
Recovery also involves preventative measures to reduce the risk of a moderate or severe stroke after a TIA. These measures can include:
-
Medication for stroke prevention: Most patients who experience an ischemic stroke or TIA will need medication to reduce the risk of another TIA or a more serious stroke. Examples include antiplatelet drugs and anticoagulants to reduce the risk of forming blood clots, hypertensive medication to manage high blood pressure, and statins to lower cholesterol.
-
Surgical interventions: For some patients, the best option to prevent future strokes is a carotid endarterectomy, which removes fatty acid deposits and part of the lining of the carotid arteries that may be constraining blood flow. Another common procedure is angioplasty, which uses a balloon-like device to open a clogged artery, followed by a stent to keep it open.
Rehabilitation and Supportive Therapies
Dedicated rehabilitation and supportive therapies are some of the most important aspects of mini-stroke recovery. Physical, occupational, and speech therapy, for example, offer tailored exercises and activities to help patients recover from specific post-TIA symptoms.
Some supportive therapies that can help TIA patients include:
-
Physical Therapy: After an initial assessment, a physical therapist can determine your needs and develop a plan to help you return to your normal daily activities. Typical exercises include aerobic training, such as walking, cycling, or aquatic therapy to help patients regain strength and mobility. Physical therapists also play an important role in educating TIA patients about the importance of physical activity, blood pressure control, smoking cessation, a healthy diet, recognizing a stroke, and when to seek immediate medical assistance.
-
Occupational Therapy: Occupational therapy is another type of therapy that can help patients develop their skills and confidence to manage daily activities. This includes, for example, suggesting physical exercises to practice, helping patients find new ways of doing things, or suggesting equipment that could help.
-
Cognitive Therapy: After a TIA, about half of patients report having subtle cognitive and communication problems, including problems with attention, memory, fatigue, reading, and participating in conversations which can last for months after the incident. These patients may benefit from cognitive therapy to help improve these functions. Typically, these include exercises to train memory, attention, problem-solving skills, and executive function, to name just a few.
-
Speech and Language Therapy: A TIA can affect patients’ abilities to communicate with others, including slurred speech, difficulty finding words, and struggle to focus on conversations. It may also cause problems swallowing. Speech therapists provide personalized exercises to help patients recover their speech and communication skills.
-
Vision Therapy: Although vision problems typically improve over time, some patients may benefit from vision therapy to help with this process. Ideally, therapy should start as soon as possible after the TIA to minimize the impact visual problems can have on your daily life. Sessions should be customized to each patient, but typical exercises include ways to help with double vision, visual field loss, and eye coordination.
-
Counseling: Counseling helps patients discuss how the TIA has impacted them, focusing on recovery, managing health, setting goals, risk factors, and making lifestyle changes to prevent future strokes. Counselors can also assist in identifying support systems.
Recovering at Home
While a mini-stroke can be scary, it’s important to remember that it’s often a wake-up call, not a final warning. The good news is that TIAs themselves don’t typically shorten life expectancy, giving you time to take proactive steps to prevent a more serious stroke in the future. By making positive lifestyle changes, you can significantly reduce your risk and potentially avoid a major stroke altogether.
Here are some tips that may help:
-
Embrace a healthy lifestyle: Leading a healthy lifestyle can significantly reduce the risk of a repeat incident. Patients should prioritize regular exercise and follow a balanced diet low in saturated fats and sodium.
-
Take medication as prescribed: After a TIA, patients are often prescribed medication to manage their blood pressure, cholesterol levels, and other underlying conditions. It’s crucial to take this medication as prescribed.
-
Manage stress: Stress can be a significant risk factor for a stroke. Patients should take steps to reduce stress, such as practicing relaxation techniques like meditation, yoga, or tai chi.
-
Stay vigilant: Patients should stay informed about the warning signs of a stroke and seek medical attention immediately if they experience any symptoms.
-
Join a support group: Support groups provide fellowship with other patients in similar situations and who understand exactly what you’re going through. They can offer suggestions, resources, social opportunities, and friendship.
-
Go easy on yourself: Full recovery may take time, especially for patients with lingering symptoms. You may have less energy than before your TIA and struggle with everyday activities. Feeling overwhelmed and stressed can also be draining. Plan to ease back into life slowly and ask for help from family and friends if needed.
What to Avoid After a TIA to Help with Recovery
The journey to recovery also involves knowing what not to do, including:
-
Smoking: Continuing to smoke after a TIA doubles the risk of another TIA or stroke and increases mortality rates. The good news is that smoking cessation, through nicotine patches, gum, or inhalers, along with counseling, can help TIA patients quit and reduce their stroke risk.
-
Consuming high amounts of alcohol: Heavy alcohol consumption raises blood pressure, triggers atrial fibrillation (a stroke risk factor), and damages the liver, affecting blood clotting. After a TIA, patients taking medications should consult a doctor to determine if drinking alcohol is safe.
-
Maintaining excessive weight: Obesity increases the risk of a TIA or a stroke by 50% to 100%. Losing as little as 5% to 10% of body weight can significantly reduce stroke risk.
-
Ignoring risk factors: Hypertension, inactivity, poor diet, obesity, excessive alcohol consumption, and smoking are major risk factors for TIA. Ignoring these increases the likelihood of another TIA or stroke, but the danger can be minimized by adopting healthy behaviors. For example, hypertension can be treated with medication or reduced with a low-sodium diet, while high cholesterol can be managed with medication or a diet rich in fiber and low in saturated fats.
How Long Does It Take to Recover From a TIA?
Most people recover quickly from a transient ischemic attack, with effects typically lasting from a few minutes to a few hours, resolving within 24 hours.
With that said, symptoms of a mini-stroke can persist for weeks or months. In some cases, short-term treatments may not be sufficient. Some patients experience worsening or new symptoms, while others may not find relief from acute therapies, which are often done in isolation.
These patients may experience:
- Fatigue
- Cognitive difficulties
- Difficulty focusing
- Poor memory
- Depression
- Anxiety
- Physical weakness
- Visual impairments
- Impaired speech
- Mood swings
- Moderate to severe headaches
If patients are experiencing some of these symptoms, they may find it harder to return to their daily activities, including work and family commitments, and experience a lower quality of life.
After a stroke, there are many services in place to help patients recover. After a TIA, however, patients are often quickly discharged from health services and have limited access to follow-up support services. Patients can feel abandoned and dissatisfied with their care, particularly due to a lack of communication, follow-up, rehabilitation options, and personalized support.
At Cognitive FX, we recognize the importance of treating these patients, many of whom were never actually informed that their TIA could cause long-term symptoms when they were first treated at their local hospital.
How TIAs Cause Long-Term Effects
.png?width=1200&height=881&name=TIA%20(1).png)
In a previous post, we explained how and why TIAs can cause lasting after-effects. Here, we’ll dive deeper into the mechanisms behind these long-term impacts.
During a TIA, a blood clot restricts or blocks blood flow to specific parts of the brain, depriving them of essential resources like oxygen and energy. Although the clot eventually dissolves and blood flow resumes, the brain doesn’t always fully recover.
Functional MRI (fMRI) studies show that even when patients are at rest, their brains often look and function differently from those of healthy individuals.
Even brief interruptions in blood flow can disrupt neurovascular coupling (NVC), a key mechanism in the brain. In a healthy brain, nerve cells signal nearby blood vessels to deliver resources exactly where and when they’re needed. When a TIA interrupts this process, affected brain areas struggle to perform their tasks due to resource deprivation.
This disruption can lead to clusters of dead cells, especially in deeper brain regions where smaller blood vessels branch from the carotid arteries. Once the clot dissolves, fragments can travel further into smaller capillaries, causing additional blockages and cell death. Over time, these clusters of dead cells — often visible as tiny white dots on MRI scans — can accumulate. While a neuroradiologist might classify them as “nonspecific findings” since they’re not immediately life-threatening, these cells once played critical roles in brain function.

In this figure, we see a patient before (A) and after (B) a TIA caused a small cluster of dead brain cells. [Source]
The result? Lingering physical and cognitive symptoms, such as memory problems, difficulty concentrating, and motor issues. Recovery involves retraining the brain to reroute communication around damaged areas and restore healthy neurovascular coupling.
At our clinic, we specialize in helping patients achieve this recovery. Using advanced imaging and tailored therapies, we address the long-term effects of TIAs and other brain injuries, empowering patients to regain function and quality of life.
Treating TIAs Long-Term Symptoms at Cognitive FX
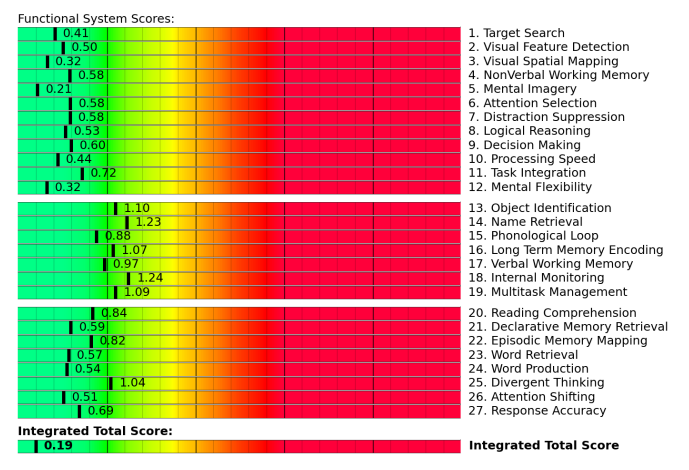
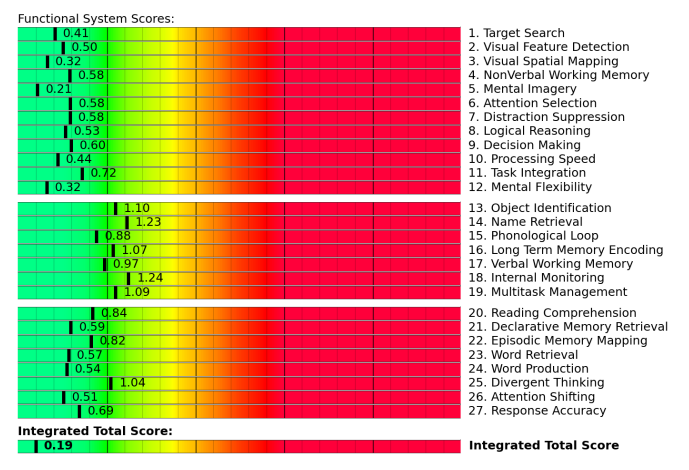
Before treatment starts at Cognitive FX, our team assesses each patient’s medical history and symptom profile. Patients also undergo a series of assessments to test physical, cognitive, and emotional abilities.
As part of this process, patients undergo a brain imaging scan called functional neurocognitive imaging (fNCI) to determine how and where the TIA affected their brain function. This scan measures blood flow in approximately 100 different brain regions to reveal how these areas communicate with each other while the patient carries out a series of standardized cognitive tasks. Combining all this information enables our team to design a customized treatment plan targeting the areas most affected by the TIA.
Example of fNCI results for a stroke patient (scores in red and yellow indicate areas of poor neurovascular coupling):

For comparison, fNCI results from a patient with healthy neurovascular coupling:
These are the two characteristics of Cognitive FX that set our clinic apart from other therapy options and allow us to consistently help our patients achieve significant improvements in their symptoms:
-
State-of-the-art brain imaging scan: The fNCI scan provides detailed insights into brain health, allowing us to tailor treatment. For example, if the scan shows poor sustained attention, our therapists can focus on exercises targeting this function during treatment week.
-
Multidisciplinary team under one roof: While most patients must visit different doctors and therapists who may not communicate or coordinate with each other, our multidisciplinary team works closely together to ensure seamless treatment. We even use a Slack channel to share notes on each patient's response, session adjustments, and considerations for other therapists.
During treatment, patients follow an evidence-based, three-step cycle repeated several times per day: Prepare, Activate, and Recover. The goal is to restore normal neurovascular coupling, recover proper autonomic nervous system function, and reduce the incidence and severity of long-term symptoms from the TIA.
Prepare
Typically, sessions start with aerobic exercise, usually on a treadmill or stationary bike. Exercise triggers the release of important neurochemicals, including a compound called brain-derived neurotrophic factor (BDNF). BDNF promotes the growth of brain cells and improves communication between different areas of the brain. In turn, this helps the patient's brain become more flexible and boosts the effect of subsequent therapy.
Even patients who struggle with physical activity can make remarkable progress in these sessions. Our therapists are trained to help patients exercise without triggering severe symptoms.

Activate
After exercise, patients attend a variety of therapies, including cognitive therapy, sensorimotor therapy, neuromuscular therapy, Dynavision therapy, occupational therapy, neurointegration therapy, vision and vestibular therapy, and psychotherapy, to name just a few. Patients receive all or most of these therapies during their visit, but the exact regimen for each one is unique to them.
Many sessions include cross-disciplinary exercises. For example, our therapist may ask patients to balance on a Bosu ball, toss color-coordinated tennis balls back and forth, and name an animal for each letter of the alphabet, at the same time. This forces the brain to activate areas involved in balance, hand-eye coordination, and word recall while encouraging healthy neurovascular coupling.
Recover
The final step involves activities designed to help patients relax and recover between therapies. These may include neuromuscular massage for the neck and shoulders, breathing and mindfulness exercises, and listening to Brainwaves, which work similarly to meditation.
At the end of treatment, patients undergo a second brain imaging scan to check on their progress. They then meet with one of our therapists to review the results and receive a series of at-home exercises. These typically include physical activities, cognitive tasks, visual and vestibular exercises, and relaxation techniques. We recommend patients perform these exercises for about an hour five times a week initially, with the frequency decreasing as symptoms improve. For patients needing further therapy, we provide referrals to appropriate specialists.
Schedule a consultation with our team to determine if our program is right for you.

.png?width=1200&height=881&name=TIA%20(1).png)






.jpg?height=175&name=Slow%20Concussion%20Recovery%20(6).jpg)




