After experiencing a transient ischemic attack (TIA) — often called a mini-stroke — it’s common to struggle with persistent physical and mental fatigue. This exhaustion can significantly impact daily life, making it difficult to wake up refreshed, stay productive, or even complete routine tasks.
While medications, therapy, and lifestyle changes can help manage fatigue, many TIA patients have underlying brain dysfunction that often goes untreated. When the brain is not functioning optimally, standard treatments may only provide limited relief.
In addition, post-TIA fatigue is rarely an isolated issue. Many patients also experience headaches, brain fog, vision problems, sleep disturbances, and more, making recovery even more challenging.
The most effective way to treat post-TIA fatigue is a multidisciplinary approach that targets the root cause: brain dysfunction that contributes to exhaustion and other lingering symptoms.
In this article, we’ll cover:
What Is It Like to Live with Post-TIA Fatigue?
Fatigue is one of the most common and persistent challenges after a transient ischemic attack (TIA). Studies suggest that 30% to 60% of TIA patients experience ongoing tiredness, with about one-third of these individuals reporting severe fatigue that significantly impacts their daily life. Alarmingly, many continue to struggle with these symptoms for over a year.
Patients often describe post-TIA fatigue as overwhelming and unrelenting — a type of exhaustion that doesn’t improve with rest. Many wake up feeling just as drained as when they went to sleep, as if their body and brain never fully recharge. As the day progresses, their energy depletes even further, eventually forcing them to stop and rest.
The way fatigue manifests varies from patient to patient:
-
Some feel constant exhaustion, while others experience fatigue that worsens after activity (physical or mental).
-
Some struggle with mental fatigue, feeling drained after cognitive tasks like reading or answering emails.
-
Others experience physical fatigue, becoming exhausted after brief periods of exercise or exertion.
-
Many have fluctuating symptoms, with good days where they feel functional and bad days where they feel incapacitated.
Not surprisingly, this level of fatigue makes it difficult to return to work, enjoy daily activities, or maintain relationships. Friends and family may misunderstand or underestimate how severe the exhaustion is, leading to frustration and isolation. Additionally, many patients struggle to fully participate in rehabilitation because they simply don’t have the energy to keep up with therapy.
As a result, post-TIA fatigue is linked to higher rates of depression, reduced physical function, lower quality of life, and even increased mortality. Understanding and properly managing this fatigue is crucial to improving long-term recovery and well-being.
Symptoms of Post-TIA Fatigue
Post-TIA fatigue can cause a variety of physical, cognitive, and emotional changes and symptoms, including:
Cognitive Symptoms
- Brain fog
- Difficulty with cognitive skills, including communication, thinking, and focus
- Memory loss (especially short-term memory problems)
- Decreased awareness of surroundings
- Difficulty communicating (aphasia)
Emotional Symptoms
- Apathy or lack of enthusiasm
- Anger or irritability
- Difficulty regulating emotions
- Feeling cynical or pessimistic
- Increased negative thoughts
- Feelings of depression and anxiety
Physical Symptoms
- Persistent tiredness
- Headaches
- Sleep disorders
- Weight changes
- Digestive problems
- Shortness of breath
- Slow speech
- Decreased coordination
In addition, post-TIA fatigue can worsen other symptoms, such as physical weakness, memory problems, and difficulty with focus and concentration. Some patients become anxious or fearful, mistaking their heightened symptoms for signs of another TIA or even a full ischemic stroke.
What Causes Fatigue After a TIA?
Post-TIA fatigue is rarely caused by a single factor. Instead, it typically results from a combination of underlying issues, including:
- Neurovascular coupling (NVC) dysregulation
- Autonomic nervous system (ANS) dysfunction
- Sleep disturbances
- Depression and anxiety
- Other TIA-related symptoms
- Side effects of medication
Each of these factors can contribute to ongoing physical and mental exhaustion, making it essential to address them holistically.
1. Neurovascular Coupling (NVC) Disruption
During a TIA, a temporary blockage in blood flow deprives certain brain areas of oxygen and nutrients. While the clot typically dissolves on its own, even brief interruptions can disrupt neurovascular coupling (NVC) — the brain’s mechanism for efficiently directing blood flow to areas that need it most.
In a healthy brain, neurons signal nearby blood vessels to deliver oxygen and energy where needed. However, after a TIA, this process can become inefficient. The affected brain regions must work harder to complete even simple tasks, leading to increased energy consumption and persistent fatigue.
2. Autonomic Nervous System (ANS) Disruption
The Autonomic Nervous System (ANS) controls vital functions such as heart rate, blood pressure, and digestion. It has two key subsystems:
-
Sympathetic nervous system (SNS) — Triggers the “fight or flight” response, using energy.
-
Parasympathetic nervous system (PNS) — Activates the “rest and digest” response, restoring energy.
Normally, the SNS and PNS balance each other to regulate energy use. However, after a TIA, the SNS often remains overactive, keeping the body in a constant state of stress and alertness. This drains energy reserves, making patients feel persistently fatigued.
3. Sleep Disturbances
Up to 20% of TIA patients experience sleep problems, which further contribute to fatigue. Common causes include:
- Brain injury effects disrupting sleep regulation
- Changes in daily activities and routines after a TIA
- Medication side effects
- Pain or discomfort
- Emotional distress, such as anxiety or depression
Because sleep quality is often poor, many patients wake up feeling just as exhausted as when they went to bed. This leads to a cycle of daytime drowsiness and frequent naps, which can further disrupt sleep patterns.
4. Depression and Anxiety
TIA survivors often face heightened emotional distress, including anxiety about their health, fear of another stroke, and lifestyle limitations. Many also experience depression, particularly if they struggle with ongoing symptoms or reduced independence.
These emotional challenges can trigger:
- Increased mental exhaustion due to constant worry
- Disrupted sleep patterns, leading to further fatigue
- Reduced motivation for physical activity and self-care
The combination of stress, uncertainty, and emotional strain can leave patients feeling mentally and physically drained.
5. Other TIA-Related Symptoms
Beyond fatigue, TIA patients often experience other lingering symptoms, such as:
- Headaches
- Muscle weakness
- Brain fog and difficulty concentrating
- Sleep disturbances
These symptoms can intensify fatigue by making daily activities more mentally and physically taxing. Additionally, some patients avoid physical activity due to pain or fear of overexertion, leading to deconditioning and lower fitness levels — which, in turn, worsens fatigue.
6. Medication Side Effects
Certain medications prescribed after a TIA can contribute to fatigue. Common culprits include:
- Beta blockers (for high blood pressure)
- Antidepressants
- Epilepsy medications
If you suspect that medication is making your fatigue worse, consult your doctor. Adjustments to dosage or switching to an alternative medication may help.
How Post-TIA Fatigue Is Commonly Treated
For most patients, post-TIA fatigue improves with time, but it’s impossible to predict how much it will improve or how long it will take. TIA and stroke recovery varies greatly from patient to patient. Additionally, it can be challenging to find a suitable treatment, but there are some options available.
Common treatments include:
- Medication
- Psychotherapy
- Lifestyle changes
1. Medication Options
Doctors have had very little success treating fatigue and lack of energy with medication. Often patients try different prescription and over-the-counter drugs, but don’t experience any real benefits. For example, patients may be prescribed narcolepsy drugs because they’re constantly napping during the day, but that doesn’t really improve their fatigue.
The only exception that can address fatigue directly is a prescription drug called modafinil, which is a neuroendocrine regulator and wakefulness-promoting agent. There are no studies with TIA patients, but stroke patients reported less fatigue and better quality of life after taking this drug for 6 weeks.
Other medications can be used to address specific symptoms which may be causing fatigue:
-
Sleep problems: In TIA patients, melatonin can help patients sleep better at night, which in turn helps them wake up more refreshed and less fatigued. If you want to give melatonin a try, consider a small dose (such as 0.5 mg), and slowly work your way up to a dose that works for you.
-
Depression and anxiety: Antidepressants don’t cure fatigue, but can address emotional problems, which in turn can help patients sleep better.
2. Therapy and Rehabilitation
In contrast to medication, there is some evidence to support the use of various forms of therapy to help patients after a minor stroke. These should not be seen as a cure, but part of a wider treatment plan to help patients cope with their symptoms, including fatigue.
Some of these include:
-
Cognitive Behavioral Therapy (CBT): Studies assessing the efficacy of CBT to treat fatigue show favorable results. Sessions typically cover ways to conserve energy during the day, reorganize daily schedules, establish a healthy sleep routine and develop strategies to deal with physical and mental fatigue.
-
Cognitive and graded activity training (COGRAT): This form of therapy combines cognitive therapy and physical exercise. Results show that combining exercise and cognitive activities is more effective at reducing fatigue than either type of therapy in isolation.
-
Physical therapy: Engaging in regular exercise with the help of a physical therapist improves fitness, which in turn can help reduce fatigue in TIA patients.
-
Educational fatigue management: There is some evidence that support groups and education programs can help patients manage their symptoms, including fatigue. For example, patients reported feeling better and less tired after a few sessions discussing sleep hygiene and relaxation exercises.
3. Lifestyle Adjustments
Certain lifestyles, such as being sedentary, following a poor diet, or not sleeping enough, can make patients feel tired and have less energy. As such, the most common advice for patients experiencing high levels of fatigue involves lifestyle changes.
Some of these changes include:
Better Sleep Hygiene
Lack of sleep at night and sleepiness during the day can affect your cognition, mood, energy levels, and even appetite. For TIA patients, maintaining a healthy sleep pattern is essential to recovering from and managing fatigue.
-
Go to bed and wake up at the same time, regardless of the day of the week. Establishing this routine allows your brain to “learn” when it’s time to sleep.
-
If you need it during the day, take a power nap (no longer than 30 minutes).
-
Pick a relaxing activity to do before bedtime, such as gentle yoga or reading a book.
-
Avoid using mobile phones and tablets in the evening.
-
Dim or switch off unnecessary lighting as you’re getting ready for bed.
Healthy Diet for Energy
Eating a high-fat, high-sugar diet can lead to fatigue. In addition, high sodium intake — common in highly processed foods — is closely associated with hypertension, one of the major risk factors for stroke. TIA patients should follow a healthy and balanced diet rich in fruits, vegetables, and nuts, while avoiding fatty and sugary processed foods.
Exercise & Movement
Exercise may be the last thing you want to do when you’re feeling drained, but it’s an essential way to increase your energy levels, improve your mood, and increase your overall physical well-being. You don’t need to engage for long periods or at a high intensity to notice benefits. Just do what you can, even if that means dancing to a fun song for five minutes a day and working up to more.
Stress Management
Reducing stress can reduce fatigue and improve mental and physical health. Find ways to limit, or even eliminate, sources of stress in your life. For example, if you feel overwhelmed in noisy situations, go shopping late in the evening or early morning when everything is quieter.
Other options include meditation and mindfulness, breathing exercises, yoga, tai chi, massage, and aromatherapy.
Daily Pacing & Energy Management
Learn to pace yourself during the day to avoid becoming overtired. If you’re at work, plan which tasks you need to complete according to your energy levels:
-
Complete tasks that require the most mental effort earlier in the day.
-
Set firm boundaries regarding working hours, and take breaks during the day.
-
Consider working from home, if possible.
-
Learn to identify what triggers your fatigue and avoid it if possible.
-
Develop brain strategies that can help you, such as using to-do lists and alarms to remind you of something important.
Taking Breaks & Resting
A few minutes to rest and recharge during the day can go a long way to stave off fatigue. Rest breaks don’t necessarily mean you need to sleep. A break could be any of the following:
-
Take a break from what you’re doing: Walk away from your computer for a few minutes, go outside if you can, or stop to eat a healthy snack.
-
Follow the 20-20-20 rule: Every 20 minutes, look at something that is 20 feet away for 20 seconds.
-
Find a distraction: Grab an adult coloring book or some scrap paper for doodling.
-
Switch tasks: Sometimes, just changing what you’re doing can function as a break if it uses different parts of the brain.
-
Enjoy a few minutes to yourself: Close your eyes and allow yourself to daydream for a few minutes.
-
Take short naps during the day: If you feel exhausted after a particular task, take a 20-minute power nap. However, avoid sleeping too much during the day as this will disrupt your sleep patterns at night, making you feel more fatigued.
-
Take a few minutes to hum, sing, or gargle: It may sound silly, but humming, singing, or gargling is one of the easiest ways to reduce anxiety, stress, and fatigue. The vagus nerve is a long nerve that goes from your brain down your neck, chest, and abdomen, essentially connecting the brain with the body. Activating this nerve by humming, singing, or gargling stimulates the parasympathetic nervous system, which in turn helps you relax and feel less tired.
-
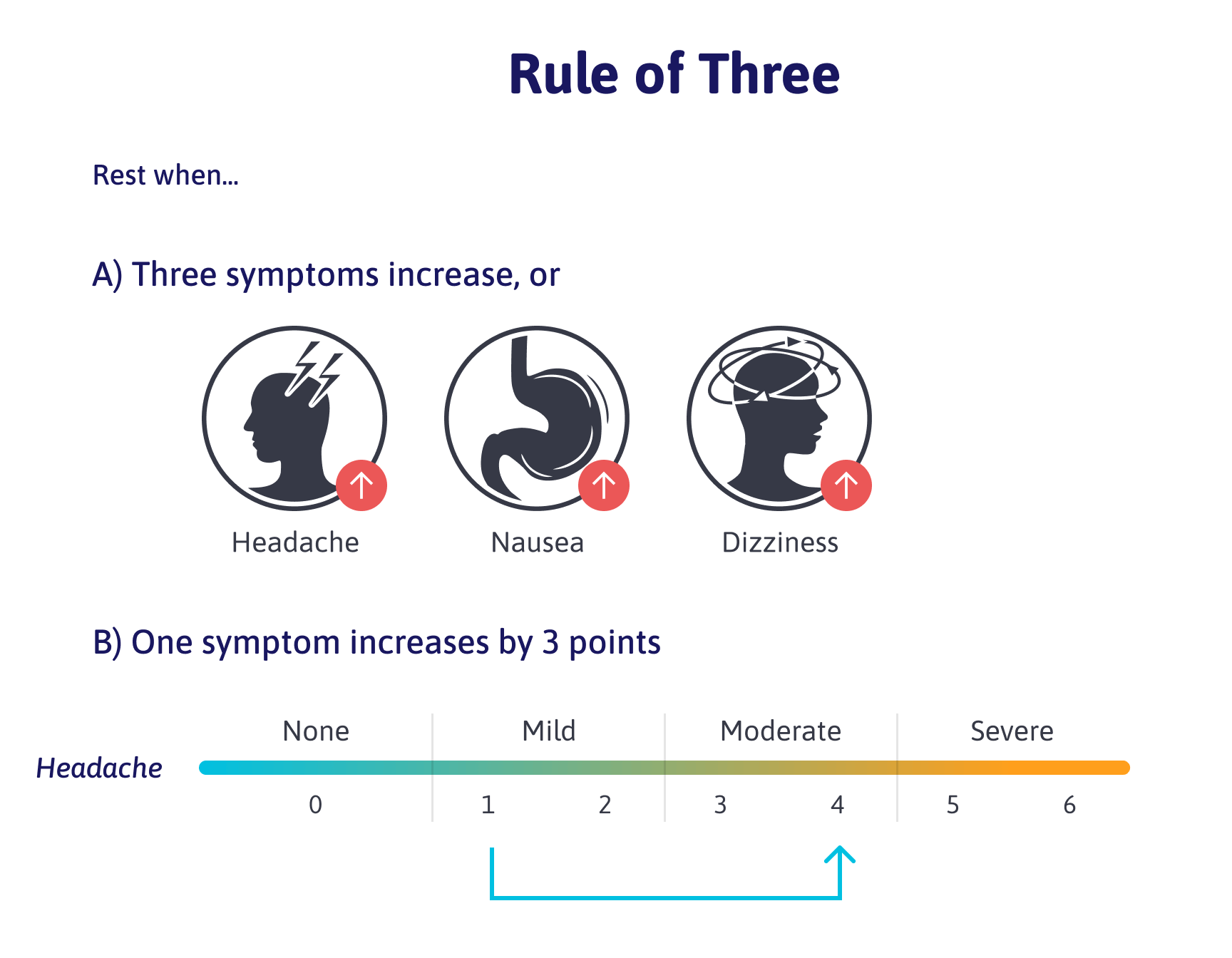
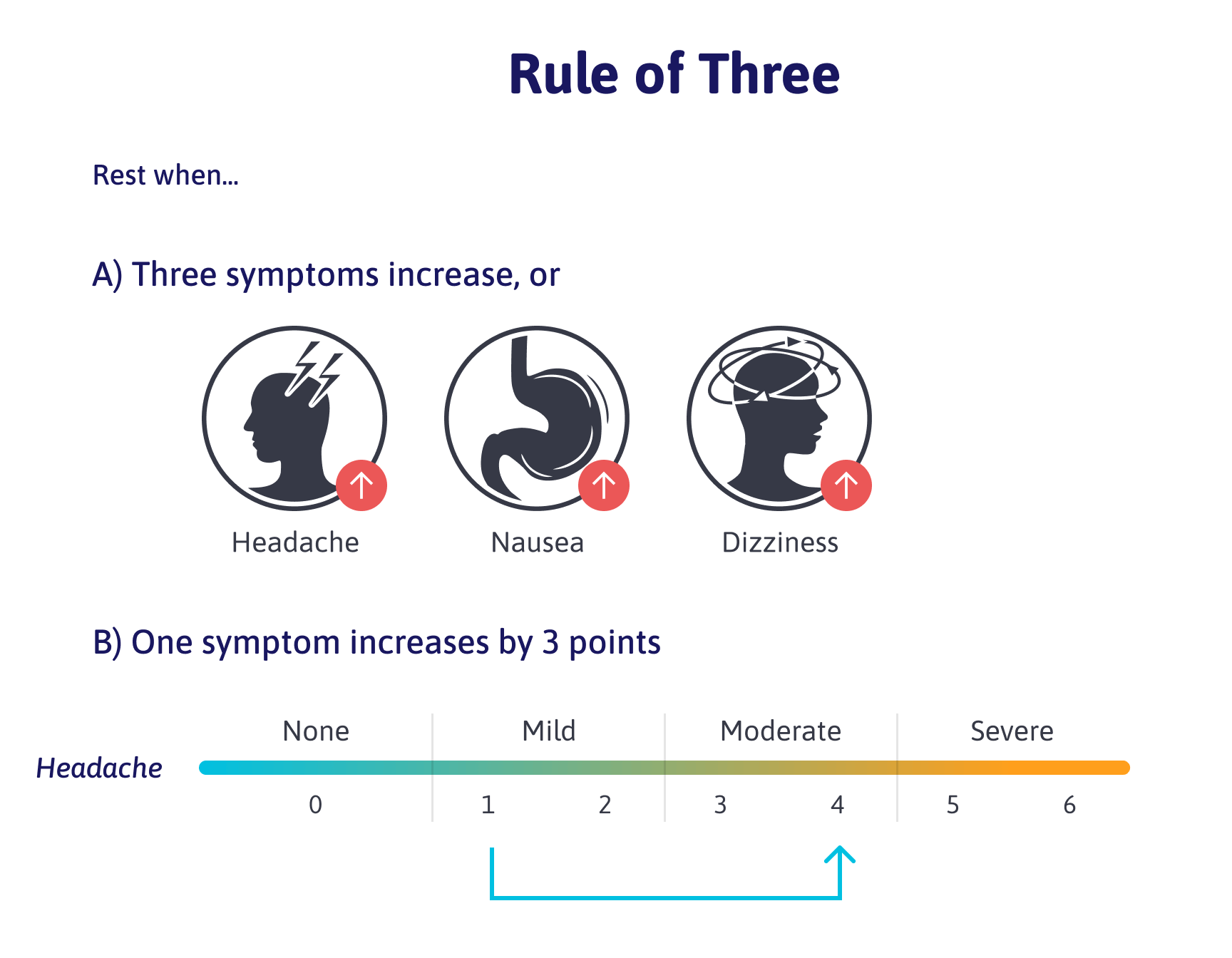
Follow the rule of three: If you notice either three different symptoms worsening at the same time or one symptom going from mild to severe (increasing by three points on a six-point scale), then it’s time for a break.
How Cognitive FX Helps Treat Post-TIA Fatigue
Many healthcare professionals lack the resources or specialized treatments needed to effectively manage post-stroke fatigue. Patients are often prescribed medications that provide little relief or given general lifestyle recommendations that don’t fully address the underlying problem. As a result, many people are left struggling with chronic exhaustion, forced to adapt rather than recover.
At Cognitive FX, we take a multidisciplinary approach to treat the root causes of fatigue, rather than just the symptoms. Our treatment program targets:
-
Neurovascular Coupling (NVC) Dysfunction, improving the brain’s ability to regulate blood flow and energy use.
-
Autonomic Nervous System (ANS) Dysfunction, helping restore balance between energy use and recovery.
-
Other contributing factors, such as sleep disturbances, depression, and cognitive impairments, which often worsen fatigue.
Many of our patients report feeling less fatigued and more energized after treatment because we focus on comprehensive brain rehabilitation — helping them regain control over their energy levels and overall well-being.
Step 1: Comprehensive Evaluation
Before treatment starts at Cognitive FX, our team assesses each patient’s medical history, symptom profile, and physical, cognitive, and psychological well-being.
This includes:
-
Physical performance, including reflex response, balance, hand-eye coordination, and so forth.
-
Cognitive abilities, such as memory, thinking, executive function, and problem-solving skills.
-
Emotional status, including signs of anxiety, depression, or other mental health conditions.
Patients also go through a special type of brain imaging scan, called functional NeuroCognitive Imaging (fNCI), to determine how and where the TIA affected their brain function. This scan assesses about 100 different areas in the brain and how those regions communicate with each other while the patient carries out a series of standardized cognitive tasks.
Example of fNCI results for a stroke patient (scores in red and yellow indicate poor neurovascular coupling):

fNCI results from a patient with healthy neurovascular coupling for comparison:

Combining all of this information allows our multidisciplinary team (made up of experts in neuroscience, neuropsychology, physical and occupational therapy, psychotherapy, and more) to design a customized treatment plan to target the parts of your brain that were most affected by the TIA.
These are the two characteristics of Cognitive FX that set our clinic apart from other therapy options and allow us to consistently help our patients see significant improvements in their symptoms. The fNCI scan gives us detailed insight into the patient’s brain health to customize treatment. For example, if we see from the fNCI scan that sustained attention is poor, then our therapists can work on more exercises to improve that specific function during treatment week.
Second, instead of being treated by doctors and therapists from different offices who don’t communicate or coordinate with one another (with appointments spread out over weeks or months at a time), our multidisciplinary team works closely together so that every aspect of treatment is tightly coordinated. We even have a Slack channel where we share notes throughout the day on how each patient is responding to therapy, what needs to change in an upcoming session, and anything the next therapist should consider.
Step 2: Multidisciplinary Treatment
During treatment week, patients go through an evidence-based, three-step cycle that is repeated several times a day: Prepare, Activate, and Recover. The goal is to restore normal neurovascular coupling, recover normal function of the autonomic nervous system, and reduce the incidence and severity of long-term symptoms from the TIA.

Prepare
Typically, sessions start with a period of aerobic exercise intervals (usually on a treadmill or stationary bike) to take advantage of a phenomenon in the brain called post-exercise cognitive boost (PECB). PECB triggers the release of chemicals in the brain, including a compound called brain-derived neurotrophic factor (BDNF). BDNF promotes the growth of brain cells and improves communication between different areas of the brain. In turn, this helps the patient's brain become more flexible and boosts the effect of subsequent therapy.
Patients who struggle with physical activity still make remarkable progress in these sessions. Our therapists are trained to work around exercise intolerance and to help patients recover without triggering severe symptoms.

Activate
After exercise, patients attend a variety of therapies, including:
Most patients receive all or most of these therapies during their visit, but the exact regimen for each person is unique to them. Many sessions often include cross-disciplinary exercises.
For example, our therapist may ask you to balance on a BOSU ball, toss color-coordinated tennis balls back and forth, and name an animal for each letter of the alphabet, all at the same time. This forces your brain to activate areas involved in balance, hand-eye coordination, and word recall while encouraging healthy neurovascular coupling.
Rest
The last step involves activities to help patients relax and rest between therapies. These periods may include:
-
Massage to relax: This includes, for example, neuromuscular massage on the neck and shoulders
-
Breathing exercises: We teach patients a series of breathing exercises to help reduce symptoms after physical exercise, calm down, and feel less tired. Studies show improved respiratory function and overall well-being in stroke patients who practice intentional breathing patterns several times a week. This is because breathing, emotion, and cognition are all closely linked.
-
Mindfulness meditation: We also teach mindfulness meditation that patients can continue to do at home. Studies show that mindfulness practices can combat stress and fatigue after a TIA, as well as help alleviate symptoms of depression.
-
Brain Wave: Finally, our patients also learn to use an app called Brain Wave. This app helps the brain produce calming alpha waves, which are the same ones the brain produces with meditation. We recommend the alpha setting, but you can experiment to see what works best for you.
Step 3: Recovery and Integration
.jpg?width=1557&height=1072&name=Dr.%20Alina%20Fong%20with%20a%20patient%20at%20Cognitive%20FX%20(V2).jpg)
At the end of treatment, patients undergo a follow-up scan to check on their progress. Then, they meet with one of our therapists to read their results and receive a series of exercises to do at home.
This homework typically includes physical exercises, cognitive activities, visual and vestibular exercises, and relaxation techniques. We recommend that patients do these exercises for about an hour five times a week at first, but this frequency can be gradually reduced as symptoms improve. For patients who need further therapy, we also recommend suitable specialists.
Schedule a consultation with our team to determine if our program is right for you.





.jpg?width=1557&height=1072&name=Dr.%20Alina%20Fong%20with%20a%20patient%20at%20Cognitive%20FX%20(V2).jpg)







