After a concussion or other type of traumatic brain injury (TBI), some patients experience persistent symptoms for months, or even years. This condition is known as post-concussion syndrome (PCS), and it can affect patients of any age.
PCS is not a well-known condition, so many patients live with it for years without knowing what’s wrong with them. It’s especially difficult to identify in young patients who can’t describe how they’re feeling. Even teens and adolescents may not realize why they’re struggling to concentrate at school or why they get headaches after using the phone.
Combine that with the fact that parents may not even be aware that their child has suffered a concussion — if it happened when they were practicing sports or out with friends, for example. It is entirely possible that these children could grow up experiencing symptoms without realizing the head injury was the culprit.
To address these difficulties, this article is intended to help both:
- Parents of children who suffered a concussion and are still experiencing symptoms more than six weeks after the injury.
- Adults who sustained a concussion when they were younger and have lingering symptoms but were never diagnosed with PCS.
Whether you’re a parent worried about your child or an adult wondering if an earlier concussion could explain all your symptoms, it’s important to seek evaluation and treatment from experts in post-concussion syndrome. At Cognitive FX, our world-renowned treatment program includes:
- Cutting-edge tools and methods for evaluation (especially functional Neurocognitive Imaging, or fNCI).
- The most multidisciplinary treatment team for PCS in the world.
- Evidence-based treatment practices that combine the benefits of cardio exercise with targeted therapies.
- Ongoing resources for recovery.
Whether the patient’s injury was a few months ago or a few decades ago does not impact treatment outcomes. We’ve seen many patients who came to us 20, 30, or 40 years after their head injury who made dramatic improvements during and after treatment.

Take Sam Gray, for example. He suffered a brain bleed when he was just 11 years of age. Thirty-three years later, he connected his symptoms with his childhood injury and found Cognitive FX. After treatment, Sam felt like he woke up from a dream. The world looked like a brighter place.
“People see the change in me. They ask, ‘What happened to you?’ and ‘Was it worth it?’”, said Sam. “And I tell them … it changes your life.”
Read how this businessman reclaimed his life back.
With that in mind, here’s what you need to know about the long-term effects of childhood injuries on the brain:
If you’re suffering from persistent symptoms after brain trauma, you’re not alone. Many of our patients struggle with headaches, word retrieval, feelings of overwhelm, and more before treatment. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-concussion symptoms. To see if you are eligible for treatment, schedule a consultation.
Head Injuries in Children Can Cause Long-Term Effects Into Adulthood
.jpg?width=1000&height=445&name=childhood%20head%20injuries%20(6).jpg)
Traumatic brain injuries (TBI) are one of the most common reasons for parents to visit the emergency room (ER) with their children. According to the Centers for Disease Control and Prevention (CDC), falls, motor vehicle accidents, and being struck during sports or recreational activities are the most common causes of head injuries in youngsters. Child abuse may also cause concussions and brain damage.
For most patients, symptoms dissipate in the days or weeks after their injury. However, in some cases, symptoms do not resolve, but instead become chronic. In addition, new symptoms may develop or come and go in waves. This condition is known as post-concussion syndrome (PCS).
Typically in children, PCS is defined as symptoms lasting longer than four weeks, and it affects around 13% to 30% of young TBI patients. Most adults are considered to have PCS if their symptoms last beyond three months. Worryingly, patients are unlikely to recover without the correct treatment, and children who develop PCS will continue to suffer the consequences into adulthood. PCS may develop after a mild, moderate, or severe brain injury.
Which Patients Are at Risk of Developing PCS?
At the moment, researchers and healthcare providers don’t understand why some patients develop PCS and others don’t.
In an attempt to make it easier for doctors to guide families of children who just suffered a concussion, a team of Canadian researchers assessed 46 potential risk factors and leading causes for PCS. They found nine symptoms or preconditions that could help predict the likelihood of developing long-term PCS if they are present during the first 28 days after the injury:
- Being female
- Being a teenager (age group between 13 and 18 years old)
- A history of migraines
- More than one concussion in medical history
- Headaches
- Sensitivity to noise
- Fatigue
- Answering questions slowly or feeling dazed after the concussion
- Balance issues
Studies with adult patients also suggest that a history of mental health problems — such as depression, anxiety, and personality disorders — or loss of consciousness after the injury may contribute to PCS, but this has not been confirmed in children. Research is ongoing to find better ways to predict which children will develop PCS so that medical professionals can offer appropriate treatment at much earlier stages.
One of our teenage patients, Sam Pembleton, ticked several of these boxes. A keen soccer player, she suffered two concussions in middle school (although the second was an accident when she was near a pickup game). She and her parents spent five years looking for treatment. During this time, Sam was rarely able to attend school or participate in extracurricular activities. Eventually, her mother found Cognitive FX.

“Leading up to Cognitive FX, I felt the lowest I've ever been in my life and hopefully will ever be. I was so isolated, and I felt so hopeless, and I found it extremely hard to get out of that, just because there wasn't much I could do, and normal therapies weren't working for me,” said Sam. “But after Cognitive, it's been like night and day. It's so much better. I feel like a normal teenager. I have friends that I hang out with. I actually leave the house now.”
Read more about Sam’s story and how she overcame her concussion symptoms.
PCS Symptoms in Children vs. Adults
.png?width=643&height=882&name=childhood%20head%20injuries%20(14).png)
Overall, children and adults can experience the same range of cognitive, physical, and emotional problems after a head trauma. But the way children present can differ, so the checklist of questions we share helps parents identify them more easily. Common PCS symptoms in children and adults include:
Cognitive Symptoms
Physical Symptoms
Emotional and behavioral Symptoms
If you’re a parent of a child who is still struggling after a mild traumatic brain injury (mild TBI), it can be difficult to recognize these symptoms. Children may not be able to explain how they feel or even notice that there is something different. Sometimes symptoms can be confusing, and children may simply act frustrated and angry. It helps to understand how these symptoms look from the outside. As a general rule, any changes from normal behavior may indicate PCS, including:
- Do they no longer like school when they used to love it (or reading, parties, shopping, etc.)?
- Do they complain of headaches during or after cognitive or physical activity or insist they don’t want to do them anymore?
- Are they having frequent emotional outbursts (out of the blue) that they never used to have, and you can’t figure out why?
- Are they exhibiting symptoms of attention deficit hyperactive disorder (extra fidgeting, poor impulse control, short attention span, etc.)?
- Are they struggling to learn and retain information? Do they have difficulty reading?
- Do they suddenly get grumpy whenever they play video games?
- Are they getting dizzy and nauseous in cars?
- Does their balance or coordination seem off?
- Do they complain of blurry vision or changes to their vision?
- Do they now prefer quiet places and seem more withdrawn?
- Do they have sleep problems like trouble falling asleep and/or trouble staying asleep?
If you answered “yes” to one or more of these questions, your child could be suffering from post-concussion syndrome. In that case, it’s important that you seek medical help to get a diagnosis and treatment. Many of these issues can be treated, but your doctor needs to understand that they’re caused by the head injury to treat them effectively. Later in the article, we explain in detail how we diagnose and treat PCS patients at our clinic.
Further reading: Post-Concussion Syndrome in Children
What Causes PCS Symptoms?
.png?width=1600&height=1472&name=childhood%20head%20injuries%20(15).png) Post-concussion syndrome can be caused by a variety of factors. Usually, it’s a combination of one or more of the following:
Post-concussion syndrome can be caused by a variety of factors. Usually, it’s a combination of one or more of the following:
Neurovascular Coupling (NVC) Dysfunction
Many PCS symptoms are caused by dysfunctional neurovascular coupling.
In a healthy brain, brain cells receive oxygen and nutrients from a network of blood vessels in the brain. This mechanism is called neurovascular coupling (NVC).
Brain injuries, however, can disrupt this connection such that brain cells in affected areas stop getting what they need, when they need it. While they have enough nutrients to survive, they don’t function at the level they did previously. When patients try to perform tasks controlled by these areas — such as following a conversation or playing a video game — they often struggle. The brain may attempt an alternative neural pathway to complete the task, but it’s always less efficient and more tiring for the patient. That can lead to headaches, feeling overwhelmed, and irritability.
Patients may also experience symptoms specific to the areas of the brain that were affected by the concussion. Some examples are struggling to find the right word if the TBI affected parts of the brain involved in speech or altered peripheral vision if it affected areas involved with eyesight.
Dysfunction of the Autonomic Nervous System (ANS)
A second cause of PCS symptoms involves the autonomic nervous system (ANS).
The ANS controls many behind-the-scenes bodily functions such as heart rate, blood pressure, and breathing rate. This is done by two subsections of the ANS, called the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS activates the “fight or flight” response when you're stressed and worried about something. In contrast, the PNS is responsible for the “rest and digest” mechanisms involved in calming the body.
Under normal circumstances, both work together in harmony, and which side ‘dominates’ fluctuates between the SNS and the PNS, as needed. In PCS patients, however, the SNS remains active most of the time, even if there is no source of stress. Being constantly on “standby” leads to fatigue, headaches, high blood pressure, digestive issues, problems sleeping, mood changes, and other symptoms.
Further reading: Autonomic Nervous System Dysfunction after a TBI
Vision Problems
Vision problems are common in children after a mild head injury. TBIs can affect how the eyes communicate with the brain or disrupt function in the areas of the brain involved with vision. Patients may experience a variety of visual issues, such as changes in peripheral vision, eye teaming (how the eyes work together), depth perception, and focusing. As a result, patients often complain about headaches, tired eyes, double vision, and difficulty reading, among others.
Further reading: Vision Problems after Concussion
.jpg?width=1000&height=445&name=childhood%20head%20injuries%20(4).jpg)
Vestibular Dysfunction
Similar to vision, children can experience long-term vestibular problems after a concussion. Your body, eyes, and vestibular system (located in the inner ear) work together to send information to the brain about the position of your body. TBIs can disrupt this connection or affect the areas in the brain that process this information. As a consequence, patients may experience dizziness, nausea, or problems with balance.
Further reading: Vestibular Therapy for PCS
Hormonal Dysfunction
If the pituitary gland and the hypothalamus — located at a particularly vulnerable place in the brain — are damaged during a TBI, it can trigger a variety of symptoms. That’s because these two structures regulate multiple hormones, which are involved in many different mechanisms throughout the body. For example, young girls can experience abnormal menstrual periods for months after a concussion due to hormonal issues.
Other symptoms may include emotional changes, fatigue, dizziness, vision problems, weight changes, cold or heat intolerance, and more.
Further reading:
Breathing Dysregulation
Finally, damage to areas of the brain involved in regulating breathing will lead to respiratory problems, such as shallow or irregular breathing and/or shortness of breath. For example, some patients can take deep breaths but cannot completely exhale because the brain can no longer detect how much the lungs are expanding or contracting. This generates excessive amounts of CO2 in the blood, which leads to headaches or even seizures (in extreme cases).
Further reading: Can PCS cause breathing difficulties?
Getting an Accurate PCS Diagnosis Is Challenging
.jpg?width=1000&height=445&name=childhood%20head%20injuries%20(2).jpg)
For PCS patients, the first step toward recovery is to get an accurate diagnosis.
If you’re a parent, and your young child is suffering long-term symptoms, you may decide to visit a sports medicine doctor (if it was a sports injury) or a pediatrician. However, chances are, you will not get a PCS diagnosis. Many pediatric or even neurology specialists don’t recognize the multiple symptoms as one condition and instead treat specific symptoms, such as dizziness or headaches. Or, they may misdiagnose your child with a learning disability, such as attention-deficit hyperactivity disorder (ADHD) or other behavioral problems, and refer them to a neuropsychology or psychiatry specialist.
Misdiagnosis delays the long-term recovery your child needs, placing them at risk of developing long-term cognitive issues. That may cause problems at school, including poor academic achievements and poor school attendance.
If you’re an adult who suffered a concussion as a child, you may be wondering if your current symptoms may still come from the head injury you experienced when you were younger.
If you’re wondering how this went unnoticed for so long, it’s actually easy for parents to miss head injuries in their children. If they happen at school or during sports, parents may not necessarily be informed at the time. If your symptoms were mild, they were probably attributed to other conditions or simply to the fact that you were growing up.
A study found that 1 in 4 children is misdiagnosed and continues to suffer from PCS symptoms for many years as a young adult. Long-term outcomes such as memory problems, sensitivity to light and noise, and psychological problems are often mistakenly diagnosed as ADHD, sleep disorders, or depression.
Without adequate treatment, these patients are more likely to develop medical and social problems later in life. A study followed over 100,000 TBI patients who suffered a concussion at a young age throughout their lives and found that they were more likely to experience mental health problems as adults and struggle at work.
One of our patients, Olivia Seitz, knows this from personal experience, after suffering multiple head injuries at a young age while figure skating. Olivia had to quit both her beloved sport and her teaching career because of her PCS symptoms.

Finally, after 14 years of unexplained chronic illnesses, Olivia found Cognitive FX. “Once I went through testing and treatment, there was no question that post-concussion syndrome was the mystery illness I’d been fighting,” said Olivia. “I am doing so much better. My energy levels are higher, and my symptoms are less oppressive. It’s awesome.”
Read more about Olivia’s journey to recovery here.
Evaluation and Treatment of Post-Concussion Syndrome
.png?width=552&height=227&name=childhood%20head%20injuries%20(8).png)
Before treatment, each patient needs to complete a detailed medical examination. During this exam, our team will ask about your or your child's symptoms, review your medical history, and test physical, cognitive, and emotional health. We can treat children aged eight and up (or at a third-grade reading level).
Patients also undergo a functional Neurocognitive Imaging (fNCI) scan. This scan looks at how blood flows in 56 regions of the brain and how these regions communicate with each other while the patient performs a series of cognitive activities. In practical terms, the scan allows our therapists to identify how much and where in the brain a concussion has affected neurovascular coupling (NVC).
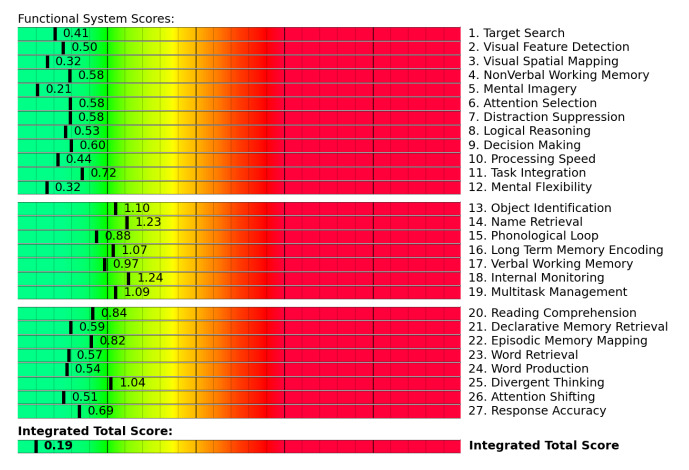 fNCI results from a patient with healthy neurovascular coupling. Scores in the yellow and red zone often indicate poor NVC.
fNCI results from a patient with healthy neurovascular coupling. Scores in the yellow and red zone often indicate poor NVC.
After this initial evaluation process, our therapists use the results to design a customized treatment for you or your child. Treatment involves a three-step cycle that repeats multiple times a day: Prepare, Activate, and Recover. The main goal is to restore normal neurovascular coupling in the brain, as well as to improve ANS function and reduce the incidence and severity of PCS symptoms.
The first step involves preparing the brain for the intense therapy that’s coming next. Patients engage in short sessions of aerobic exercise (typically on a treadmill or stationary bike) to take advantage of a phenomenon in the brain called the post-exercise cognitive boost (PECB). PECB triggers the release of neurochemicals that promote healthier blood flow in the brain. One of these chemicals is called brain-derived neurotrophic factor (BDNF). It helps the brain perform complex cognitive challenges for longer periods. In practical terms, a session of aerobic exercise before therapy boosts the impact of subsequent therapies and helps treat the root cause of PCS symptoms.

The second step involves multidisciplinary therapies to activate and challenge your or your child’s memory, motor skills, executive thinking, and more. A few of the therapies we employ during treatment include:

Finally, we also provide set times throughout the day for patients to recover and relax before going to the next therapy session. This often includes neuromuscular massage of the neck and shoulders, learning breathing exercises to relax, mindfulness exercises, and listening to Brainwaves (which work similarly to meditation).
At the end of treatment, patients undergo a second brain scan to see how much their brains have improved. Patients also meet with a member of our team to discuss progress and receive a list of follow-up exercises to do at home. This takes about an hour to do and includes aerobic exercises, cognitive games, and rest.
Our recommendation is to start with about an hour for five days a week and then slowly reduce at-home exercise as recovery progresses. We believe this is the best way to ensure that patients continue to recover at home in the weeks and months after their treatment.
Treatment for children
Essentially, treatment is the same for children and adults, with a few extra considerations:
- Our activities in therapy can be tailored to children and include content they are likely to find interesting. For example, if they like soccer, then our therapists might use a soccer ball instead of a football. Or if they’re interested in dinosaurs, they will weave dinosaurs into word games and other cognitive activities.
- Parents are welcome to attend the sessions, but not all children want them to. Some children need some space and perform better if the parents are not in the room, while others find it reassuring to see familiar faces present.
- We know how important it is to communicate with parents. We love to partner with parents to understand what motivates their child, their likes and dislikes, and what they fear.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in therapy for persistent brain injury symptoms. To see if you are eligible for treatment, sign up for a consultation.
Frequently Asked Questions
.jpg?width=1000&height=445&name=childhood%20head%20injuries%20(7).jpg)
Are My Symptoms Permanent?
We find that most of our patients experience complete recovery for some, but not all, symptoms. Some symptoms may improve a lot, but they’re still present, while others only improve a little or not at all. Each patient is different.
What we can say for sure is that, without treatment, your symptoms are much more likely to become permanent, with long-term consequences. Reports show that symptoms may change with time, but PCS patients don’t usually recover by themselves.
How Can I Help My Child at Home?
There are many ways to help your child at home:
- Be patient with them, and always offer support and encouragement. Recovery from PCS is a long journey, and your child will have good days and bad days.
- Learn to recognize their triggers, and plan around them, if possible. For example, avoid long car journeys or busy shopping areas if that makes them feel sick or overwhelmed.
- Monitor their screen time, including school work and recreational use. Make sure they have regular breaks away from the screen.
- Help them pace themselves throughout the day.
- Play cognitive games when their symptoms allow. (Here are 17 cognitive exercises they can play.)
Will I/My Child Struggle at School Because of PCS? How Can the School or College Help?
PCS can cause many cognitive issues, including difficulties with concentration, poor memory, and brain fog. In addition, patients may also suffer from emotional problems and alterations in vision and balance. Not surprisingly, this may affect how children perform at school and reduce their educational attainment.
The CDC recommendation is to return to school as soon as possible after a concussion to avoid missing too much. This may involve some modifications at school, college, or university to ensure the patient doesn't struggle with symptoms. The best way is to devise a customized plan for each patient, taking into account the severity, type, and duration of symptoms. This may include:
- Reduced timetable
- Extra resources to catch up
- One-to-one help in class
- Extra time to complete assignments and exams
- Frequent breaks
Effective communication between the student, parents, and teachers is key. If possible, involving a school psychologist or social worker can be beneficial in assessing how the patient is coping and adjusting the plan further, if needed.
Can PCS Prevent Me/My Child From Playing Sports in the Future?.jpg?width=1000&height=443&name=childhood%20head%20injuries%20(1).jpg)
In general, playing sports should only be considered after a patient has returned to normal academic participation without any modifications in place (see previous question). Even in this situation, the decision to return to sports should be done in conjunction with your doctor.
Returning to organized sports after a TBI should follow a strict Return To Play (RTP) process. This involves gradually adding more intense forms of exercise, starting with simple exercises on a stationary bike all the way to harder training drills and full contact.
If exercise triggers severe symptoms at any stage, patients stop and go back to the previous stage. This applies to patients who just suffered a concussion, as well as to those who are experiencing long-term symptoms. It’s worth noting that when symptoms are triggered either by cognitive or physical exertion, it does not cause any further brain damage. Guidelines concerning symptoms are to help the patient experience a smoother recovery, but they need not be anxious about further injury from over-exercising.
Without treatment, it is unlikely that PCS patients will be able to return to sports, especially if they want to return to a competitive level.
Further reading: Exercise after a Concussion
Do I/Does My Child Need to See a Psychologist?
It’s common for PCS patients to experience emotional and behavioral issues, such as depression, anxiety, and irritability. This may develop soon after the concussion or years later into adulthood.
During treatment, all of our patients meet with a psychologist for a mental health evaluation. If we find that they need additional care, we’ll recommend counseling or other forms of psychotherapy. For example, both young patients and adults may benefit from cognitive behavioral therapy (CBT) to help reduce stress, anxiety, and depression, as well as to improve sleep and cognitive function.
Further reading: Cognitive Behavioral Therapy for PCS
Can PCS Be Treated With Medication?
With very few exceptions, our patients say that any meds they tried before coming to us didn’t really help or caused worse side effects.
The problem is that most doctors are not trained, nor do they have the resources to diagnose and treat PCS symptoms. Often, the only treatment they can provide involves prescription drugs to address individual symptoms.
As a parent, you need to scrutinize any medication prescribed to your child very carefully. Many of the children who come to us have been incorrectly diagnosed with ADHD and given medication to help them with school. Sometimes, these patients also receive meds to help them sleep at night. This is not a healthy combination. Using ADHD and sleep meds at the same time is dangerous, can make their symptoms worse, and will likely inhibit their recovery.
Also, children with PCS can be prescribed antidepressants and other medication for anxiety or depression. Some children may truly need them for their mental health, but these drugs cause changes in the brain and may delay recovery from PCS.
In addition, over-the-counter medications can have an impact, too. For example, excessive or prolonged use of painkillers such as acetaminophen (Tylenol) or NSAIDs (Ibuprofen, Aleve) can trigger rebound headaches.
Medications can be useful in certain situations after a pediatric traumatic brain injury, but it’s better if you or your child receives the right treatment to address the real problems causing PCS symptoms, therefore eliminating the need for medications altogether.
How Can I Help Myself or My Child Sleep Better?
Sleep problems are common in children with PCS. This may include sleeping too much or not enough, sleep apnea, and restless leg syndrome.
At Cognitive FX, we don’t think medication is the answer to treat PCS symptoms, but there is one exception that you may want to try: melatonin. Studies show that taking melatonin can not only help patients with PCS sleep better, but it may also improve symptoms of depression and anxiety.
In addition, there are many ways you can help yourself or your child sleep better:
- Follow a regular sleep routine by going to bed and waking up at the same time every day, even during weekends and holidays.
- Find a relaxing activity to do before bed, such as reading a book in a quiet place or listening to calming music.
- Limit daytime naps to 20-30 minutes, ideally before 3 p.m. If you or they sleep too much during the day, they may struggle to sleep at night.
- Use earplugs at night if noise sensitivity is an issue.
- Keep the bedroom comfortable, cool, and dark enough to fall asleep.
- Avoid caffeinated drinks in the evening.
- Don’t use mobile phones before bed.
Further reading: Post-Concussion Syndrome and Sleep
Can I/My Child Develop ADHD From PCS?
Many symptoms of PCS and ADHD are similar, including memory problems, lack of attention, deficits in executive skills, mood swings, and impulsivity. It can be difficult to determine whether you or your child are suffering from PCS, ADHD, or even both.
The worrying part for parents is that recent studies show that 1 in 5 children who had a head injury may develop ADHD. This is known as secondary ADHD because it’s caused by an injury, and symptoms may take up to a decade to develop.
This makes it even more important to receive treatment — such as what we offer at Cognitive FX — as soon as possible. The aim is to eliminate PCS symptoms and lower the risk of developing ADHD.
Further reading: Link Between Concussions and Attention Deficit Disorder
Can Patients With Severe TBI Expect Good Results From Treatment?
PCS patients consistently see strong results from treatment at our clinic. But what if you suffered a skull fracture? Or had neurosurgery? Or just finished inpatient rehabilitation at the hospital to relearn skills like brushing your teeth and tying your shoelaces?
Patients who suffered a severe head injury can and do make significant progress during treatment, but how much we can help you specifically depends on your injury. We have a number of resources for severe TBI patients. If you would like to learn more, read the following:
- Abigail Ward’s recovery story. Abigail fell off a 70 foot cliff and was in a coma for months. After she completed the outpatient rehabilitation program available through the hospital, she came to Cognitive FX to further her recovery.
- How much can you recover from a TBI? This post delves more deeply into the question of when and how much you can recover from a TBI.
- The long-term effects of TBI. This post discusses the long-term implications of TBI, how it’s treated, and what Cognitive FX can specifically offer TBI patients.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in therapy for persistent brain injury symptoms. To see if you are eligible for treatment, sign up for a consultation.


.jpg?width=1000&height=445&name=childhood%20head%20injuries%20(6).jpg)

.png?width=643&height=882&name=childhood%20head%20injuries%20(14).png)
.png?width=1600&height=1472&name=childhood%20head%20injuries%20(15).png) Post-concussion syndrome can be caused by a variety of factors. Usually, it’s a combination of one or more of the following:
Post-concussion syndrome can be caused by a variety of factors. Usually, it’s a combination of one or more of the following:.jpg?width=1000&height=445&name=childhood%20head%20injuries%20(4).jpg)
.jpg?width=1000&height=445&name=childhood%20head%20injuries%20(2).jpg)

.png?width=552&height=227&name=childhood%20head%20injuries%20(8).png)
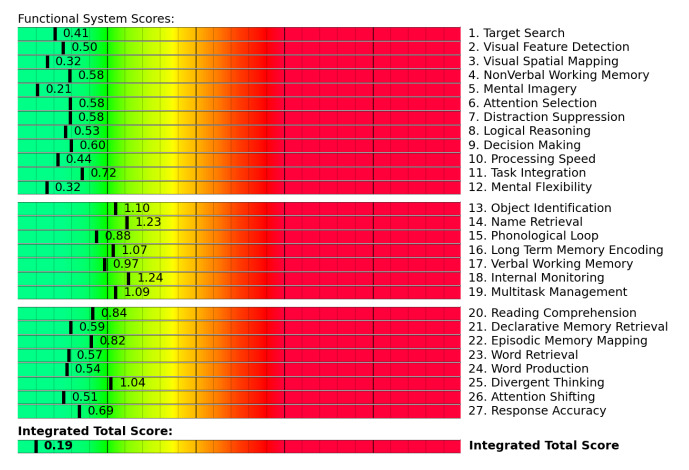 fNCI results from a patient with healthy neurovascular coupling. Scores in the yellow and red zone often indicate poor NVC.
fNCI results from a patient with healthy neurovascular coupling. Scores in the yellow and red zone often indicate poor NVC.

.jpg?width=1000&height=445&name=childhood%20head%20injuries%20(7).jpg)
.jpg?width=1000&height=443&name=childhood%20head%20injuries%20(1).jpg)









