Most patients recover from a concussion within days or weeks. But for roughly 30%, symptoms such as post-traumatic headaches, dizziness, fatigue, sleep disturbance, and brain fog persist for months or even years—highlighting the prevalence of a condition known as post-concussion syndrome (PCS), and the need for better long-term treatment solutions.
At Cognitive FX, we specialize in helping these patients recover through a multidisciplinary, individualized approach grounded in cutting-edge brain imaging and neuroscience.
Our treatment is centered around a form of functional MRI called functional NeuroCognitive Imaging (fNCI), which can identify specific brain regions that have been affected by a mild traumatic brain injury (mTBI). This insight allows us to develop highly targeted treatment programs involving physical, cognitive, and psychological therapies.
Internal data shows that over 90% of our patients experience significant symptom improvement after treatment. Now, our program’s effectiveness has been independently validated. A peer-reviewed study published by researchers in the Netherlands found that ~77% of participants who received our treatment experienced substantial symptom relief.
In this article, we explore:
- The challenges PCS patients face in getting adequate care
- How Cognitive FX addresses these challenges
- Key findings from the recent study on our treatment’s effectiveness
The Ongoing Challenges PCS Patients Face
1. Lack of Expertise in the Healthcare System
Many PCS patients go months or even years without a proper diagnosis. Primary care providers and even some neurologists lack the training to recognize PCS or provide effective care.
Instead of addressing the root cause, they often prescribe symptom-based medications (e.g., painkillers, sleep aids, antidepressants), which may bring temporary relief but do not facilitate long-term recovery.
How We Address This at Cognitive FX
Our team comprises highly trained specialists with deep experience in treating persistent post-concussion symptoms, as well as lingering symptoms from other types of head injuries and mild TBIs (e.g. transient ischemic attacks, carbon monoxide poisoning, whiplash, encephalitis, and others).
Therapists from different disciplines are trained to recognize the neurological, emotional, and physical complexities of PCS. Our personalized care model ensures patients feel seen, understood, and properly guided in their recovery.
You can hear from past patients such as:
- Olivia Seitz, a former figure skater who suffered sport-related concussions
- Anthony Loubet, a lawyer sidelined after a car accident
- Sam Pembleton, a student who visited multiple clinics before finding Cognitive FX
2. Lack of Coordinated, Multidisciplinary Care
PCS symptoms span multiple systems: neurological, cognitive, visual, vestibular, and emotional.
Effective treatment requires a coordinated effort from experts across disciplines. Unfortunately, most patients are left to navigate siloed providers on their own, with little communication between specialists.
How We Address This at Cognitive FX

Cognitive FX delivers fully integrated, multidisciplinary care under one roof. Our team includes specialists in:
We develop a custom treatment plan for each patient based on comprehensive diagnostic results, and our providers communicate daily to fine-tune care. This integration not only saves time and reduces stress, but also leads to better outcomes.
Our exercises often combine multiple therapy goals. For example, a patient may balance on a Bosu ball (vestibular training) while catching color-coded balls (motor coordination) and performing mental math (cognitive engagement). These multi-layered therapies drive neuroplasticity and recovery.
3. Lack of Specialized Tools for PCS Diagnosis
Most doctors do not have advanced equipment at their disposal, so they rely on the patient’s self-reported description of symptoms, in-person examination, and/or neuropsychological testing to assess cognitive impairment and make their diagnosis. (If the patient is an athlete with an established baseline, they may also use baseline testing.)
These methods have limited effectiveness because they don’t show clinicians the exact areas of post-injury brain dysfunction (which are different for each patient), and therefore don’t provide clear insight for targeting treatment.
Traditional imaging—such as computerized tomography (CT scan) or structural magnetic resonance imaging (standard MRI)—typically shows nothing abnormal in patients with persistent post-concussive syndrome. That’s because PCS is caused by functional, not structural, changes in the brain. When scans come back “normal,” patients are often dismissed or told their symptoms are psychosomatic.
How We Address This at Cognitive FX
Instead of strictly conducting interviews with the patient about their symptoms, as you’d experience at most concussion clinics, we use advanced neuroimaging to pinpoint exactly where the brain is showing signs of dysfunction.
The type of scan is called Functional Neurocognitive Imaging (fNCI), which measures two key things:
-
Regional brain activity: How much oxygen each brain region uses during specific cognitive tasks (indicating underactive, normal, or overactive function).
-
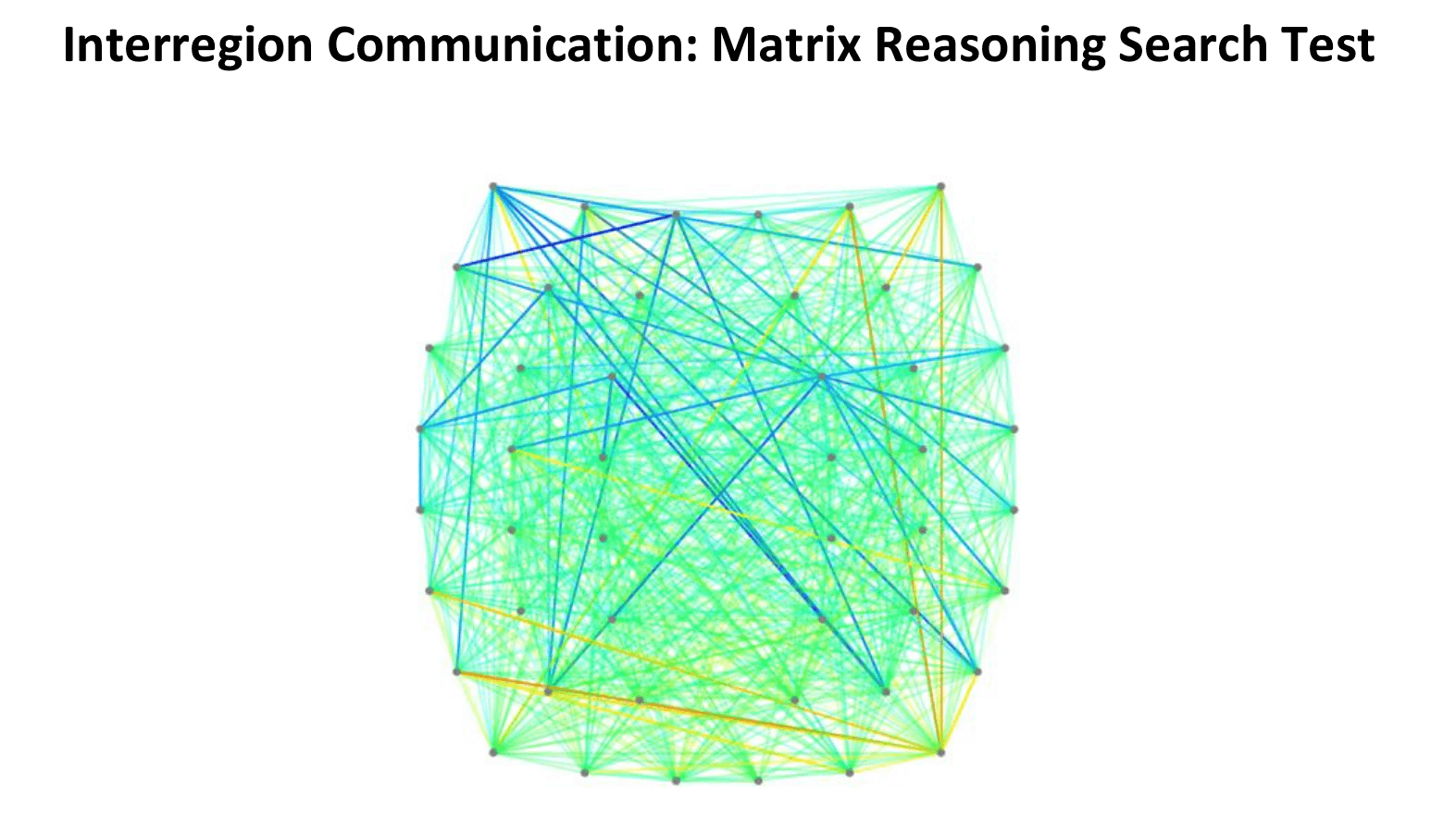
Connectivity between regions: How well different parts of the brain communicate with each other.
The scan results are displayed in intuitive charts and brain maps that help us identify whether a patient is experiencing hypoactivity (under-functioning), hyperactivity (over-functioning), or a mix of both—and where.
This detailed view of brain function allows us to tailor each person’s therapy precisely.
For example:
-
Someone with hypoactivity may need therapies that target various brain regions with stimulation and cognitive endurance training.
-
Someone with hyperactivity may benefit from therapies that reduce neural “noise” and promote regulation.
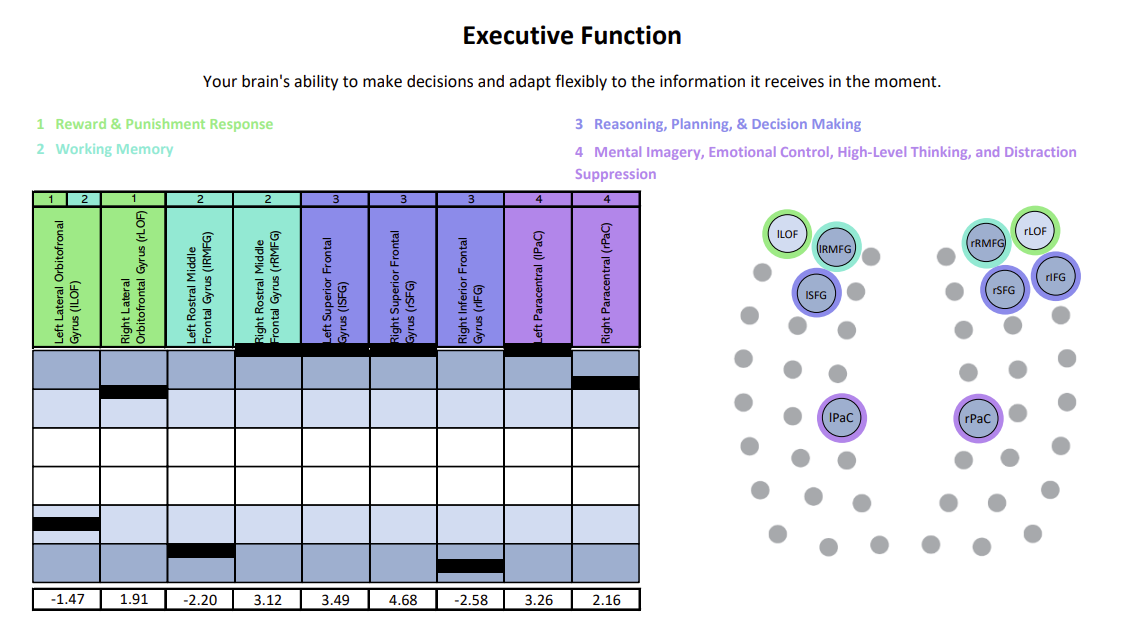
We’ve organized scan results for regional activity into six clear cognitive domains—like memory, attention, and executive function—to make them easier to understand and better guide individualized treatment.
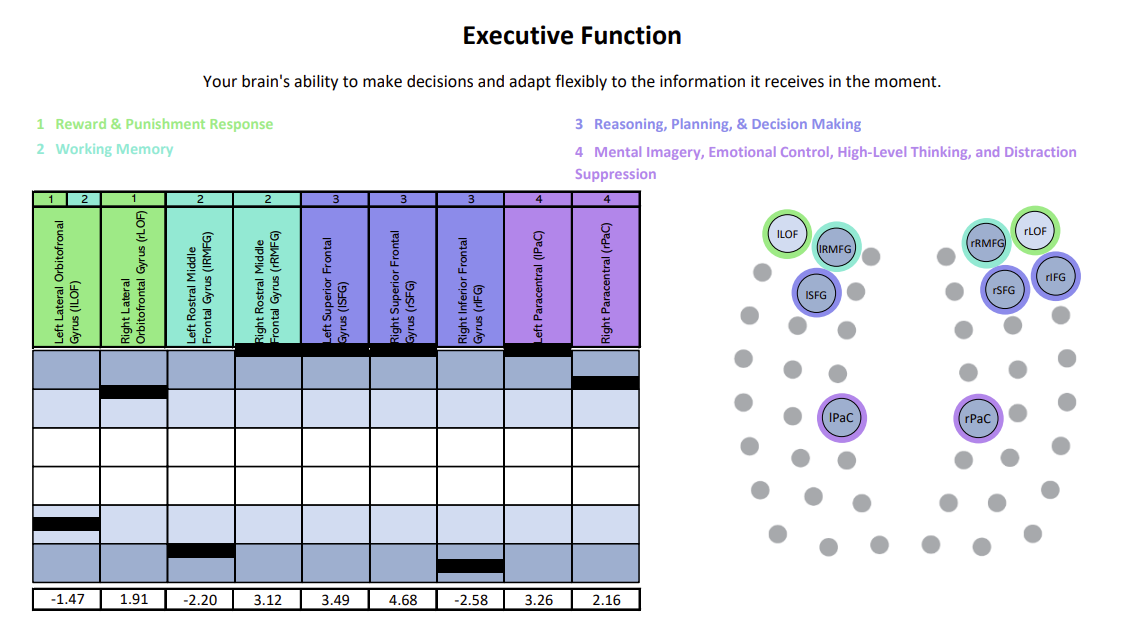
Each chart shows how specific brain regions are functioning compared to a normal brain. The white area represents the normal range, with the center line marking the average. Light and dark blue zones show increasing levels of abnormality. A black line marks the patient’s result for that region—ideally landing within the white. Lines in the light and dark blue zones suggest that region is either hyperactive (blue zones above the white) or hypoactive (blue zones beneath the white). In this example, the patient was experiencing both hypoactivity and hyperactivity within different key regions linked to executive function.
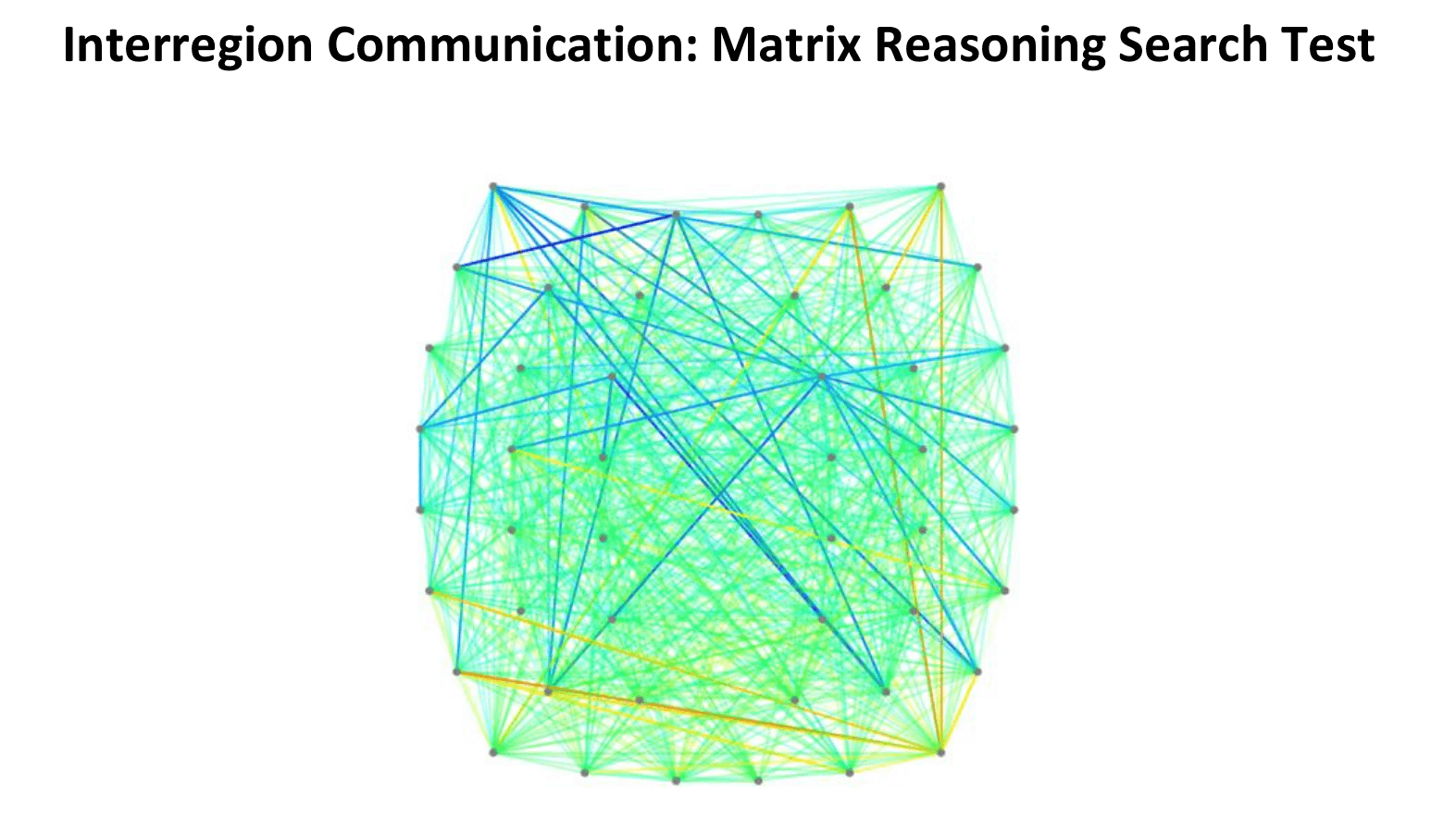
In this connectivity map, cooler colors (blues) indicate areas of hypoactivation (underactivity), while warmer colors (reds, oranges, yellows) indicate areas of hyperactivation (overactivity).
This detailed insight allows us to design highly targeted interventions. While fNCI is not widely used for concussion diagnosis, research shows it can outperform cognitive tests in identifying functional abnormalities related to mild head injuries.
4. Lack of Evidence-Based PCS Treatments
Despite ongoing research, there is no universal treatment for PCS. Every patient presents differently—one may struggle with vision and attention, another may struggle with mental health and balance problems. One-size-fits-all therapies often fall short, and few treatment centers have published long-term outcomes.
How We Address This at Cognitive FX

Our specialized neurorehabilitation program—Enhanced Performance in Cognition (EPIC)—is built around individualized recovery. Each patient’s plan is informed by their fNCI scan, physical and psychological assessments, and unique profile of cognitive symptoms, physical symptoms, and emotional symptoms.
The treatment cycle consists of:
- Prepare: Aerobic exercise to increase brain plasticity and blood flow.
- Activate: Targeted cognitive, physical, and emotional therapies.
- Recover: Rest periods with breathing, mindfulness, and neuromuscular massage.
Patients leave with a second fNCI scan showing their progress, plus a home exercise plan to continue recovery. Over our years of clinical practice, we’ve refined our protocol using data from thousands of patients.
New Independent Study Supports the Effectiveness of Our Treatment
For years, we’ve collected internal data supporting the effectiveness of our program. Now, a third-party study by researchers from the Netherlands provides independent validation.
Study Overview
-
Sample: 69 patients treated at Cognitive FX. All were adults with persistent symptoms after concussion and shared common demographics (age, majority female) and time since injury (years on average).
-
Timeline: Patients completed questionnaires before treatment, one week after treatment, one month after treatment, and six months post-treatment.
-
Measures: The study evaluated symptom severity using validated clinical scales, including:
- Depression, Anxiety, and Stress Scale (DASS)
- Fatigue Severity Scale (FSS)
- Sleep and vision assessments
- Quality of life indicators
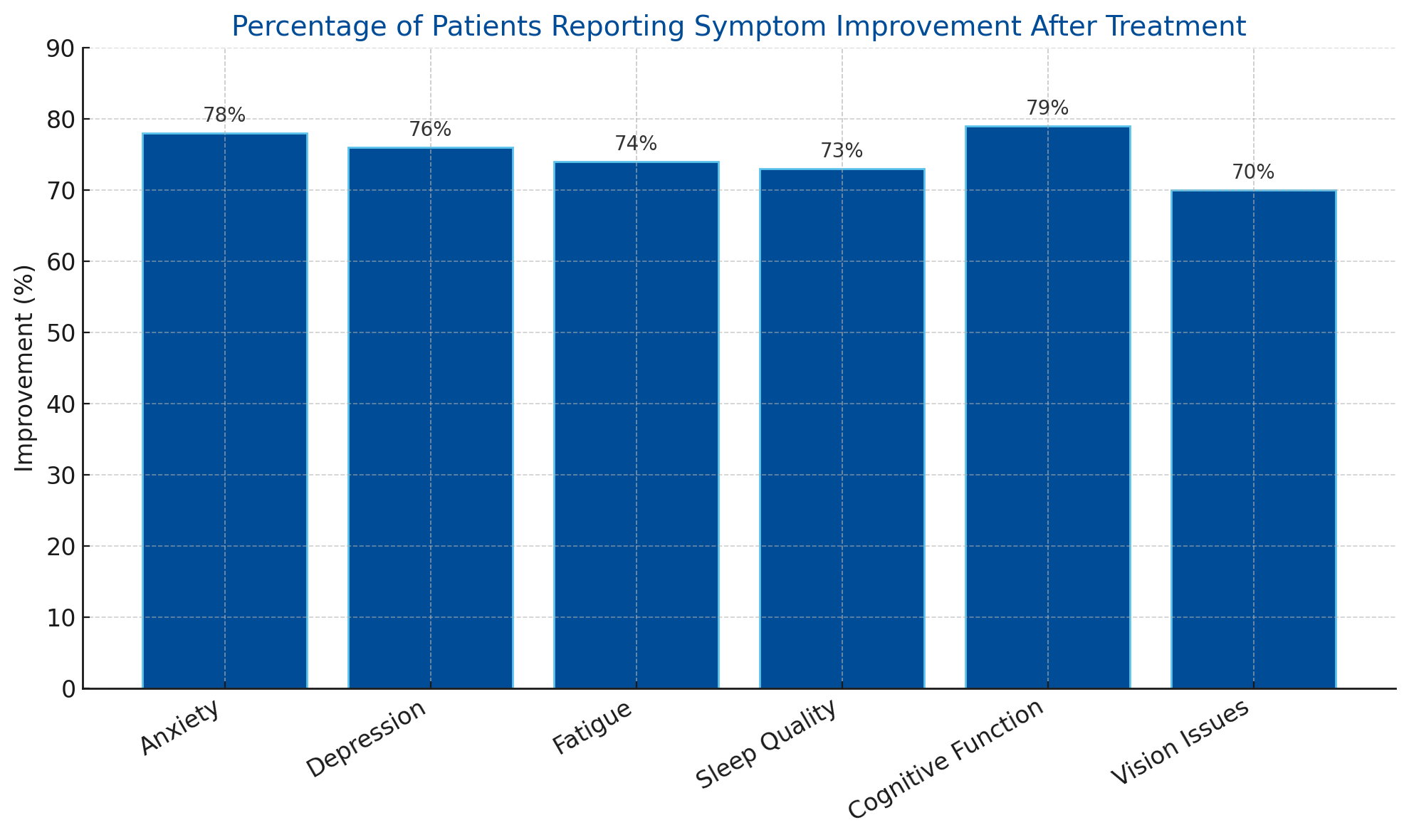
Key Results
-
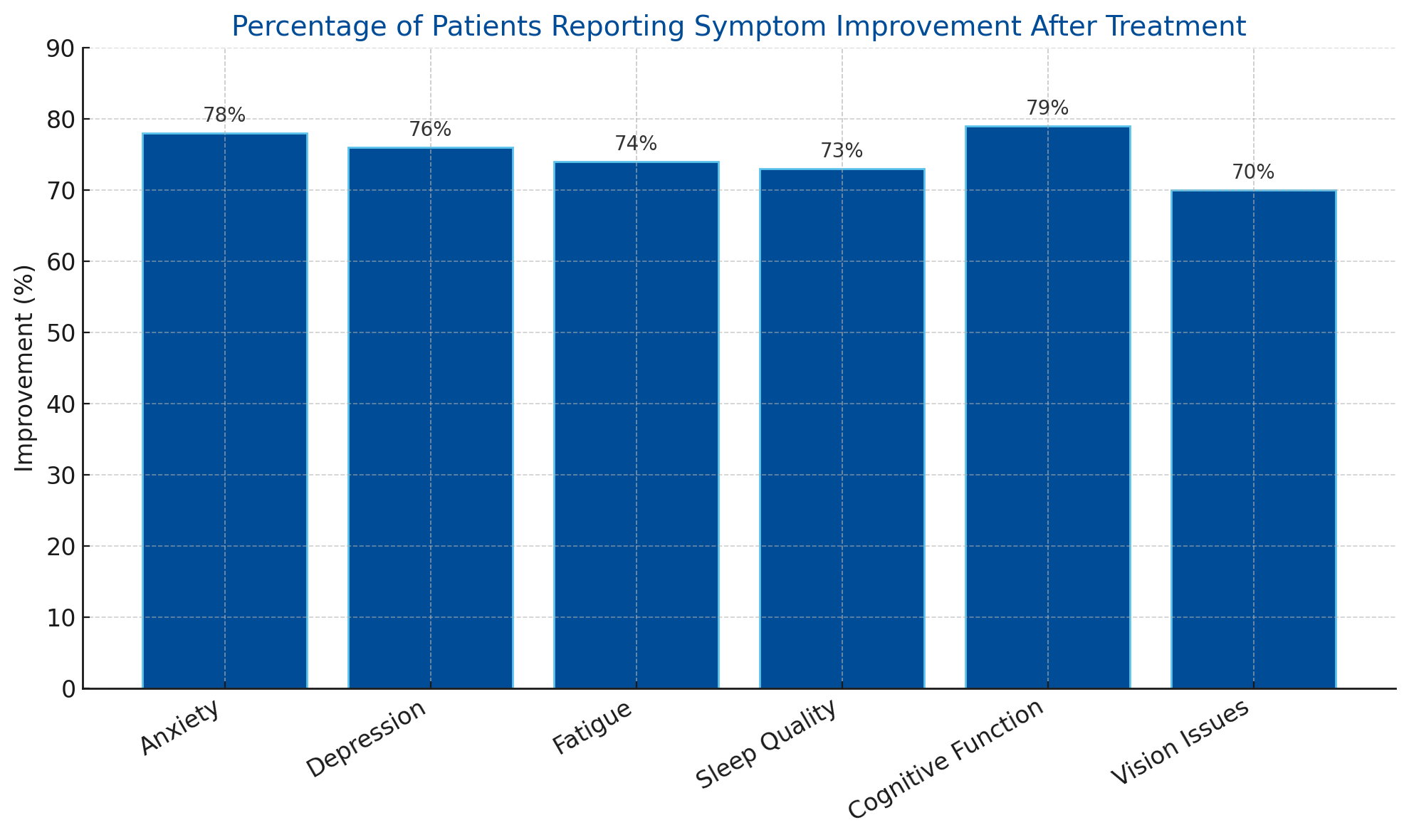
77% of patients experienced a clinically significant reduction in symptoms after treatment.
-
Statistical analysis showed improvements across all categories:
- Reduced anxiety, depression, and fatigue
- Better sleep, cognitive performance, and vision
- Enhanced quality of life
-
Patients with more severe psychological symptoms before treatment showed the most improvement, both physically and emotionally.
-
Gains were highest at the six-month follow-up, suggesting long-term effectiveness.
-
Not all participants improved, and a minority worsened on some outcomes.
|
Symptom Category
|
% of Patients Reporting
Improvement
|
|
Anxiety
|
78%
|
|
Depression
|
76%
|
|
Fatigue
|
74%
|
|
Sleep Quality
|
73%
|
|
Cognitive Function
|
79%
|
|
Vision Issues
|
70%
|
This is the first peer-reviewed validation of a specialized PCS clinic’s outcomes, placing Cognitive FX at the forefront of evidence-based concussion recovery.
Disclaimers and Considerations
-
On not having a control group: Yes, it was not a randomized controlled trial. But all factors considered, it’s extremely likely the symptom reductions were largely due to Cognitive FX treatment.
-
Generalizability considerations: The cohort study consisted only of adults (mostly female). Whether results would generalize to other patient demographics, such as pediatric/adolescent populations, requires further study.
-
More research is needed: Randomized controlled studies and systematic reviews are needed to further our understanding of treatment efficacy.
What This Research Means for Patients and Providers
This study reinforces what many in the field have suspected: post-concussion syndrome is a complex, multi-system condition that requires a comprehensive, individualized approach to treatment. While it may not offer a definitive cure, the data show that targeted, multidisciplinary care—like the approach we use at Cognitive FX—can lead to meaningful, lasting improvements for many patients.
For Patients
Recovery from PCS can be frustratingly non-linear, but improvement is possible—even months or years after injury. This study is a reminder that:
-
A treatment program that addresses multiple systems (e.g., cognitive, visual, vestibular, and emotional) may be more effective than single-symptom interventions.
-
Advocating for advanced neuroimaging, such as fNCI scans, can significantly improve diagnosis accuracy and guide targeted treatment.
-
Advocating for coordination between your healthcare providers may help lead to better treatment outcomes.
-
Progress takes time. It’s common for symptoms to fluctuate before settling.
-
Setting clear goals and communicating openly with your care team is key to navigating the uncertainty of recovery.
For Clinicians
The findings support a shift toward multi-domain rehabilitation—combining aerobic activity, cognitive challenges, vestibular and oculomotor retraining, and psychological support. In particular:
-
Advanced neuroimaging should be considered more often, as it allows for more targeted and effective treatment.
-
Monitor mood, sleep, and fatigue closely, as these comorbidities often influence symptom severity and response to treatment.
-
While this was not a randomized controlled trial, the real-world improvements offer encouraging signals.
-
Continued research into predictors of treatment response may help refine patient selection and protocol design over time.
In short, the study supports that targeted, multidisciplinary care can make a real difference—and that hope and healing are possible, even when recovery feels out of reach.
Interested in Getting Help for PCS?
If you or a loved one is struggling with lingering concussion symptoms, we’re here to help. Our evidence-based, individualized approach has helped thousands of patients regain their quality of life—and now, this research confirms what we see every day.
Want to learn more? Contact us to schedule an evaluation or speak with a team member.