Headaches are one of the most common symptoms after a head injury (studies show 70% of mTBI patients experience them, though 84% of our patients report having them). They can develop after mild, moderate, or severe injuries. For many patients, the headaches develop for the first time shortly after the injury. For others, the injury causes pre-existing headaches, such as migraines, to worsen.
Whether the headaches were a brand-new symptom or a worsening of a pre-existing condition, most patients return to normal a few days or weeks after the injury. But for about 30% of patients, these headaches persist for months or even years after the injury. In addition to headaches, these patients experience a variety of persistent cognitive and physical symptoms, such as nausea, dizziness, fatigue, anxiety, difficulty concentrating, memory problems, and sleep difficulties, to name just a few. Collectively, this condition is known as post concussion syndrome (PCS).
It can be challenging for PCS patients to get the right treatment to address their headaches. The most common obstacle is that doctors don’t connect the present headaches with an incident that happened years ago. This is more likely to happen to patients with mild injuries, although it can happen after moderate or severe injuries.
For example, Samuel Gray experienced years of mysterious symptoms, including brain fog, sensitivity to sounds, short-term memory loss, depression, and severe migraines after he suffered a brain bleed as a child. His doctors believed it was some type of undiagnosable hereditary issue, and nobody made the link between the symptoms and his childhood head injury.
You can read Samuel Gray’s full head injury recovery story here.

Eventually, Samuel found Cognitive FX after one of his relatives was treated at the clinic, making the connection between the old injury and his current symptoms. Successfully treating PCS headaches is not just a matter of alleviating the pain; for long-term results, therapy needs to address the root of the problem caused by the head injury.
At Cognitive FX, we focus on getting to the root of the issue and treating it appropriately using a multidisciplinary approach. Our treatment program combines physical exercise, interdisciplinary therapies, and lifestyle recommendations to restore normal brain function and alleviate symptoms.
So what can you do about headaches that occur years after your head injury? We’ll explain…
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in the long-term symptoms of head injury. To see if you are eligible for treatment, sign up for a consultation.
Yes, Head Injuries Can Cause Headaches Years After the Incident
.png?width=1000&height=500&name=head%20injury%20headache%20years%20later%20(1).png)
Headaches that develop after a head injury are called “post-traumatic headaches,” or PTH for short.
Surprisingly, this symptom is most common in patients with mild traumatic brain injuries (mild TBIs). Over 70% of patients with mild head injuries experience headaches, while only 30% of those with moderate to severe TBIs experience them. You don’t need to experience loss of consciousness to develop long-lasting symptoms. For most head injury patients, headaches fade after a few days or weeks after the injury, but for about 30%, headaches continue for months or even years. In addition to headaches, patients can experience a range of other long-term symptoms, such as:
According to the International Classification of Headache Disorders (ICHD-3), PTH is a secondary headache disorder, which means they develop as a consequence of another disorder. This classification defines that to be considered a PTH, the headaches need to develop within 7 days of an injury. Some researchers, however, suggest that this interval needs to be reassessed. It’s not uncommon for patients to develop chronic headaches several weeks or months after an injury.
These headaches can get progressively worse over time if patients don’t seek medical attention and appropriate treatment. Finding the right approach is not always easy, but at Cognitive FX, we offer a comprehensive treatment program to treat long-term head injury symptoms, including headaches.
Types of Headaches
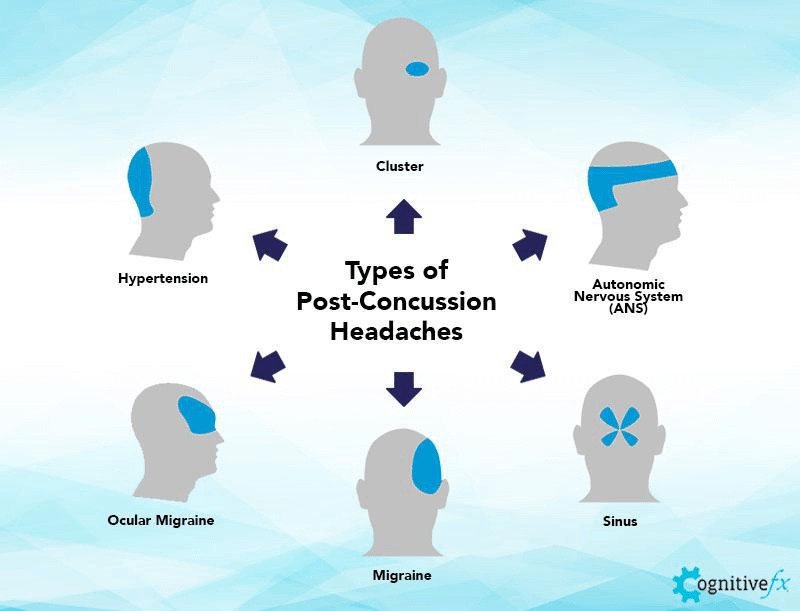
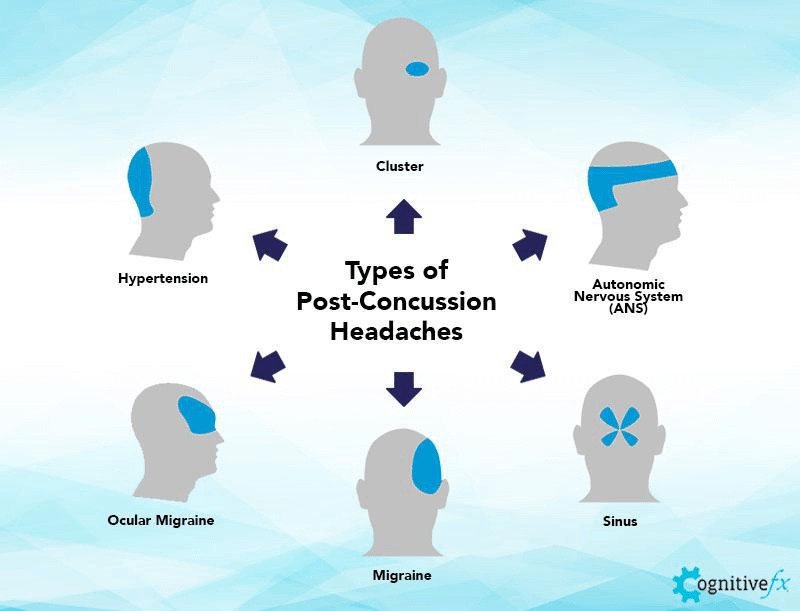
Not every post-head injury headache feels the same. Patients may experience pain at the point of impact, but headaches can also occur around the temples, the back of the head and neck, the forehead, or around the eyes. Here are some common types of post-traumatic headaches:
- Migraines
- Tension-type headaches
- Rebound headaches
- Cervicogenic headaches
- Cluster headaches
Migraine Headaches
Migraines occur when one or more areas of the brain become hypersensitive, triggering an intense pain signal that spreads out to other parts of the brain. Patients who have migraines (or have a family history of migraines) before the head injury are more likely to develop post-traumatic migraines.
The main features of migraines include:
- A dull, throbbing sensation, usually on one side of the head (but sometimes on both sides)
- Nausea or vomiting
- Light and sound sensitivity
- Moderate to severe pain
- An aura (such as seeing spots or bright lights) that precedes the pain
- Pain that worsens with physical activity
A very specific type of migraine that can develop after a head injury is called a vestibular migraine. This type of migraine comes with a wide range of other symptoms, including dizziness, lightheadedness, vertigo, and/or motion-induced sickness. These headaches can persist for months or years after the injury.
Patients may also experience ocular migraines, which typically involve loss of vision in one or both eyes and a headache. They are sometimes referred to as visual migraines, ophthalmic migraines, or monocular migraines. The headache associated with an ocular migraine tends to affect one side of the head with a throb or pulsating sensation and feel worse when moving around. It can also cause nausea, vomiting, sensitivity to light, and blind spots or colored halos in vision.
Tension-Type Headaches
Tension-type headaches occur when there has been some injury to the muscles and soft tissues in the back of the head and neck. Patients can experience pain in the neck, shoulders, back of the head, and sometimes at the top of the head. Alongside migraines, these headaches are one of the most common types present in patients with a brain injury. Up to 40% of patients experience this type of headache during the first year after a concussion.
These headaches may:
- Be continuous or come and go
- Feel like something is pressing or squeezing on both sides of the head
- Worsen from the stress of physical activity
- Range from mild to moderate in pain level
- Tend to occur late in the day
- Worsen from neck movements and muscle tension
- Include sensitivity to light and sound
- Last a few minutes or a few hours
- Gradually increase in intensity
- Worsen from stress
Tension-type headaches also include headaches caused by dysfunction of the autonomic nervous system (ANS). Patients experiencing this type of headache often report pain starting from the jaw and moving across the face over the top of the head or affecting the sinus area, with pain around the cheekbones.
Rebound or Medication Overuse Headaches
Sometimes, patients experience headaches caused by the meds used to treat them. This can happen with prolonged use of over-the-counter or prescribed painkillers.
Features of these headaches include the following:
- Caused by long-term use of painkillers
- Improved by stopping painkillers
- Often mistaken for the headache that the patient is already experiencing
- Often accompanied by neck pain and consequently mistaken for cervicogenic headaches
- Experienced most often in the morning
- Accompanied by poor sleep
Cervicogenic Headaches
Cervicogenic headaches are associated with neck pain and often occur after whiplash. They are caused by problems with the cervical spine (vertebrae in the neck region) and muscles in the neck and shoulders. Neck movements and pressure or stress can trigger this type of headache and worsen symptoms.
Common features of cervicogenic headaches often include:
- Headaches that start at the back of the head and shoulders
- Dizziness and balance issues
- Pain that ranges from mild to severe
- A dull, “pulling” feeling around the neck
- Reduced range of motion in the neck
- Gradually worsening symptoms
Cluster Headaches
Cluster headaches are rare after a head injury but can be extremely painful. They are characterized by pain behind one eye that can occur in cyclical patterns or clusters. Attacks can last for weeks or months, followed by a period of remission.
Features of cluster headaches often include:
- Excruciating head pain behind or around one eye radiates to other areas of the face
- Redness of the eye
- A stuffy or runny nose
- Pale skin or flushing on the affected side
- Drooping eyelid on the affected side
- Sensitivity to light and sound
90% of our patients report reduced symptoms after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.
What Causes Headaches Years After a Head Injury?
-1.png?width=1000&height=445&name=head%20injury%20headache%20years%20later%20(10)-1.png)
Headaches that persist or recur for years after a head injury are most likely caused by one or more of the following:
- Autonomic Nervous System (ANS) dysfunction
- Neurovascular Coupling (NVC) disruption
- Vision problems
- Vestibular problems
- Untreated whiplash
- Sleep disturbances
- Psychological problems
Autonomic Nervous System (ANS) Dysfunction
The autonomic nervous system (ANS) controls many vital body functions, such as heart rate, blood pressure, gastrointestinal responses, contraction of the urinary bladder, focusing of the eyes, and thermoregulation. Often involved in post-head injury dysfunction are two subsections: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS helps the body respond to stressors, while the PNS helps the body conserve energy under resting conditions (such as by decreasing heart rate and lowering blood pressure).
In a healthy body, these two sections work together, swapping dominance as needed. After a head injury, however, this dynamic can be disrupted. For most patients, that means the SNS stays in charge most of the time, keeping the body in a constant state of stress. This leads to various symptoms, including fatigue, sleep disturbances, memory problems, headaches, and more.
Further reading: Dysautonomia after a head injury
Some patients describe ANS headaches as feeling like their head is blowing up like a balloon or like there’s a tight clamp around their head. Others complain of neck pain and headaches around the back of the head to the temples. Some experience the headaches across the jaw or the sinus area. Finally, some report pain over the top of the head.
If your symptoms get worse after physical exercise, then it is likely that your headaches are caused by ANS dysfunction. Despite this, it’s very important to engage in regular exercise to help with your recovery. There are steps you can take to exercise safely after a head injury.
Stress can also exacerbate autonomic nervous system dysregulation.
Caffeinated drinks and alcohol provide pain relief for a short period, but they make headaches worse over time. Our advice is to avoid them as much as possible or consume with moderation.
Further reading: Post-concussion caffeine and alcohol
Neurovascular Coupling (NVC) Dysfunction
Brain cells get the resources they need — oxygen and nutrients — from a network of blood vessels in the brain. As the cells are called upon to complete a task, they “request” what they need, which is then delivered to the right place at the right time by surrounding blood vessels. This dynamic relationship is called neurovascular coupling (NVC).
After a head injury, however, this connection can be disrupted. As a consequence, the brain starts to struggle to complete normal functions. Depending on the region affected, patients experience different symptoms. For example, patients may have vision problems if areas associated with visual processing are harmed.
Irrespective of the areas affected, NVC dysfunction is very taxing on the brain as a whole, leading to general symptoms such as headaches, fatigue, and irritability. The more the brain is affected by NVC dysfunction, the more likely patients are to experience headaches after a neurotrauma. If you’re experiencing headaches after cognitive tasks, you may have headaches caused by NVC disruption.
Vision Problems
When the visual system is damaged — which is common after a head injury — this area struggles to function properly and often compensates by working overtime. This puts an extra strain on the brain and causes headaches. The most common form of visual problems that can trigger headaches is binocular vision dysfunction (BVD), where the eyes are misaligned and don’t focus in the same direction. Other conditions that cause headaches include convergence insufficiency and accommodative dysfunction.
To find out if headaches are caused by visual dysfunction, patients need to be assessed by a neuro-optometrist. However, the following symptoms are common in patients with visual dysfunction:
- Frontal headache in the brow area
- Sensitivity to light
- Headache pain that impedes daily functioning or memory
- Dizziness
- Dull, stabbing, or throbbing pain around the eyes and forehead
- Double or blurry vision
- Headaches that get worse in a busy environment or when using the computer
Further reading: Vision problems after a concussion
Vestibular Dysfunction
.png?width=1000&height=445&name=head%20injury%20headache%20years%20later%20(7).png)
Head injuries can also damage the vestibular system located in the inner ear. As a consequence, the brain receives inaccurate signals about the position and movement of the body. When this happens, the brain must rely more on visual input to stabilize the head and the body than it normally would. Relying more on the eyes to help with balance leads to headaches, fatigue, nausea, balance issues, and difficulty performing routine daily activities.
In the long term, relying too much on vision to keep balance and posture causes the brain to become visually dependent. This means that, after a head injury, the brain will continue to prioritize information from the eyes and ignore vestibular input. As a result, patients may struggle to perform tasks in low light, triggering symptoms such as dizziness and headaches.
Headaches caused by vestibular dysfunction can cause the following symptoms:
- Migraines
- Severe, throbbing headaches
- Pain usually on one side of the head
- Nausea and vomiting
- Dizziness and loss of balance
- Sensitivity to light, smell, and noise
Further reading: Vestibular therapy after a concussion
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in the long-term symptoms of head injury. To see if you are eligible for treatment, sign up for a consultation.
Untreated Whiplash
As described earlier, cervicogenic headaches are common after a whiplash injury. Patients often experience pain radiating from the neck and upper shoulders to the forehead and back or sides of the head. These headaches can flare up immediately after the injury or in the days to weeks afterwards.
For some patients, whiplash symptoms persist for months and need specialized treatment to resolve. In addition to headaches, patients may experience weakness, difficulty talking, confusion, dizziness, nausea, and excessive tiredness.
Further reading: Untreated whiplash symptoms & treatment
Sleep Disturbances
There is strong evidence to show that sleeping disturbances after a head injury can trigger headaches, including migraines, tension-type headaches, and cluster headaches. This happens because the hypothalamus is responsible for both regulating sleep and modulating pain. If this area is damaged after a head trauma, it dysregulates sleep patterns and triggers headaches.
The pineal gland is another part of the brain involved in regulating sleep. This gland produces melatonin, a hormone that promotes feeling sleepy in the evening. If this area is affected by the head injury, low levels of melatonin can cause migraines and cluster headaches and increase the chances that patients wake up with headaches.
Further reading: Sleep disturbances after a head injury
Psychological Difficulties
Depression, anxiety, and other psychological struggles are common after a brain injury. About half of patients are affected by mental health problems within the first year after injury and a small proportion may need antidepressants.
Headaches triggered by depression are often described as dull and throbbing, with the pain usually worse in the morning but getting better as the day goes on. Researchers believe these headaches are caused by changes in the brain that occur with depression, but the exact mechanism is still a mystery.
Depression headaches are usually accompanied by:
- Fatigue
- Tension in your neck and shoulders
- Lightheadedness or dizziness
- Difficulty concentrating
- Muscle aches
- Sleep problems
- Jaw pain
While pre-existing psychological conditions are risk factors for persistent symptoms after a head injury, patients can experience headaches from depression and the like even if they did not have any psychological conditions before their injury.
Further reading: Post-concussion depression
Treating Post-traumatic Headaches Can Be Challenging
.png?width=1000&height=445&name=head%20injury%20headache%20years%20later%20(5).png)
As we’ve seen, there are multiple causes behind post-traumatic headaches, making their management and treatment very challenging. At the moment, there are currently no evidence-based treatments to suit all patients, and doctors rely only on general guidelines.
If your long-term headache is making it hard for you to work or go to school, your doctor may suggest some medication, including over-the-counter painkillers (such as acetaminophen) or specific drugs to treat migraines (such as triptans). This may help with some symptoms for some patients but should only be considered as a short-term option. We strongly discourage long-term treatment of headaches with medication because:
- It’s not FDA-approved: At the moment, there are no FDA-approved drugs to treat post-traumatic headaches.
- It’s not backed by science: There isn’t enough scientific evidence to support their use in patients with long-term headaches. One of the few studies available found that migraine medications were largely ineffective.
- It’s not suitable: Painkillers were not designed to treat PTHs. For example, doctors can prescribe triptans to treat migraines and cluster headaches. These drugs work by limiting blood flow in the brain. However, if your headache is caused by NVC or ANS dysfunction, constricting blood flow could make the problem worse.
- It’s not effective: Studies looking at different medications for headaches — including acetaminophen, over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, as well as more specific analgesics, such as lidocaine and opioids — found limited evidence to suggest that these medications are helpful for patients with long-term headaches and additionally may trigger many side effects.
- It’s not safe: Use of painkillers is not always safe for patients. In addition to rebound headaches described above, medication can cause renal failure or gastrointestinal complications such as acute gastritis and gastric ulcers, for example.
Alternative Treatments for Post-traumatic Headaches

Health care providers are becoming more aware that prescription drugs are not the best option to treat patients with persistent headaches after a head injury. Instead, neurologists and researchers are developing non-pharmacological options. Some of the options you may be offered include:
- Cognitive Rehabilitation Therapy: This therapy aims to alleviate headaches by educating patients about ways to avoid stress and understand what triggers their headaches. Studies show that it can reduce headaches, dizziness, and nausea.
- Progressive Muscle Relaxation Techniques: This intervention involves a series of exercises to tense and relax particular muscle groups in the body. Recent research shows that engaging in muscle relaxation exercises a few times per week can improve headaches.
- Cognitive Behavioral Therapy (CBT): This type of therapy is becoming increasingly popular to treat post-traumatic headaches, especially if patients also have emotional or behavioral symptoms and a history of headaches. For example, a study showed that CBT for military veterans with headaches and PTSD reduced symptoms and improved their quality of life.
- Acupuncture: There is evidence to show that this non-pharmacological technique can reduce headache pain and improve quality of life compared to standard treatments using medication.
- Physical Therapy: Physical activity can reduce inflammation in the brain and help patients with headaches. Exercise may also help relieve migraines and cervicogenic headaches by improving the range of motion in the neck and shoulders.
- Nutraceuticals: Food supplements can also be used to help with headaches and other neurological conditions, including vitamin D, riboflavin (vitamin B2), coenzyme Q, and melatonin.
- Osteopathic Treatments: There is some evidence suggesting that osteopathic manipulations, such as craniosacral therapy and neck massage, can help headaches. Sessions must be performed by a certified therapist.
- Lifestyle Changes: Lifestyle changes after a brain injury can alleviate headache symptoms and improve quality of life. Recommendations include keeping hydrated, reducing stress, and following a healthy sleep pattern.
Treatment for Years-Later Headaches at Cognitive FX
The treatments described above can be useful to treat some types of headaches in some patients, but recent evidence suggests that a multidisciplinary approach produces much better results. This is the method we follow at Cognitive FX.
One of our patients, Chris Nicastro, spent years visiting multiple doctors and specialists after sustaining several concussions as a teenager. He tried physical therapy, acupuncture, chiropractic adjustments, and many other therapeutics with very little benefit. Eventually, Chris found Cognitive FX’s website. He was skeptical at first. His doctors had convinced him that recovery from post-concussion syndrome was a slow and gradual process, so how could just one week’s treatment rewire his brain and alleviate symptoms?
The “trick” is that our treatment — called Enhanced Performance in Cognition (EPIC) — addresses the underlying post-concussion symptoms caused by the brain injury, including neurovascular coupling disruption and autonomic dysfunction, as well as vision and vestibular issues. While most patients do not recover 100% at the end of their treatment (one to two weeks) at Cognitive FX, they experience notable improvements and continue improving at home. For example, patients with a visual dysfunction component may need to spend a few more months in vision therapy before fully recovering.
What’s more, our treatment can be used to treat most types of brain injuries, whether from a mild, moderate, or severe injury (though patients with long-term symptoms from a severe traumatic brain injury may need lower expectations for recovery than someone who had a concussion). Some of our past patients have made recoveries from the long-term effects of transient ischemic attack, chemo-induced brain fog, long COVID and other illness, carbon monoxide poisoning, and more.
For Chris, asking questions of the team and watching patient stories was enough to convince him EPIC treatment was worth a try. In the end, the treatment program at Cognitive FX accomplished what months of other therapies couldn’t. He realized soon after that he was able to hang out with friends and family at a barbeque with no symptoms, play his beloved guitar again, and even do gigs with his band.

Chris Nicastro playing guitar after treatment.
Evaluation at Cognitive FX
All patients undergo an extensive evaluation, including a review of their medical history, rating past and current symptoms, and exams to assess physical, cognitive, and emotional condition.
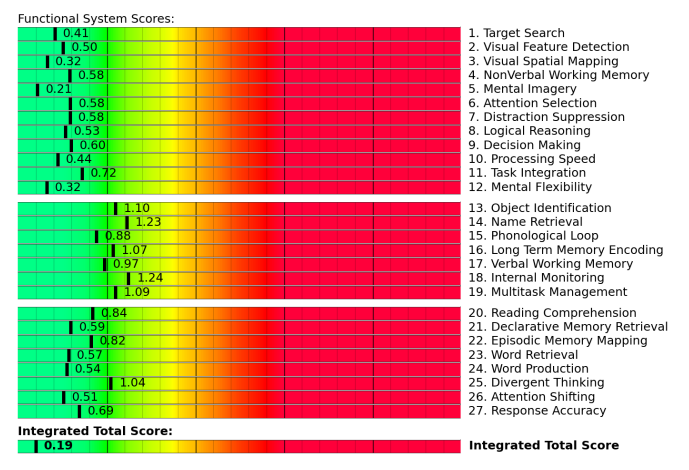
Patients also undergo a brain imaging scan called functional Neurocognitive Imaging (fNCI) scan. This brain imaging scan investigates neural functioning in 100 regions of the brain and checks how effectively these regions communicate with each other. The scan is conducted while the patients perform a series of cognitive tasks.
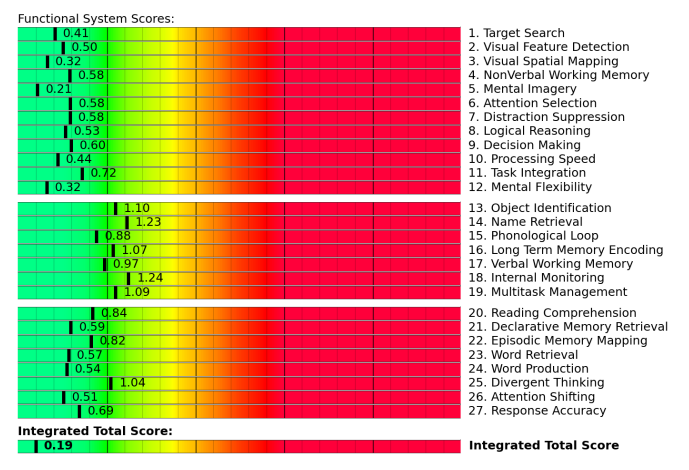
fNCI results from a patient with healthy neurovascular coupling. Scores in the yellow and red zone often indicate poor NVC.
The fNCI is a key component to post-injury treatment that other clinics do not have the resources to offer. It informs exactly where and in what way the brain was affected by injury so that the therapists can tailor their exercises to the specific injury. While the overall therapies offered are similar for each patient, the specific exercises and how they’re combined can vary considerably because they are closely tailored to each person’s injury and evaluation results. That’s why our treatment success outcomes are so consistent.
For example, Sam Pembleton tried nearly every concussion clinic near her home in Ontario and even traveled to a well-known clinic in Chicago. It got so bad that she was afraid of trying any more treatment programs. “I was scared of getting everyone's hopes up and then being sent home again because they couldn't fix me or they didn't know what was wrong with me,” she shared.
It wasn’t until she received treatment at Cognitive FX that she experienced the breakthrough she’d been seeking. That breakthrough was due to the combination of insight from the fNCI results and a multidisciplinary staff who could challenge Sam’s brain in the way that she needed.
“I think the most difficult thing for people to grasp is the fact that unlike a broken bone or something, a concussion is so different for everyone. Each person’s brain is so different that one treatment may work for one person, whereas someone else may need a completely different approach,” she said. “A concussion is like a fingerprint. It's unique for each person.”
Further reading: Sam Pembleton’s concussion recovery story
Treatment at Cognitive FX
After evaluations are complete, our team of doctors and therapists design a treatment plan specific for each patient. This treatment involves a three-step cycle that is repeated throughout your time at the clinic: Prepare, Activate, and Recover.
Treatment starts with short sessions of aerobic exercises, usually on a stationary bike or treadmill, to promote healthier blood flow in the brain and to prepare the brain for therapy. Physical activity is a key part of our treatment to trigger a phenomenon in the brain called post-exercise cognitive boost (PECB). During PECB, the brain releases a series of chemicals, including a compound called brain-derived neurotrophic factor (BDNF), which boosts the impact of subsequent therapies and helps the brain adapt better to changes.

After exercise, patients engage in a series of different therapies to activate the brain and treat physical and cognitive symptoms. Therapies include occupational therapy, neuromuscular therapy, neurointegration therapy, cognitive therapy, sensorimotor therapy, vision therapy, vestibular therapy, and others. Our treatment also includes sessions with a clinical psychologist to assess and begin to address emotional symptoms. This can be especially helpful for patients whose headaches are triggered by symptoms of depression and anxiety. If our team feels patients need further support, we can make appropriate recommendations for follow-up with other specialists.

Throughout the day, patients also have periods to rest and recover, including breathing exercises to promote relaxation, neuromuscular massage of the neck and shoulders, and mindfulness exercises.
Toward the end of treatment, patients undergo a second scan to assess how their brains are recovering. In addition, patients meet with a therapist to discuss progress and receive a series of exercises to complete at home. These typically include aerobic exercises, cognitive activities, and relaxation techniques.
Most patients need to spend about an hour per day, five days a week on exercises at home but can then slowly reduce the time spent as they recover. Completing these exercises boosts your chances of a fast and complete recovery.
Additionally, you can check out our online headache treatment course that covers what types of headaches patients can develop after a head injury, as well as specific techniques for coping with this symptom.
90% of our patients report reduced symptoms after their treatment at Cognitive FX. To see if you’re a good fit for our program, sign up for a consultation.


.png?width=1000&height=500&name=head%20injury%20headache%20years%20later%20(1).png)
-1.png?width=1000&height=445&name=head%20injury%20headache%20years%20later%20(10)-1.png)
.png?width=1000&height=445&name=head%20injury%20headache%20years%20later%20(7).png)
.png?width=1000&height=445&name=head%20injury%20headache%20years%20later%20(5).png)