If you’ve started getting headaches after you’ve suffered whiplash, you’re not alone. After neck pain, headaches are the second most common symptom from whiplash. Over 60 percent of patients have headaches immediately after their injury, and many continue to experience this symptom for months and even years afterward.
Often, patients also experience a traumatic brain injury (TBI), such as a concussion, at the same time as whiplash. In this case, it can be virtually impossible to determine exactly what’s causing headache symptoms. Inevitably, this makes treatment more difficult.
As a result, most available treatments focus on managing the pain rather than treating the cause of it, but this only offers temporary relief. For example, you may have resorted to taking painkillers to deal with your headaches, but ironically, this may cause a different type of headache called a rebound headache (more on this later). Also, if you’ve tried working with a chiropractor, you may have noticed that you must keep returning as symptoms come back after a few days.
At Cognitive FX, we offer an alternative treatment that targets the underlying causes of your symptoms — including chronic headaches — using a series of mobility and strengthening exercises specifically designed to help nerves and muscles in the neck recover from the effects of whiplash. In addition, our treatment program takes a holistic approach to addressing whiplash and concussion effects — such as brain fog, emotional changes, sleep disruption, and more — using a combination of aerobic exercises and multidisciplinary therapies.
In this article, we’ll cover:
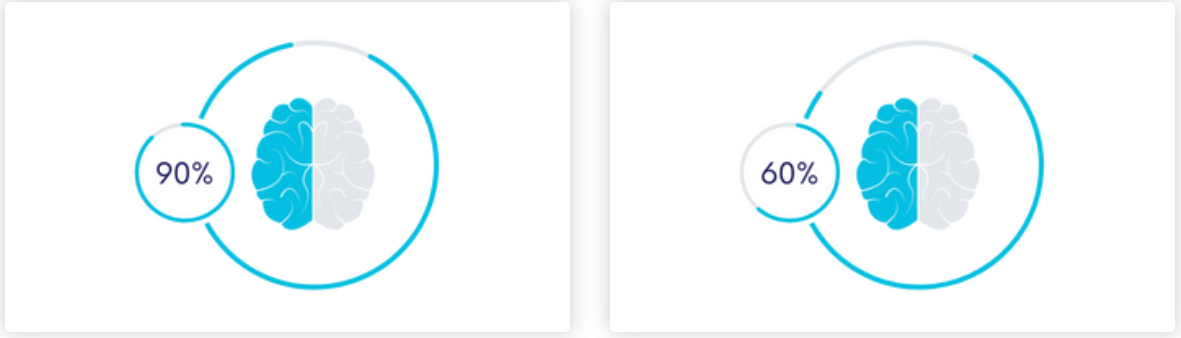
If you’re experiencing persistent headaches or other symptoms, such as brain fog, fatigue, memory problems, vision changes, and more, months or years after whiplash, know that these are real symptoms caused by changes in the brain and autonomic system, and they can be helped. Over 90% of our patients experience significant recovery after treatment in our clinic. To determine if our program is right for you, please schedule a consultation with our team.
What Are the Causes of Whiplash Headaches?

When the body senses an unusual or sudden motion — due to an auto accident or contact sports, for example — the muscles in the neck tense up to prevent the head from hitting anything. This protective response, however, is what leads to whiplash. Neck muscles, as well as other soft tissues in this region, can sprain and become damaged and inflamed, leading to headaches and soreness. For some patients, these head pains develop immediately after the injury, while for others, they take some time to appear.
Whiplash headaches (and other whiplash-associated disorders) can have a variety of causes, and it can be difficult to identify what’s causing the pain for each patient, especially in patients who have also suffered a concussion.
Some of the most common causes of headaches in whiplash patients include:
- Cervical instability
- Neurovascular coupling disruption
- Dysfunction of the autonomic nervous system
- Proprioception issues
Direct Damage to the Neck Causing Cervical Instability
The cervical spine refers to the top seven vertebrae (called C1 to C7), of which C1 and C2 are more mobile than the rest. Other structures located in this region include blood vessels, muscles, ligaments, and nerves. In a healthy person, these structures are correctly aligned and protected by the vertebrae.
After whiplash, however, patients experience localized inflammation in the neck and overextension of the ligaments in the neck, which inevitably causes cervical instability and misalignment of vertebrae C1 and C2. This affects blood flow to the brain, resulting in a variety of symptoms, including neck pain and headaches.
Neurovascular Coupling (NVC) Disruption
In a healthy brain, cells can “request” the resources (nutrients and oxygen) they need to complete a particular task from a network of surrounding blood vessels. These blood vessels then deliver them at the right time and to the right place. This dynamic connection is called neurovascular coupling (NVC).
However, whiplash alters blood flow in the brain and disrupts this link between brain cells and blood vessels. In practical terms, this means affected regions may struggle to perform their tasks. This particularly affects areas of the brain involved in pain perception and processing sensory information, which may explain chronic symptoms such as constant headaches and fatigue.
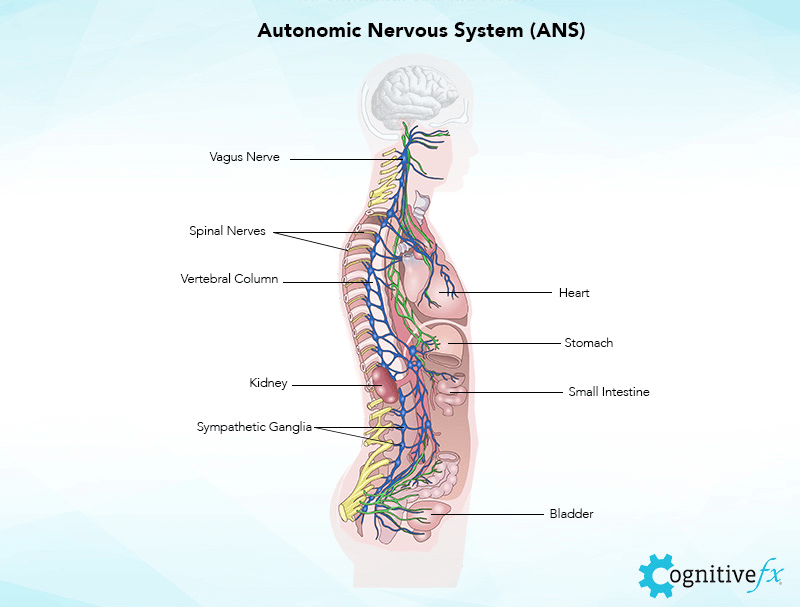
Autonomic Nervous System (ANS) Dysfunction
In addition to affecting blood flow in the brain, whiplash also has an impact on the autonomic nervous system (ANS).
The ANS includes the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS controls our fight-or-flight response to stress, while the PNS controls the rest-and-digest response by initiating a calming influence on the body. Under normal conditions, the SNS and PNS work together seamlessly.
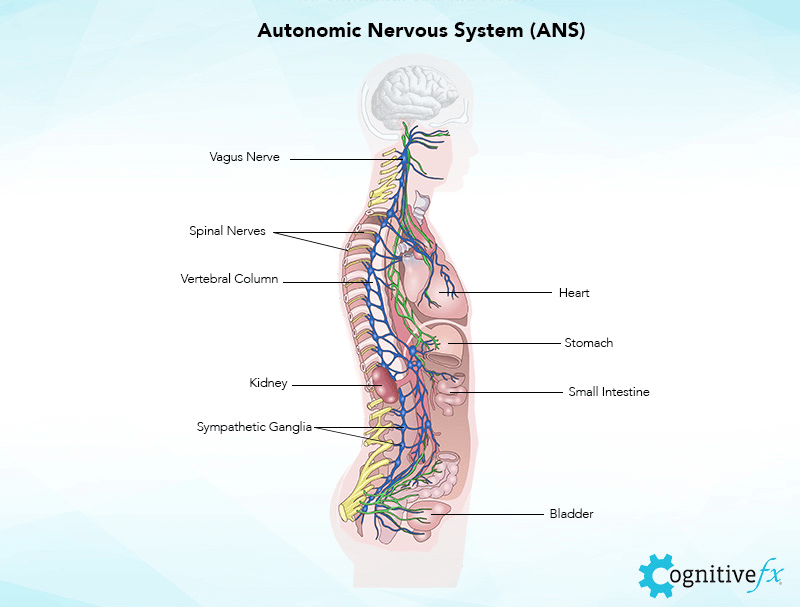
Whiplash, however, disrupts this cooperation, and the ANS often gets stuck in fight-or-flight mode. As a consequence, the brain can no longer send out the correct pain signals, and patients continue to experience chronic pain — including headaches — even when the body is no longer physically hurt.
Some patients describe ANS headaches as feeling like a tight clamp around their head, pain around the back of the head and temples, or pain across the jaw and sinus area. If you notice that pain worsens after exercise, your headaches are likely due to ANS dysfunction.
Proprioception Issues
Many whiplash patients also develop proprioception issues after whiplash. The brain receives information regarding how the body is moving (proprioception) through the nerves that pass through the neck. Based on this information, the brain then sends messages to the vestibular and vision systems to keep your posture balanced and your vision focused.
If whiplash damages these nerves, the brain may start to send and receive faulty information regarding position and movement. This causes a variety of visual and vestibular symptoms, including dizziness, vertigo, lightheadedness, spatial disorientation, light sensitivity, double vision, and eyestrain, which, in turn, may trigger headaches.
Further reading: Dizziness after a concussion
What Are the Common Types of Whiplash Headaches?
The most common types of headaches from whiplash are cervicogenic and tension-type headaches. However, it’s possible that you could experience other types of post-traumatic headaches as well, particularly if you sustained a concussion or TBI in addition to whiplash. These may include:
- Cervicogenic headaches
- Tension-type headaches
- Orofacial pain
- Cervical migraines
- Cluster headaches
- Headaches caused by neck or skull fracture
- Pinched nerve headaches
- Rebound headaches
Cervicogenic Headaches
The most common type of headache caused by whiplash is a cervicogenic headache. Typically, these headaches start a few hours after the incident that caused the whiplash. Neck movements can worsen the pain, especially if the neck is extended. For example, looking up to the ceiling can be very painful.
Common features of cervicogenic headaches include:
- Pain that starts at the back of the head and shoulders, then radiates to the temples, top and front of the head, or down the neck
- Pain that increases while texting, reading, using a computer monitor, or when moving your neck
- Pain that often affects only one side of the head
- Constant non-throbbing pain
- Dizziness and balance issues
- Pain that ranges from mild to severe
- A dull “pulling” feeling around the neck, shoulders, and upper back
- Reduced range of motion in the neck
- Gradually worsening symptoms
- Tingling or numbness in the arms
- Fatigue
- Light and noise sensitivity
- Blurred vision
Tension-type Headaches
After cervicogenic headaches, the second most common type of headache is a tension-type headache. As the name suggests, these headaches are associated with muscle tension or muscle spasms. As such, patients experience pain in the neck, shoulders, back of the head, and sometimes at the top of the head.
Typically, these tension headaches:
- Feel like something is pressing or squeezing on both sides of the head
- Worsen during physical activity
- Range from mild to moderate
- Tend to occur late in the day
- Worsen with neck movements and muscle tension
- Include sensitivity to light and sound
- Last a few minutes up to a few hours
- Gradually increase in intensity
- Worsen from stress
Orofacial Pain
Neck injuries due to whiplash can cause pain and functional impairments in the jaw. The sudden movement can cause elongation of the jaw ligaments and trauma to the jaw muscle. If not treated promptly, these symptoms may lead to orofacial pain. In medical terms, this condition is known as temporomandibular pain dysfunction disorder.
Orofacial pain after whiplash may include:
- Jaw tenderness
- Severe headache
- Jaw fatigue with eating
- Pain with eating and yawning
- Stiffness or numbness in the jaw-face region
- Clicking or popping sounds when opening the mouth
Cervical Migraines
In some patients, chronic whiplash triggers a type of migraine called trauma-precipitated cervical migraine. In most cases, these headaches start immediately or within the first few days after the injury.
The main features of migraines include:
- A dull, throbbing sensation, usually on one side of the head (sometimes on both sides)
- Nausea or vomiting
- Dizziness
- Light and sound sensitivity
- Moderate to severe pain
- An aura (such as seeing spots or bright lights) that precedes the pain
- Pain that worsens with physical activity
Cluster Headaches
Cluster headaches are less common after whiplash but can be extremely painful. Patients experience pain behind one eye that occurs in cyclical patterns or clusters. Headaches can last for weeks or months, followed by a period of remission.
Features of cluster headaches often include:
- Excruciating pain behind or around one eye, radiating to other areas of the face
- Red eyes
- Stuffy or runny nose
- Pale skin or flushing on the affected side
- Drooping eyelid on the affected side
- Sensitivity to light and sound
Headache Caused by a Fracture of the Neck
Whiplash may also cause fractures in the neck or skull, which in turn cause severe headaches. This condition can be extremely dangerous, especially if there’s bone displacement or splintering of the bone, and it requires immediate medical care.
Typically, these headaches start immediately after whiplash. The pain is generally located in the neck and back of the head. Depending on the type and severity of the fracture, symptoms may include nausea, confusion, stiff neck, slurred speech, or even seizures.
Pinched Nerve Headaches
Whiplash sometimes causes compression of the spine, which, in turn, may pinch nerves located in the neck or base of the skull. This condition — called occipital neuralgia — causes pain, tenderness, burning, numbness, and tingling from the bottom of the skull up the back of the head.
Features include:
- Sudden bursts of shooting pain in the neck region, accompanied by persistent throbbing or aching headaches that continue between the spasms.
- Pain that starts in the neck and then spreads upward
- Pain that affects the back of the head, scalp, and forehead
- Migraine-like pain
- Scalp sensitivity and tenderness
- Sensitivity to light
- Pain that worsens with small movements, such as turning the head or lying down
- Disc herniation
- Neck stiffness
Rebound Headaches
Finally, patients may experience post-whiplash headaches caused by excessive or long-term use of over-the-counter and/or prescription medication taken to treat headache pain. These rebound headaches often resemble the type of headache that prompted the medication use to begin with, which means it’s very difficult to distinguish between the headache caused by whiplash and the headache caused by medication.
The good news is that most patients improve once they’ve weaned themselves off these medications. The downside is that some medications — such as opioids — are difficult to stop taking and may cause side effects if stopped abruptly.
How Are Whiplash Headaches Diagnosed?

Diagnosing whiplash headaches is a challenging process. Typically, doctors start by examining the neck area to assess the level of damage. During this initial examination, your doctor will need to touch and move your head, neck, and arms. You may also be asked to perform some simple movements to determine the range of motion, tenderness, reflexes, and sensation in your arms.
If needed, your doctor may request a brain imaging test, such as a CT or MRI scan. Whiplash injuries are not visible on imaging tests, but these scans can be used to rule out other conditions, including fractures, bone damage, and some soft tissue injuries, such as damage to the spinal cord, discs, or ligaments.
If the scans are normal but the headaches continue, your doctor may request additional testing to assess facet injury. (Facets refer to areas of contact between two adjacent vertebrae.) This includes injecting anesthetic to the affected area, which lasts for a few hours. If the pain stops, then it’s possible to conclude that the headaches are being caused by a facet injury.
How Are Whiplash Headaches Treated?

There are various ways to treat whiplash headaches, depending on the severity of symptoms. The most common ways include:
- Physical therapy
- Chiropractic treatments
- Medication for pain management
- Spinal injections
- Surgery procedures
Physical Therapy
Physical therapy (also called physiotherapy) is the most common way to treat whiplash, which in turn will help with headaches. Patients who engage in regular physical activity (with the help of a therapist) experience less pain and recover faster than patients who avoid movement. As soon as you’ve been cleared of neck or skull fractures, you can start physio. Therapists can show you exercises to help you regain range of motion, relieve symptoms such as muscle stiffness and soreness, and restore normal movement.
To treat whiplash, physical therapy includes passive and active treatments:
- Passive treatments: These include deep tissue massage and hot and cold therapies to help patients’ muscles relax. For example, during deep tissue massage, therapists use direct pressure and friction to release muscle tension. In cold and hot therapies, therapists start with cold compresses to slow down circulation and reduce inflammation, followed by hot to promote blood flow to the area.
- Active treatments: These require you to actively participate in a series of physical exercises to improve strength, reduce muscle spasms, and increase range of motion. Some of these exercises include rotating your neck in both directions, tilting your head from side to side, rolling your shoulders, and touching your chin to your chest.
Chiropractic Procedures
Chiropractic procedures are a popular treatment for patients with whiplash. Chiropractors use spinal manipulation techniques (also known as chiropractic adjustments) to identify the neck joints that are misaligned after whiplash and reposition them into their proper place. The aim is to relieve pain by reducing pressure on the affected nerves, increase the range of movement, reduce swelling, and promote relaxation.
With that said, while spinal manipulation techniques may offer relief for a few days, symptoms often come back. Patients then need to continue visiting their chiropractor to get adjusted repeatedly. In addition, spinal manipulation can be difficult if the damage is mainly affecting the first few vertebrae (C1 and C2). Anything in this area needs an extremely gentle approach to ensure that it doesn’t cause further damage. (We’ve treated patients who sustained a concussion when their chiropractor adjusted C1 or C2 too violently.)
Unfortunately, because these adjustments often don’t resolve the underlying causes of whiplash symptoms, patients may suffer long-term effects of whiplash for months or even years.
Medication for Pain Management
Depending on the severity of your whiplash symptoms, your doctor may prescribe medication, such as painkillers or anti-inflammatory medication, to deal with headaches. It’s important to note that these medications may help relieve your pain in the short term, but they won't help heal your whiplash injury and may cause unwanted side effects such as rebound headaches.
Your doctor may recommend over-the-counter medications first, such as acetaminophen and NSAIDs (Non-Steroidal Anti-Inflammatory Drugs). If those don't help, they may prescribe stronger pain medications. The exact type of medication depends on your symptoms, but options include:
- Muscle relaxants (including benzodiazepines, nonbenzodiazepines, and antispasticity medications)
- Antidepressants
- Anticonvulsants
- Anti-inflammatories
- Opioids
Worryingly, there is very little evidence to support the use of any of these meds to treat whiplash headaches. Our advice is to avoid them as much as possible or only use them for a short period.
Spinal Injections
Your doctor may also suggest a spinal injection to give you pain relief. Usually, these injections work better when combined with physical therapy and regular exercise to strengthen neck muscles.
Examples of spinal injections used for whiplash include:
- Epidural steroid injection: This injection is used to treat pain arising from irritation of spinal nerves and discs. During the procedure, steroid medications, designed to reduce inflammation and pain, are injected into the epidural space.
- Facet Joint Injection: These injections can help patients experiencing pain and inflammation due to damage to the facets. A facet joint injection will numb the joint and reduce pain.
- Trigger point injection: In more extreme cases, your doctor may suggest an injection applied directly onto painful trigger points. These are knots of muscles that form when muscles can’t relax after whiplash. The injection contains painkillers and corticosteroids to reduce pain and inflammation.
Surgical Procedures
If the treatments described above don’t help, your doctor may suggest more radical surgery. This is usually reserved for severe cases if pain persists after non-surgical treatments have not succeeded. Some examples include:
- Cervical rhizotomy is a minimally invasive procedure used to treat neck pain and headaches resulting from damage to the facet joints. During the procedure, a special needle is injected into the nerve that carries signals from the inflamed facet joint, causing the nerve to heat up. This switches off pain signals coming from the facet. Typically, pain relief lasts three to six months.
- Endoscopic anterior cervical discectomy is used to treat patients with neck pain and headaches due to a herniated disc in the cervical region. The main advantage of this procedure is the ability to treat the affected areas and reduce pain while preserving as much of the disc as possible. During the procedure, only the damaged and herniated areas are removed; the rest of the disc remains in place to help the neck maintain strength and stability.
- Endoscopic facet debridement is a minimally invasive procedure to treat patients with neck pain originating from the facet joints. The aim is to remove dead, damaged, or inflamed tissue that is trapped between facets. By removing it, the patient can once again move freely without pain. This surgery is performed through a small incision, and patients typically have a quick recovery.
Most of These Treatments Only Offer Temporary Relief
Although the treatments described above can help reduce headache symptoms, most of them only offer temporary relief or involve complex surgeries with long recovery times.
In contrast, Cognitive FX offers a combination of aerobic exercise, multidisciplinary therapies, and mobility and strengthening exercises to address the symptoms of whiplash (and often concussion) as a whole. Chiropractic spinal manipulations are not part of our treatment. Instead, our therapists focus on retraining motor control, allowing the body to adopt better posture and move without needing to be corrected.
There are occasions, however, when we need to refer patients to a trusted chiropractor with experience dealing with whiplash. We believe combining appropriate chiropractic techniques (if needed) and our therapy program is the best way to treat whiplash symptoms, including headaches and neck pain.
In addition, most whiplash patients have also suffered a traumatic brain injury and are likely experiencing a wide range of other symptoms in addition to headaches. If these symptoms persist for a long time, patients develop a condition known as post-concussion syndrome (PCS). Our approach is designed to target the root issues of these symptoms — including headaches — such as neurovascular disruption and ANS dysfunction.
Treatment for Whiplash at Cognitive FX

We specialize in treating patients with lingering symptoms after a head injury. For patients with whiplash, we adjust our treatment protocol to address the underlying neck and autonomic issues that contribute to symptoms.
Before treatment starts, patients must undergo a detailed assessment to determine how whiplash has affected their neck and brain. Patients meet with a member of our team to talk about their symptoms and medical history. During this assessment, patients also complete a series of physical, cognitive, and psychological tests, including:
- Physical assessment to test reflexes, vision, balance, and hand-eye coordination.
- Cognitive evaluation to test cognitive skills, such as brain fog, poor memory, or difficulty focusing.
- Psychological assessment to detect signs of mental health issues, such as anxiety and depression.
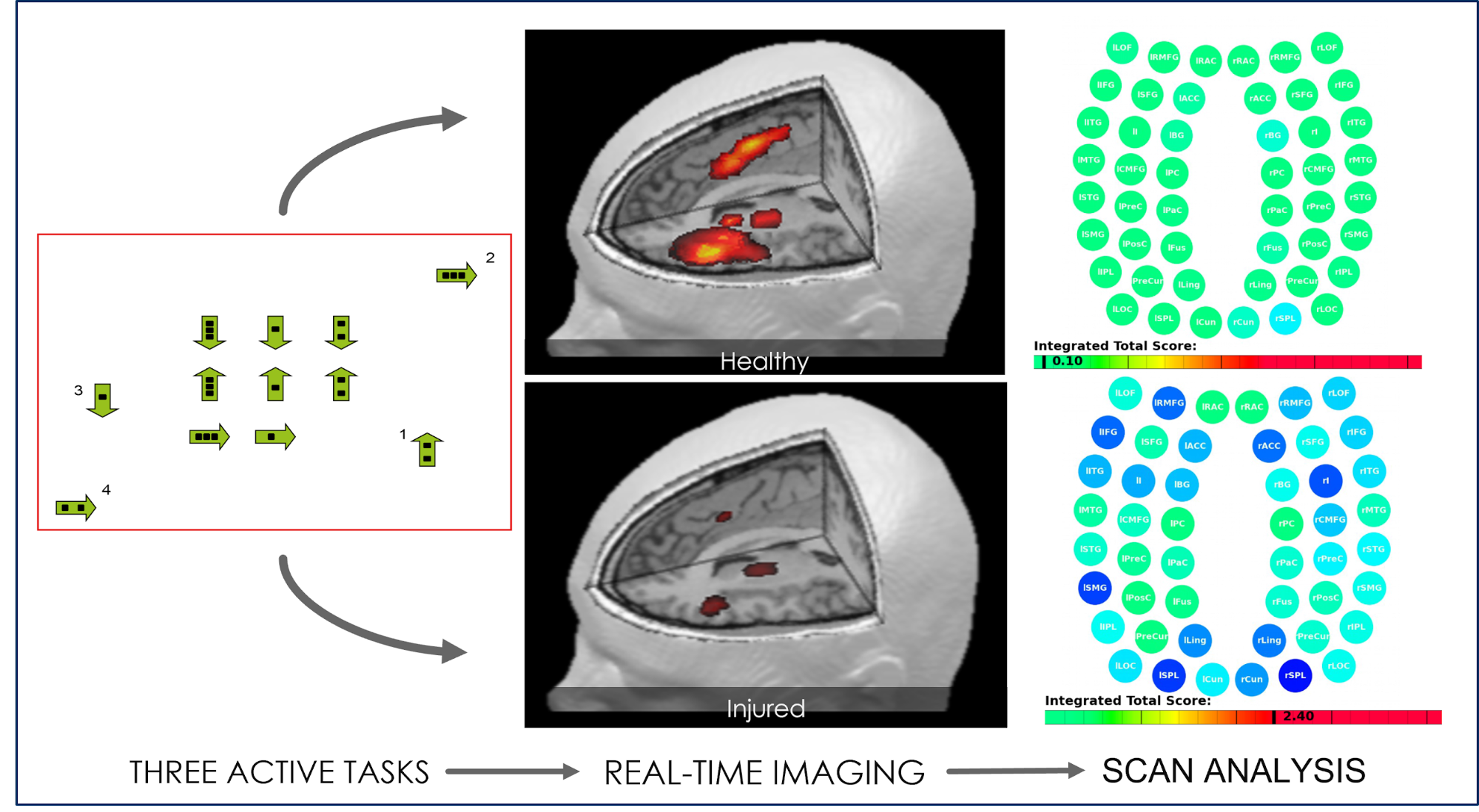
We also use state-of-the-art brain imaging technology to determine exactly how the whiplash affected the neck and brain. This scan, called functional Neurocognitive Imaging (fNCI), identifies which regions in the brain are affected by neurovascular coupling dysfunction. In practical terms, the scan looks at how blood flows in over 100 different areas in the brain, as well as how these areas communicate with each other while the patient performs a series of standardized cognitive tasks.
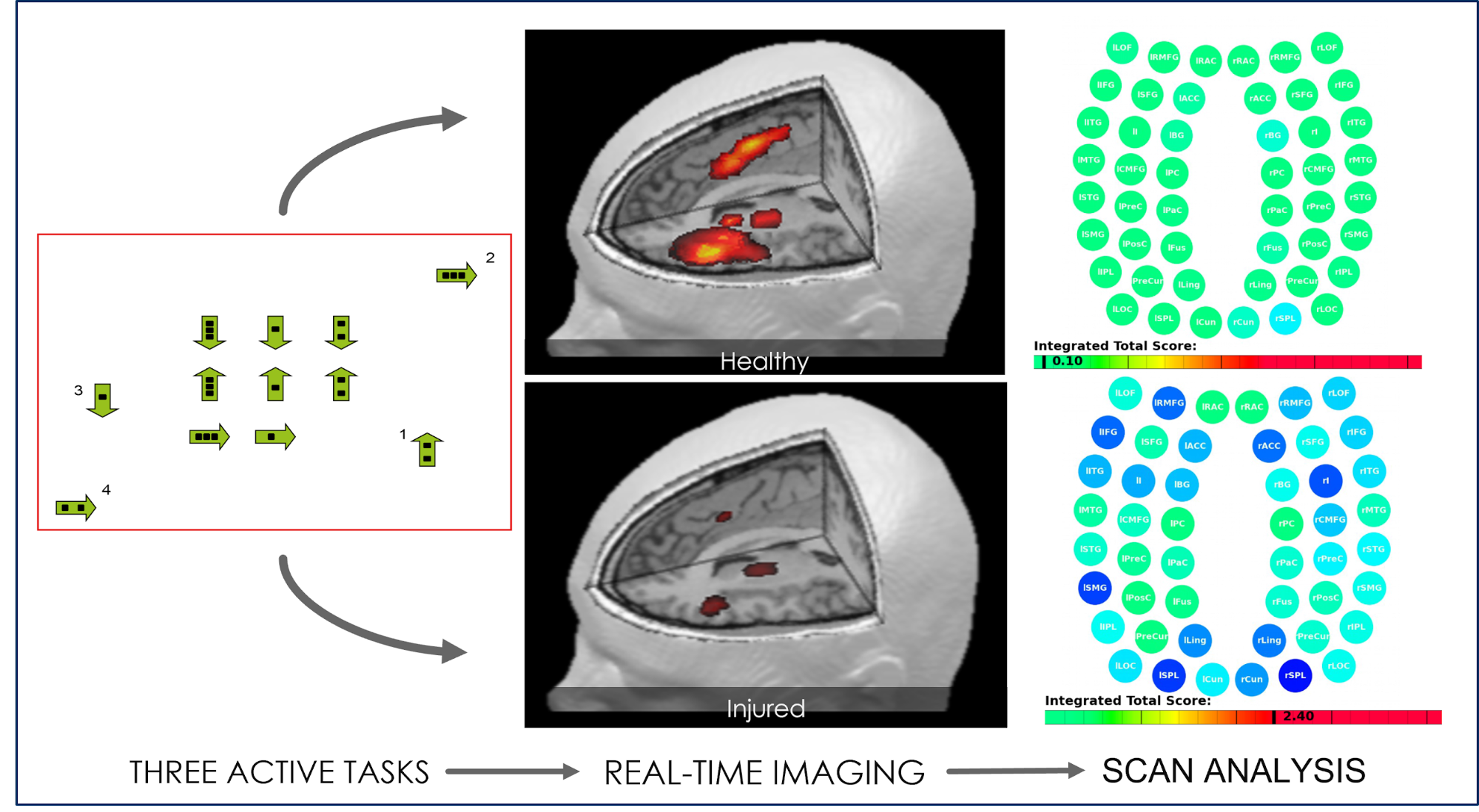
Once this initial evaluation is done, results are combined and used to design a custom-made treatment plan for each patient. We call it Enhanced Performance in Cognition, or EPIC for short. While most patients complete the same types of therapy during their treatment with us, the specific exercises used in each type of therapy are chosen based on scan and evaluation results.
For example, patients with whiplash may need more intense neuromuscular therapy along with targeted mobility and strengthening exercises. In addition, these patients attend vision and vestibular therapy sessions at the beginning of treatment to improve mobility and stability, which then allows them to take full advantage of subsequent therapies.
During treatment, patients cycle through a three-step process:

Prepare
The first stage of treatment involves a short session of aerobic exercise, usually done on a treadmill or stationary bike. Physical activity improves blood flow to the brain and promotes the release of a chemical called brain-derived neurotrophic factor (BDNF). BDNF stimulates the growth of brain cells and improves communication between different areas of the brain, helping the patient’s brain to benefit more from subsequent therapy. In addition, aerobic exercise reduces neck pain and headaches in patients with whiplash. This effect is called exercise-induced hypoalgesia.

Activate
After exercise, patients engage in a series of multidisciplinary therapies, including:
Recover
The final stage involves periods of rest and relaxation. Patients practice mindfulness, receive a neck and shoulder massage to relieve tension, or relax in a dark room while listening to binaural beats. Listening to binaural beats is done using an app that produces two similar sound frequencies that the brain averages into one frequency, encouraging the brain to rest.
After treatment, patients undergo a second scan to see how much their brain has changed. In addition, patients also meet with a member of our team to discuss their results and receive a series of exercises to do at home. This homework usually includes physical exercises, cognitive activities, and relaxation techniques, and it’s one of the best ways to speed up recovery at home. Our advice is to engage in these exercises for about one hour, four to five times a week at first, and then gradually decrease the frequency as symptoms improve. Finally, if our therapists feel that patients may benefit from further therapy, we recommend suitable specialists.
In our experience, patients who suffered whiplash and a concussion can take a little longer to recover than if they just had a concussion. After therapy, many patients experience improvements in symptoms such as fatigue and brain fog but still have neck and back pain. With continued treatment, however, we believe full recovery is possible for most of these patients.
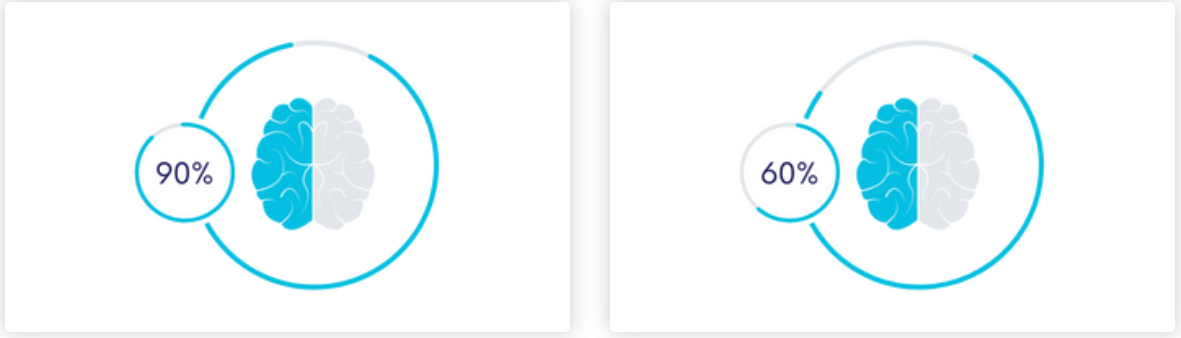
On average, 90% of our patients see improvement in their reported symptoms over the course of treatment, with symptoms decreasing by 60% on average.
To determine if our program is right for you, please schedule a consultation with our team.
Aimee, one of our patients, suffered the long-term effects of a car accident for 17 years before finding Cognitive FX. Here’s what she experienced from treatment:
What Can You Do to Cope with Whiplash Headaches at Home?

Coping with constant headaches can be extremely painful and distressing. Here are a few suggestions to help you manage your headaches and whiplash syndrome at home:
Engage in Light Stretching Exercises
At home, you can do some light stretching exercises immediately after your injury to decrease pain and improve motion. Start slowly and gradually increase as you feel better. If you experience severe pain during these exercises, stop right away and go back to your previous level. The most important message for whiplash patients is to not be afraid to move; not moving can significantly delay your recovery.
Exercises may include:
- Rotating your neck in both directions
- Tilting your head side to side
- Bending your neck toward your chest
- Rolling your shoulders
Other Useful Exercises
Other useful exercises include gargling, humming, or swallowing to stimulate some of the nerves running through your neck. For example, these exercises stimulate your vagus nerve (which crosses the neck) and activate your parasympathetic nervous system, which in turn calms the body and reduces pain.
Another is tongue positioning. The ideal rest position for the tongue is on the roof of the mouth, away from your teeth. Keeping the tongue in this position lowers neck and jaw pain and reduces the number and intensity of headaches. This works because the muscles of the tongue can stabilize the cervical spine even without you thinking about it. Correct tongue positioning can help the rest of the neck muscles that tend to get tight when they’re overcompensating for post-whiplash changes.
Apply Ice and Heat
As described earlier, ice and heat treatments can help relieve headaches. You need to apply ice to the neck to reduce pain and swelling during the first few days after the whiplash incident. Once the swelling is down, you switch to heat on the same areas to loosen the muscles and encourage blood flow to the soft tissues. You can also try to alternate between cold and heat for maximum relief.
Follow a Consistent Sleep Pattern
Not sleeping properly can aggravate headache symptoms and cause cognitive issues, such as poor memory and difficulty focusing. A few suggestions for a good night’s sleep include:
- Go to bed and get up at the same time every day, including holidays and weekends.
- Restrict daytime naps to 20–30 minutes, ideally shortly after lunch.
- Drink chamomile tea before bed; this type of tea has anti-inflammatory properties and also works as a muscle relaxant.
- Place a towel under your neck for support while you sleep.
- If the bed's too uncomfortable, try sleeping on a reclining chair or sofa.
- Make sure you sleep with your mouth closed. This helps to reduce jaw and neck pain.
Follow a Healthy Diet and Keep Hydrated During the Day
Eating a balanced diet can help you recover faster from your whiplash and control your headaches. Some suggestions include:
- Eat plenty of fruits and vegetables and avoid sugary and fatty processed foods.
- Make sure you drink plenty of liquids throughout the day. Dehydration can aggravate your headache.
- Avoid stimulants such as alcohol and caffeine. These drinks may give some temporary relief, but in the long term, they aggravate your condition and delay your recovery.
Practice Mindfulness and Breathing Exercises
Learn mindfulness or breathing techniques and practice them at home to relax. This helps to dampen the sympathetic nervous system, improves blood flow in the brain, and reduces headaches.
Our headache relief masterclass was developed specifically to help with post-traumatic headache pain relief.
Try Essential Oils
Some essential oils can help relieve your headaches. These include, for example, peppermint, lavender, and eucalyptus. You can try diffusing essential oils in your room or rubbing a small amount on your wrists or temples.
Ready to start your recovery journey at Cognitive FX? Schedule a consultation with our team.