Can Post-Concussion Syndrome Cause Stuttering?
Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
“Post-traumatic brain injury syndrome” refers to long-term repercussions from concussions and other head injuries. Someone using this term could be referring to one of three conditions:
At first glance, these conditions have similar symptoms, but there are crucial differences among them.
In this article, we answer the following common questions:
Over 90% of our patients experience significant symptom improvement after just one week at our clinic. We target injured brain regions as identified on the fNCI, a brain imaging scan that looks at 56 brain regions and their communication patterns. To see if you are eligible for treatment, sign up for a consultation.

The most common long-term consequence of a concussion — and the one we’ll explain in most detail in this article — is post-concussion syndrome (PCS), also known as persistent post-concussion symptoms.
PCS occurs when symptoms of a mild traumatic brain injury (mTBI) last longer than expected after the initial injury. Treatments for PCS are often applicable for patients with persistent symptoms from any brain injury.
For most patients, concussion symptoms are short-lived; the brain and body return to normal functioning a few days or weeks after the injury. However, up to 30% of these patients experience symptoms for longer than three months. If the symptoms cannot be explained by other conditions, they likely stem from post-concussion syndrome (PCS).
Patients with PCS can experience a wide range of symptoms, including physical, cognitive, and emotional issues. Some of these symptoms appear immediately after the concussion and stay for a long time, while others come and go in waves. For example, a PCS patient might experience (a) fatigue that sets in immediately and doesn’t leave, (b) headaches that come and go in waves, and (c) insomnia that starts to set in after a few months.
It’s also common for the nature of the symptoms to change over time. Physical and cognitive issues might set in right away or come later. Emotional issues such as mood swings and depression often take time to develop.
Here are some common PCS symptoms and common post-injury diagnoses:
|
Cognitive |
Physical |
Mental Health |
|
|
|
PCS patients often experience a wide range of physical symptoms.
For these patients, the most common issue is headaches and migraines. Up to 90% of PCS patients experience frequent or long-lasting headaches for months after the original injury. Dizziness and balance problems are also common symptoms reported in about 25% of patients diagnosed with PCS.
This condition can also affect the patient’s senses. About 14% of PCS patients develop vision problems, including blurred or double vision, about 10% develop sensitivity to light or noise, and about 5% experience a decreased sense of taste or smell.
PCS may also cause trouble sleeping: insomnia, difficulty falling asleep, or waking up frequently during the night. Nausea and other digestive problems may also be related.
Many PCS patients experience symptoms that affect cognitive function, such as difficulty concentrating and processing information, struggling to follow a conversation, or getting easily distracted.
For example, up to 25% of patients who have PCS still experience some memory deficits more than 12 months after the original injury.
Psychological conditions are present in about half of PCS patients, including irritability, apathy, anxiety, depression, and a perceived change in personality.
Other emotional and behavioral symptoms include restlessness, aggression, mood swings, and reduced tolerance to stress.
Post-concussion syndrome is usually caused by a combination of one or more of the following common causes:
Post-concussion symptoms derive primarily from dysfunctional neurovascular coupling (NVC).
Under normal circumstances, brain cells receive the resources they need — oxygen and nutrients — from a network of blood vessels in the brain. This dynamic connection is called neurovascular coupling.
After a concussion, NVC may be disrupted in some areas in the brain. As a consequence, brain cells in those areas don’t get the right resources at the right time. If you try to do a particular activity that those cells control — like reading a book or focusing on a conversation — you may struggle to complete the task. Other neural pathways may attempt to complete the process, but these less efficient paths tire the brain.
NVC dysfunction is incredibly taxing on the brain, leading to common symptoms such as headaches, feeling overwhelmed, and irritability. In addition, you may experience a variety of symptoms depending on what areas of the brain were affected. For example, if the concussion affected areas of the brain involved in forming memories, you may struggle with long or short-term memory. If it affected parts of the brain involved in speech, you may struggle to find the right word in a conversation or experience slurred speech.
A concussion may also affect the autonomic nervous system (ANS).
The ANS regulates vital body functions, including heart rate, blood pressure, and breathing rate. Two major subsections of the ANS are the sympathetic nervous system (SNS), which activates our “fight or flight” response, and the parasympathetic nervous system (PNS), which is responsible for our “rest and digest” mechanisms. In simple terms, the SNS is active if you're stressed and worried about something, and the PNS brings everything back down with a calming influence.
In a healthy person, the SNS and the PNS work together in harmony. In PCS patients, the SNS tends to stay activated most of the time. This constant overactivation affects normal brain and body function, leading to a series of symptoms such as fatigue, headaches, high blood pressure, digestive issues, problems sleeping, mood changes, and more.
Further reading: Autonomic nervous system dysfunction after a TBI
The pituitary gland, the hypothalamus, and the fragile pituitary stalk that connects them are easily damaged during a concussion. The effects of this damage are incredibly varied because of the large number of hormones that are potentially impacted. Hormone dysfunction can go undiagnosed for months or years if your doctors don’t think to check for it (or don’t use the right diagnostic tests). Some symptoms include emotional changes, fatigue, dizziness, vision problems, weight changes, cold or heat intolerance, and more.
Further reading: Post-concussion hormone dysfunction
Vision issues triggered by head trauma are another source of symptoms. Brain injuries can affect the way your brain and eyes communicate with each other, as well as disrupt function in brain areas that process visual information. As a result, patients may experience changes in peripheral vision, eye teaming (how the eyes work together), depth perception, and focusing. These issues can cause headaches, tired eyes, double vision, and difficulty reading, among others.
Further reading: Vision problems after concussion
Vestibular dysfunction can also lead to PCS symptoms. The vestibular system, located in the inner ears, controls balance and helps the body understand where it is in space at all times. Your body, eyes, and inner ear work together to send information to the brain, which synthesizes all information it receives and makes needed adjustments based on how you’re moving. If this information is wrong or mismatched, you may experience dizziness, nausea, and difficulty balancing.
Further reading: Vestibular therapy for PCS
Concussions and neurotrauma can cause breathing problems. After injury, patients may experience breathing problems, such as shallow or irregular breathing and/or shortness of breath. As a result, patients may feel dizzy and tired as they struggle to carry out their daily tasks.
Further reading: Can PCS cause breathing difficulties?
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in therapy for persistent brain injury symptoms. To see if you are eligible for treatment, sign up for a consultation.

Symptoms patients experience after a traumatic brain injury can be vague and attributable to a variety of other reasons. In addition, as there is no definitive test to confirm a PCS diagnosis, it’s not always easy for medical practitioners to assess and diagnose these patients.
In most cases, doctors have to rely on reported symptoms, combined with physical and cognitive tests and perhaps a CT (computerized tomography) or MRI (magnetic resonance imaging) scan of the head, to rule out other causes of symptoms, such as bleeding in the brain or a skull fracture. However, structural MRI scans and CT scans do not detect PCS because concussions cause subcellular damage and functional changes in the brain (such as NVC disruption), but these imaging techniques can only detect structural changes such as cell death, bleeding, and tumors.
Further reading: Can MRI detect PCS?

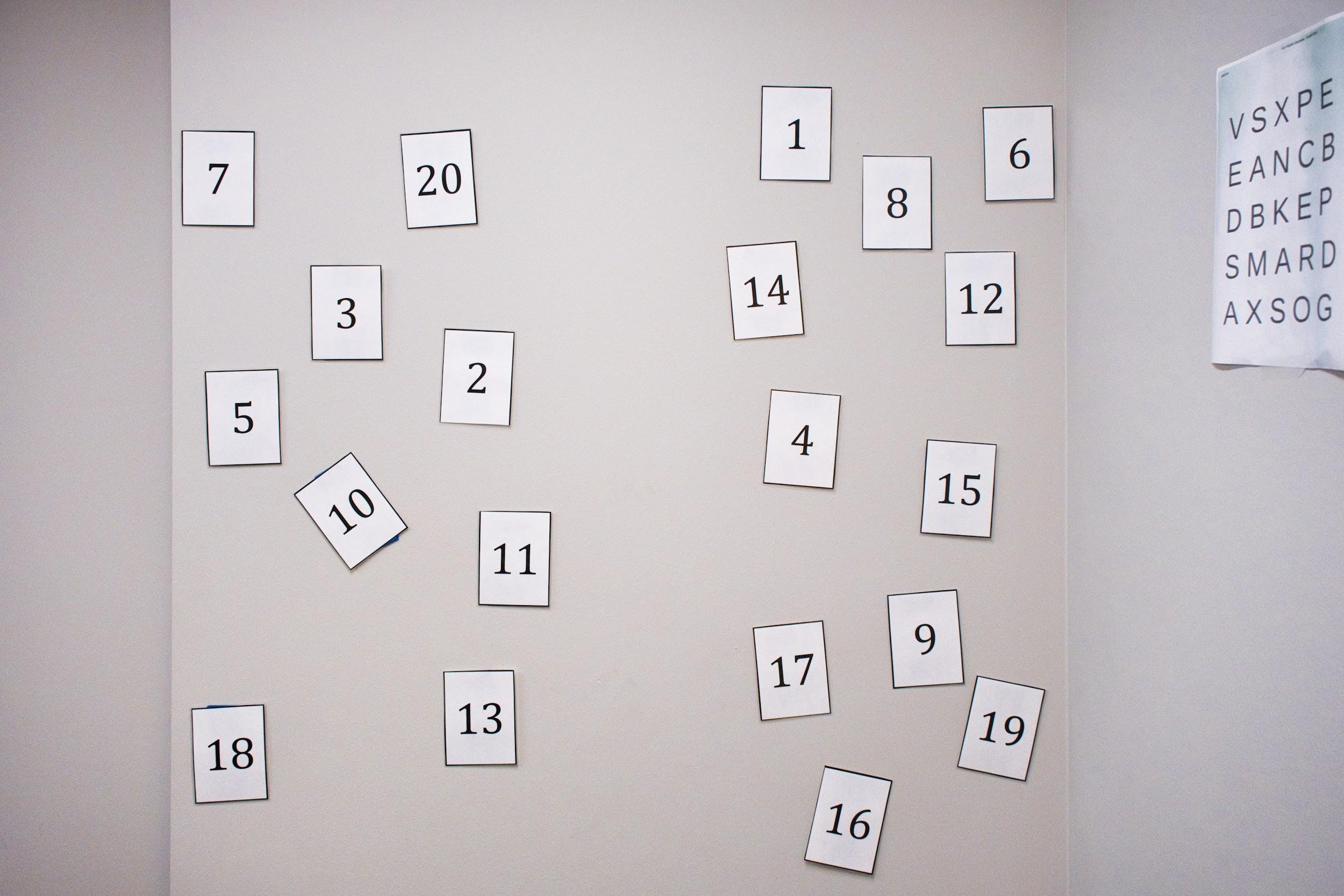
In addition to self-reported symptom scales, physical evaluation, and cognitive testing, Cognitive FX evaluates all patients via a brain scan called functional Neurocognitive imaging (fNCI). fNCI is a type of functional MRI which looks at blood flow patterns throughout the brain.
We use fNCI to evaluate NVC functioning in 56 brain regions and communication patterns between the regions. During the scan, the patient carries out a series of cognitive tasks which activate those regions of the brain. The scan allows our therapists to identify exactly which areas of the brain are affected by PCS.
Some patients have issues localized to just a few brain regions, while others have widespread dysfunction throughout the brain. Knowing what’s happening with each patient helps us design a treatment regimen that targets those specific areas.
Many patients are nervous before the scan but come away feeling validated, knowing that their symptoms are rooted in a treatable condition that can be objectively identified.

Myrthe van Boon fell while skiing and never felt the same since. After years of dismissive doctors and normal test results, she worried that visiting Cognitive FX would be more of the same.
“I was so anxious before I went because I had the feeling there would be nothing from the scan. That they would say again, ‘Sorry, we cannot find anything.’ But all the problems that I experienced were in the scan. So that was an emotional moment. After all those years, to think, ‘Wow, it is in my brain, and the things that I thought were wrong are,’” she said.
The Saturday after she finished treatment, her family went for a walk to a waterfall in the morning, and then she and her husband went to a football game. “That was amazing,” she said. “It was a crowded stadium with fireworks and lots of noise and I enjoyed it!” After that, they went out to eat and even went shopping later. It was already a huge change: Previously, even one activity in the day could overwhelm her. But that day, she could handle four — a level of activity she’s consistently able to achieve when needed.
Read more of Myrthe’s story here.
Most health care providers, such as neurologists and other specialists, treat PCS by addressing individual symptoms. For example, patients experiencing migraines and headaches will be prescribed painkillers; those with digestive problems may get anti-nausea medication. Those with depression and anxiety may visit a psychologist or psychiatrist to receive therapy or be prescribed antidepressants. But there are many problems with using medication to treat PCS, such as:
Some patients may benefit from some of the medications for a short period of time, but the vast majority who visit Cognitive FX find that prescription drugs are doing them more harm than good.
For a detailed discussion around this subject, see our post on medications and post-concussion syndrome.

At Cognitive FX, we use a multidisciplinary therapy regimen to tackle the root causes of post-concussion syndrome.
Many PCS patients struggle with exercise (known as post-exercise malaise), but rehabilitating post-brain injury exercise tolerance is a key part of treatment. Patients complete a series of guided aerobic exercise sessions to improve blood flow and trigger the release of helpful neurochemicals in the brain. This post-exercise cognitive boost (PECB) helps your brain get better results from therapy.
Specific types of exercise also counteract the dominance of the SNS, which — as described earlier — is responsible for many symptoms of PCS. The right form of exercise can also improve mood, nausea, headaches, and issues with balance and coordination. Our therapists help patients to keep their symptom levels manageable while progressing to more strenuous activity.
After exercise, patients complete a series of therapies, including:
With each therapist, patients complete activities designed to target and improve specific areas of the brain.

For example, you may be asked to balance on one leg and touch specific buttons as they light up on a board, which helps with vision and balance. As treatment progresses, exercises may become more complex. You may need to balance on a Bosu ball while throwing a ball back and forth with our therapist and solving cognitive puzzles at the same time. This intensity encourages the brain to find better ways to process information and respond to challenges, which results in healthier neurovascular coupling. (Read more about neuroplasticity-based therapy methods.)
Therapy is challenging, but many patients feel excited and validated as they feel their brain begin to ‘wake up’.

Anthony Loubet suffered a concussion in a motor vehicle accident that seriously impacted his cognitive performance and emotions. On Tuesday during treatment, he struggled to remember words that began with a ‘g’. They just weren’t coming. But as he slept that night, something clicked.
“When I woke up at 5 a.m., all these words were just flooding into my head,” he said. “Granite, graphite, grass, green, German, germane… It was like a print queue — like everything had been held up, and now there’s paper in the printer. I was exhausted, but I didn’t feel super tired because things started coming quicker to my head. I hadn’t felt like that since the accident.”
Read more of Anthony’s post-concussion syndrome recovery story here.
At the end of treatment, patients undergo a second scan to see how much their brain has improved. They and their family members also meet with a member of our team to discuss the results and develop a plan for continued recovery at home. Typically, this plan includes a series of exercises to do at home, such as aerobic exercises, cognitive activities, and ways to rest.
Completing these exercises usually takes no more than one hour, five days a week, and will help tremendously in speeding up the recovery process at home. As patients return to normal activities, they can decrease the time they spend on this homework, but they need to make sure they keep exercising as part of their regular routine.
Over 90% of our patients experience significant symptom improvement after the first week at our clinic. To see if you are eligible for treatment, sign up for a consultation.
As described earlier, PCS is only one of the long-term problems caused by concussions. Patients can also develop chronic traumatic encephalopathy (CTE) or second impact syndrome (SIS).
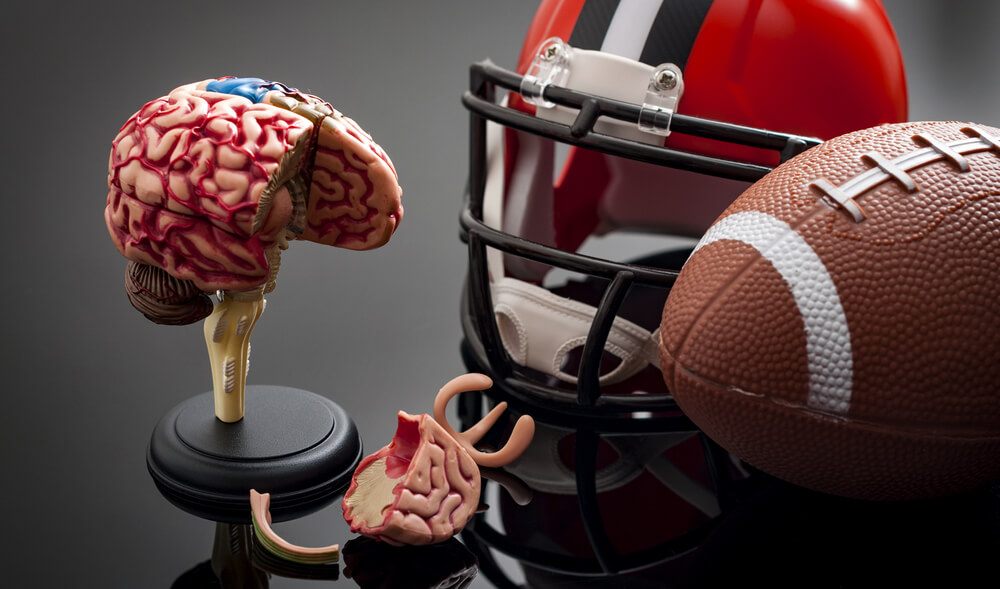
Chronic Traumatic Encephalopathy (CTE) is a progressive neurodegenerative condition found in some patients with a history of multiple head injuries. Even head injuries and contusions that did not cause symptoms may contribute to CTE.
CTE is more common in athletes who participate in contact sports such as boxing, football, and rugby. It also may affect military personnel exposed to explosions. When it was first identified in boxers in the 1920s, it was originally termed “punch drunk syndrome” or dementia pugilistica.
The repeated concussions trigger progressive degeneration of brain tissue, including a build-up of a protein called tau. That’s the same protein seen in patients with Alzheimer’s disease. But the pattern of accumulation of tau in CTE is different from Alzheimer’s. These changes in the brain take years to develop, and symptoms may start decades after the last brain trauma. Common symptoms of CTE include:
At the moment, the only way to confirm CTE is with a postmortem neuropathological analysis. Doctors make a presumptive diagnosis based on symptoms and a physical and neurological/neuropsychological exam. They also review how many times the patient suffered brain injuries and may recommend certain brain scans, such as a CT or MRI scan, to rule out other conditions.
Just as dementia is not reversible, there’s no cure for CTE. However, it’s possible to alleviate some of the symptoms with medication and therapy, such as cognitive therapy, physiotherapy, vestibular therapy, vision therapy, and occupational therapy. There are also a number of lifestyle choices, such as engaging in regular exercise and eating a healthy diet, that may delay progression of symptoms and allow patients to live independently for longer. Whether or not treatment at Cognitive FX can delay CTE progression is under research.
If you’re concerned and want to discuss your options with our staff, request a consultation.

Second Impact Syndrome (SIS) — also known as repetitive head injury syndrome — describes the occurrence of severe brain damage after a second head injury that is sustained while a patient is still recovering from a previous concussion. Even a minor blow to the head can be enough to trigger the damage, and it’s usually fatal.
There have been very few confirmed cases of SIS to date, and the exact incidence and how the condition progresses are not well known. In fact, it’s still controversial whether or not SIS truly exists, in part due to the lack of supporting evidence. At the moment, SIS is not recognised by the World Health Organization (WHO).
Typically, patients who develop SIS collapse within a few minutes of the second impact and need immediate medical attention. After they collapse, the condition then worsens rapidly with loss of consciousness, loss of eye movement, dilated pupils, and then respiratory failure. As this is such a life-threatening emergency, patients must be transported immediately to the nearest emergency department (ER) to receive medical care for brain swelling and life-threatening symptoms. The aim is to stabilize the patient and avoid respiratory failure. Neurosurgery may be needed.
Patients who survive SIS often suffer neurological symptoms equivalent to severe traumatic brain injury, which can severely affect their quality of life. These include difficulties with speech, poor cognitive skills, poor vision, impaired hearing, and emotional problems such as depression and anxiety. These patients may benefit from treatment at Cognitive FX, depending on the extent of the brain damage.
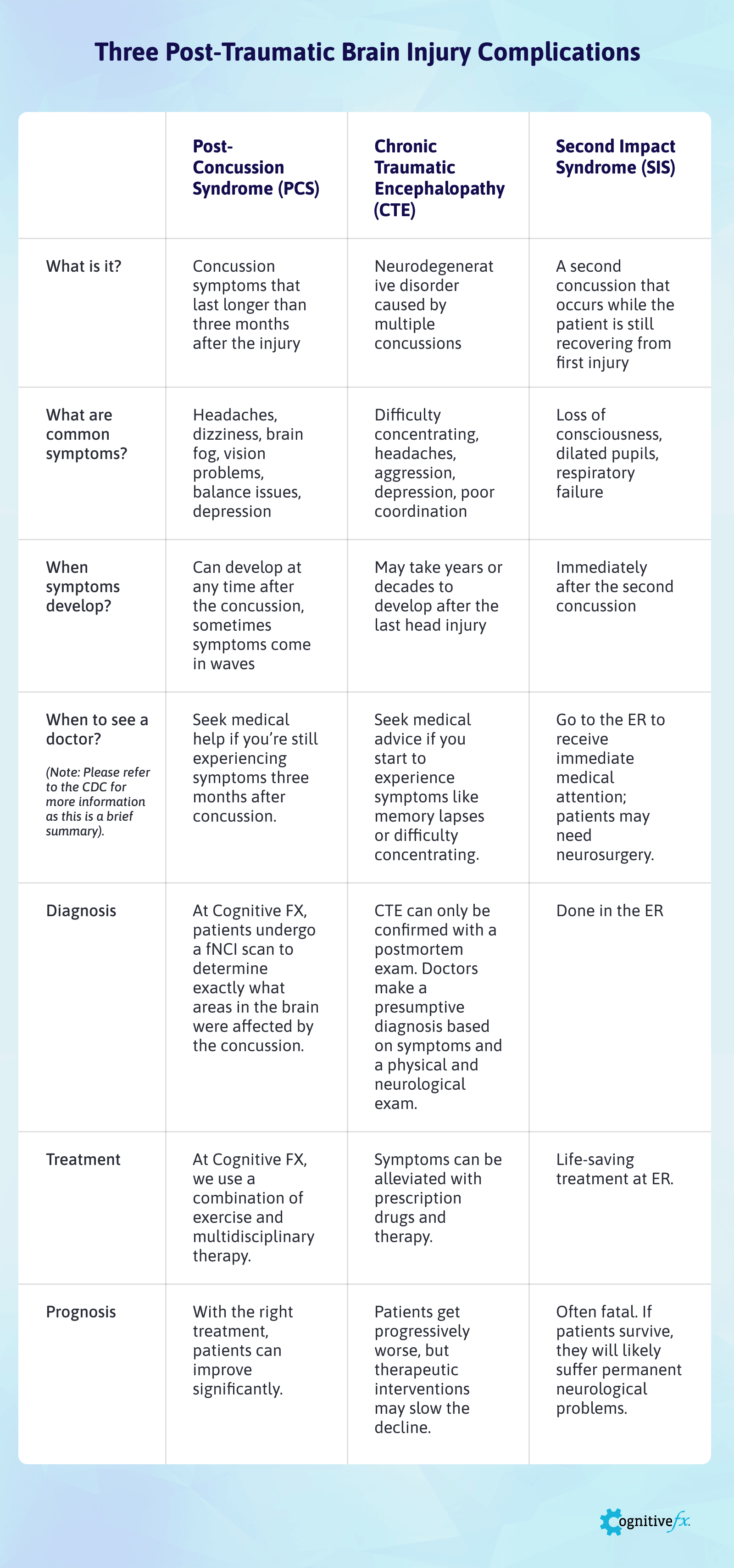 Click here to view and download the full size table.
Click here to view and download the full size table.
This table provides an easy way to summarize the information contained in this article. It includes the major differences between these three conditions in terms of diagnosis, treatment, and prognosis.

Coping with these conditions is not easy. Patients need to adapt to their particular situations, but some general lifestyle choices promote health and well-being. Multiple studies (see below) show that a combination of good nutrition, physical activity, and mental and social engagement can help alleviate symptoms for PCS patients or delay disease progression for CTE patients. There are no studies looking specifically at SIS survivors, but we believe the same advice applies.
A heart-healthy diet — low in sugar and fat and rich in vegetables and fruit — is considered to be good for both the body and the brain. An example is the Mediterranean diet, which promotes eating plenty of fruit, vegetables, nuts, and grains, while limiting consumption of processed sugary and fatty foods.
For example, a study showed that a diet rich in vegetables and fruits can slow down progression of symptoms and reduce inflammation in CTE patients. The advice for PCS patients is to boost protein intake, get omega-3s from good sources, and avoid junk food.
Further reading: Nutrition for brain injury recovery
Physical exercise has been associated with improvement of mood and mobility, along with a decreased risk of falls. Physical activities that are socially engaging — such as walking or swimming with a friend — can be especially enjoyable.
Exercise also improves mood, reduces anxiety and depression, reduces headaches and neck pain, and can help you sleep better. This is true for both PCS and CTE patients.
Further reading: How to overcome post-concussion exercise intolerance
Patients should be encouraged to get involved in activities that are mentally stimulating, such as doing crossword puzzles, learning how to play a new musical instrument, or playing strategy board games.
Anything that can help PCS and CTE patients think quickly, recall information, make decisions, or solve problems can be helpful to keep their brain engaged and stimulated.
Further reading: 17 cognitive exercises for PCS patients
Disrupted sleep is common in both PCS and CTE patients. These conditions can negatively impact memory and thinking and aggravate other symptoms that patients may have. Tips for a better night’s sleep include:
Further reading: Post-concussion sleep problems
For patients recovering from a traumatic brain injury, rest is key. It gives the brain a chance to recover and helps alleviate symptoms in the moment, such as brain fog or headaches. The brain has a limit to how much stimulation it can tolerate before patients start experiencing symptoms.
Frequent breaks during the day allow patients to cope and safely return to their activities. Keep in mind that “rest” doesn’t just have to mean a nap. There are many ways to approach rest after a brain injury which you can explore in the ‘further reading’ below.
Further reading: How to rest your brain after injury
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in therapy for persistent brain injury symptoms. To see if you are eligible for treatment, sign up for a consultation.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...

Recovering from post-concussion syndrome (PCS) is challenging, but with the right guidance, substantial progress and symptom relief are possible, even years after the initial injury.

Post-concussion syndrome is downright frustrating to experience. Doctors often miss it during diagnosis, and even if they do make the diagnosis, treatment methods vary considerably from clinic to...

What should you do when your concussion symptoms don’t go away?

Many people are surprised to learn that concussions can have long-term effects if left untreated. Chronic concussion syndrome is a less common term for persistent post-concussion symptoms (also known...
In post-concussion syndrome (PCS), a patient with a mild traumatic brain injury (mTBI) experiences persistent symptoms from the injury. If left untreated, the symptoms might last months, years, or...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY