Vision problems are common after a traumatic brain injury (TBI) and can remain for months, or even years if left untreated. Many patients experience some form of visual dysfunction, such as blurred vision, light sensitivity, difficulty focusing, and poor depth perception. Moreover, these vision problems can trigger (or aggravate) other lingering symptoms, such as dizziness, balance problems, and headaches. Not surprisingly, these symptoms can significantly impact the patient’s daily activities, including reading, driving, working, and engaging in recreational activities.
To treat these issues, it’s common for patients to receive corrective or specialized glasses, such as prism glasses (discussed below), in combination with vision therapy. However, while these treatments can certainly improve your symptoms, they often aren’t the most effective method of resolving visual issues after a brain injury.
The reason is that post-TBI visual issues are often the result of dysfunctional brain signaling, autonomic dysfunction, and other functional changes to the brain that glasses and vision therapy alone cannot address. These treatments must be combined with other therapies to address your symptoms holistically.
At Cognitive FX, we follow a multidisciplinary approach to treating lingering symptoms from TBI. We use a combination of physical exercises to prepare the brain, followed by therapies to address your specific symptoms, including visual deficits, difficulty concentrating, headache, brain fog, fatigue, emotional dysregulation (anger, anxiety, depression, teariness, etc.), short-term memory problems, and sleep issues.
In this post, we provide an in-depth overview of what TBI patients should know about experiencing vision problems after a TBI.
We cover:
In addition, before we wrap up, we walk through how we treat visual issues and other lingering symptoms from TBI at Cognitive FX.
Note: If you’re experiencing symptoms (such as vision problems) that won’t resolve after a traumatic brain injury, you’re not alone. 95% of our patients experience statistically verified restoration of brain function. To see if you are eligible for treatment, sign up for a consultation.
What Visual Symptoms Can Occur After a Traumatic Brain Injury?

Before we get to the visual symptoms that are common after TBI, it’s important to make a distinction between visual acuity (the ability to see shapes and objects clearly at a given distance) and visual processing. Many of our patients are given the all-clear when they pass a standard vision exam with 20/20 (a measure of visual acuity). However, the visual system is a collection of skills including acuity, peripheral awareness, depth perception, and eye movements/tracking. Patients can have great visual acuity, but have issues with other aspects of their visual processing system that cause them to experience symptoms.
To understand how visual processing works, it’s helpful to understand how your eyes and brain work together. When you look at something, your eyes detect light and turn it into coded nerve signals that travel through the optic nerve to your brain. Your brain receives and decodes this information and turns it into the image you see.
Depending on what you’re looking at, your brain uses different areas working together to process and understand the picture. For example, reading this sentence involves areas in the brain responsible for understanding language and recalling memories. That’s how you can see the words, understand them, and remember what they mean.
It’s also important to note that vision is not just about “seeing” things; eyes are an essential part of your balance system. The brain uses visual information to map the surrounding space, allowing you to navigate it safely.
Head injuries can damage any part of the visual pathway, from the optic nerve to the brain areas that process visual information. Consequently, patients may suffer from various visual issues that vary in severity from mild to severe.
The following are visual problems that TBI patients can experience after a head trauma.
Abnormal Eye Movements
Traumatic brain injury patients often experience abnormal eye movements.
Pursuits (the ability of the eye to follow a moving target) and/or saccades (the ability of the eye to follow from one point to another) can become unstable and “jerky” after a TBI. As a result, patients often struggle to scan and read lines of print, catch moving objects, or track nearby cars while driving, for example.
It is our view that these types of vision problems are a significant contributing factor to lingering symptoms from TBI. Evidence suggests that patients with persistent symptoms are more likely to have these types of vision problems when compared with patients who had a faster recovery.
Nystagmus is a particular type of eye movement deficit that can develop after a head injury. This condition is characterized by involuntary shaking of the eyes from side to side, up and down, or in a circular motion. The involuntary eye movements often stem from an imbalance in the vestibular system, which is critical for maintaining balance. Specifically, mismatched signaling from the vestibular nerves — one side sending more signals than the other — causes the eyes to move uncontrollably, leading to the visual perception of shaking. This affects the quality of visual information received by the brain, causing symptoms such as vertigo or nausea because the brain interprets the visual information as if the objects around are moving. Additionally, this mismatch in vestibular input can make the person feel as though they are falling, exacerbating feelings of disorientation and discomfort.
Problems with Focusing
In normal vision, the eyes can effortlessly transition focus between objects that are near and far. This process is known as accommodation and allows objects to look clear when you focus on them. Accommodation deficits are extremely common after a head injury. Patients may struggle to focus on objects that are near or switch attention between targets that are far and near. As a result, patients experience blurred vision, eye pain, and eye fatigue.
Problems with Binocular Vision
Binocular vision — also known as eye teaming — refers to how the brain combines the images seen by each eye into one focused 3D image. For this to happen, the eyes need to be aligned perfectly. Brain injuries, however, can disrupt this mechanism, and the eyes stop functioning as a team.
Convergence insufficiency is one of the most common vision conditions affecting binocular vision after a mild traumatic brain injury, affecting up to half of all patients. Many of these patients experience these symptoms for weeks after their injury. Symptoms are not always obvious, with many patients reporting vague complaints of headaches, fatigue, and balance issues that are related to convergence insufficiency. For athletes, for example, this may affect their performance because they struggle to follow a moving ball.
Loss of Depth Perception
Brain injuries may cause patients to lose their depth perception. Known as stereopsis, depth perception allows us to see in 3D and distinguish the length, width, and depth of objects, as well as estimate how far they are from us.
Depth perception also needs accurate binocular vision to ensure that both eyes focus on a single object at the same time. A patient with poor depth perception may struggle to reach out for objects, such as grabbing a cup on the table, climbing stairs safely, or driving.
Blurred Vision
Patients often experience blurred vision after a brain trauma. Even a mild injury can damage the muscles around the eye or the optical nerve itself, which causes blurred vision because the eyes struggle to work together when focusing on different objects. Some patients experience a constant blur, while others can see clearly once they focus on something but struggle to shift focus to another object.
Double Vision
Double vision — a medical condition known as diplopia — is a common symptom after a brain injury. Patients see two overlapping images of a single object at the same time. This happens because the brain is unable to merge the information it receives from both eyes. Double vision is extremely disorienting. Patients appear clumsy, spill things often, knock things over, and struggle walking up or down stairs.
Loss of Visual Field
Parts of the visual field can be affected after a brain injury. Patients may see black patches or fuzziness in particular areas of their field of vision. This is called hemianopia (when patients lose half the visual field) or quadrantanopia (when patients lose a quarter of the visual field).
When this condition affects the outside edges of the field of vision, patients experience loss of peripheral vision. This can be very disorienting, and patients may struggle to see objects that are not in the center of their field of vision, bump into things when walking, and may also have difficulty reading long lines of print.
Sensitivity to Light
Head injuries may cause increased sensitivity to light to the point where it causes severe discomfort or pain. About half of concussed patients, for example, experience this symptom. This condition is called photophobia. This symptom can be triggered by particular light sources, such as bright sunlight and fluorescent lighting. LCD screens, used for computers or smartphone devices, can also become intolerable after a brain injury.
Flashing Lights
Flashing lights — called photopsia — is a common visual disturbance after a TBI where patients experience brief, flash-like stars in front of the eyes. This is usually a temporary symptom resulting from the spontaneous firing of neurons in the occipital lobe after the impact and interpretation of these random electrical impulses as stars by the brain.
Sometimes, patients see pixelated flickering dots throughout their field of vision. This condition is called visual snow syndrome, and there is no effective treatment at the moment.
Visual Processing Disorders
In addition to the most common problems described above, a TBI may also trigger visual processing disorders. In this scenario, the eyes function normally and transmit accurate information to the brain, but the brain fails to process this information correctly, leading to a range of symptoms, including:
- Visual agnosia: TBIs sometimes cause patients to be unable to recognize objects but still understand what the object is used for. For instance, a patient with visual agnosia may be able to describe the shape of a key, how it feels, and what it is used for but still can’t identify the object as a ‘key.’ This condition is often caused by damage along the pathway connecting the areas in the brain that process visual information (occipital lobe) and the areas that allow us to make sense of what we’re seeing (parietal and temporal lobes).
- Face blindness: Also known as prosopagnosia, face blindness is a specific type of agnosia. After a TBI, patients cannot interpret and recognize faces, including loved ones or famous faces. In severe cases, patients may even fail to recognize themselves. This condition occurs when a specific part of the brain responsible for processing faces — known as the fusiform face area — is affected.
- Visual neglect: This is extremely rare, but after a TBI, some patients cannot process visual information on one side even though they can see it. This is sometimes referred to as ‘hemineglect.’ They may, for example, leave food on half of their plate or only brush their hair or teeth on one side. While this is, strictly speaking, a problem with attention rather than vision, it’s easily misdiagnosed as a visual problem unless careful observation or testing is done.
- Color vision changes: Most cases of color blindness occur from birth, but this condition can also develop after a brain injury. In this case, it’s called cerebral achromatopsia. After the brain injury, patients see colors differently, often paler versions or, in more severe cases, just shades of gray. Loss of color vision can take the enjoyment away from things like food or hobbies. It can also be a concern for drivers if the patient struggles to identify traffic light colors.
- Blindness: Complete vision loss after brain injury is extremely rare. For patients to experience full blindness after a TBI, there must be significant damage to the optic nerves, the visual pathways, and specific areas of the brain. It may also happen after a penetrative injury, such as a gunshot injury. In most cases, this is only temporary, and vision eventually returns.
- Problems with motion vision: Medically known as akinetopsia, this is the ability to identify moving objects, such as people walking or cars driving. When brain injuries affect the patient’s ability to determine motion, things may appear as static images rather than smoothly moving objects. This is often connected with balance issues, and patients can feel dizzy in busy environments such as grocery stores, social settings, or sporting events.
Secondary Symptoms
Despite the long list of visual problems caused by a brain injury, it’s not uncommon for patients to fail to notice these problems, especially if they’re mild. Patients, however, are more likely to see the consequences of these problems, including a series of secondary symptoms such as:
- Dizziness and balance problems: Our body relies on input from the visual system to help us maintain balance and navigate space in the physical world. As such, problems with vision can cause dizziness, vertigo, and balance issues.
- Headaches and eye pain: Patients who need to constantly strain their eyes because of problems with focusing are likely to also develop headaches and pain around the eyes.
- Fatigue: Patients with vision problems also report feeling tired and overwhelmed. This is not surprising as the brain has to put extra energy into finding alternative ways to process visual information.
- Sleep disturbances: Sleep problems are common after a head injury, which may aggravate problems with vision and cause ocular discomfort, dry eyes, and itching.
Impact of Visual Problems on Daily Life
Not surprisingly, many daily activities can be affected by visual problems. Perhaps the most obvious is reading. Patients skip lines, see letters “moving” on the paper, or struggle to read on a computer monitor. Sustained attempts to read cause fatigue, headaches, and eyestrain. Patients may find audiobooks or text-to-speech readers helpful.
Visual impairments also make driving very challenging after a head injury. This can be extremely dangerous for workers who need to drive heavy machinery, for example. It may be sensible to stop driving or have a driving assessment, even if you feel that your driving skills remain intact. Some states require a formal evaluation performed by a licensing bureau before resuming driving after a brain injury.
Visual symptoms caused by a head injury can even make a simple day out with friends challenging. For example, patients with poor depth perception may struggle to walk around in a busy restaurant or shopping center. It can be helpful to discuss your problems with your friends and arrange to meet in an environment that is comfortable and safe for you, such as your home or a quiet location.
How Does a Traumatic Brain Injury Cause Vision Problems?

There are several ways in which brain injuries can cause eye problems. In most patients, it’s likely to be a combination of various factors, including:
Direct Damage to the Visual Cortex
Any direct damage to areas of the brain involved in processing visual information can cause vision symptoms. This includes, for example, the visual cortex located in the occipital lobe at the back of the head, as well as the parietal lobe, which helps us recognize the physical space around us, and the temporal lobe, which controls visual memories.
Dysfunction of the Autonomic Nervous System
TBIs can also disrupt the Autonomic Nervous System (ANS), which in turn causes vision symptoms.
The ANS includes the sympathetic nervous system (SNS), which helps the body respond to an emergency (fight or flight mode), and the parasympathetic nervous system (PNS), which supports a calm and resting state (rest and digest mode). In a healthy brain, the SNS and PNS work together to control a variety of bodily functions, such as breathing rates, heart rate, blood pressure, and pupil size.
Head injuries, however, can break this balance. For most patients, the SNS takes control even if it’s not an emergency situation, keeping the body in a constant state of alert, which can be very stressful for the brain. SNS dominance causes changes in how pupils react to light, for example. Patients experience slow pupil dilation, making it difficult to adapt quickly when the light changes, causing light sensitivity.
Disruption of the ANS is also responsible for a variety of other PCS symptoms, including fatigue, sleep disturbances, memory problems, and headaches.
Neurovascular Coupling Disruption
Visual problems can also be the result of failure in the way that brain cells receive the resources they need.
Under normal circumstances, brain cells request what they need to perform a particular from a network of surrounding blood vessels. These resources are then delivered to the right place and at the right time thanks to a dynamic relationship called neurovascular coupling (NVC).
However, TBIs can disrupt this mechanism, affecting normal brain function. If this disruption involves any of the areas of the brain linked with visual function (as described above), it causes visual symptoms.
Mismatched Signaling
Some vision-related symptoms develop because the brain, the body (via proprioception, the body’s ability to sense movement), the vestibular system, and the eyes are not working together properly.
For your brain to form a clear picture, information needs to be consistent from these three sources. After a brain injury, signals from one or more of these sources become mismatched, and your brain has to work harder to figure out where you are in space and what’s around you.
Pre-Injury Visual Deficits
Sometimes, patients develop visual symptoms after a brain injury because they already have pre-existing visual deficits that they didn’t know before the injury. The brain has an impressive ability to adapt to vision issues and can find ways to compensate for them without patients experiencing any symptoms. After a brain injury, however, the brain struggles to continue compensating for those visual deficits, and, as a result, conditions that didn’t previously bother patients can become troublesome.
How Are TBI Vision Problems Treated?

When TBI patients are experiencing eye problems, it’s common for them to visit general optometrists or ophthalmologists. These are medical doctors qualified to examine and treat eyes. However, if you’re having visual problems after a brain injury, the problems often aren’t with your eyes’ physical integrity. Rather, the problems are a result of issues with the relationship between the visual system and neurological processes.
Therefore, most patients have better success at practices with a neuro-optometrist or neuro-ophthalmologist which specialize in treating these issues.
The most common method of treating patients with vision symptoms caused by a brain injury is with neuro-optometric rehabilitation. This personalized treatment addresses specific visual deficits, including problems with accommodation, focusing, eye teaming, and tracking. The aim is to “rewire” the brain using specific tools and eye-training exercises.
To begin, patients need to undergo a comprehensive eye examination conducted by an optometry expert. This includes standard tests to assess visual acuity (20/20 vision), as well as tests to check visual tracking, eye teaming, depth perception, accommodation, peripheral vision, and other visual functions that may have been affected by the brain injury.
Based on the results from your assessment, neuro-optometrists, neuro-ophthalmologists, or other vision providers decide on the best course of action for treatment. The frequency of sessions, specific combinations of therapy exercises, and the duration of treatment depend on the severity of your condition. A vision therapy program can range from several weeks to several months.
Some treatment options include:
- Corrective eyeglasses: For patients with blurry vision, regular eyeglasses may be recommended. Glasses that can magnify objects can be helpful for up-close activities such as reading or using a cell phone. If you already needed glasses before your injury, you may need a new prescription to adjust to any changes. Patients who require glasses for both near and far vision often find using bifocals challenging. In this case, it may be preferable to have separate glasses for reading and distance vision.
- Specialized glasses, such as prism glasses: These glasses have a prism attached to the lens that changes how the light reaches the eye, which can help with double vision, visual field loss or other visual field defects.
- Patching: Covering one eye (or part of one eye) is sometimes used to help patients with double vision. The patch is carefully placed to remove the information that results in the double image forming in the brain.
- Balance boards: Patients with balance issues can do exercises on a balance board. Standing feet shoulder-length apart on a balance board allows patients to learn to re-adjust their vestibular and visual systems. This can be combined with other exercises to improve focus and eye teaming.
- Computer-based vision therapy: This type of therapy uses computerized technology to treat vision problems. Patients learn to use specialized software and hardware, providing interactive visual experiences designed to improve their visual processing abilities. Sessions may include games, puzzles, and other engaging activities designed to challenge and improve the patient’s visual processing skills.
- Vision therapy: Vision therapy involves a series of exercises and activities designed to improve eye tracking, focusing, eye teaming skills, and many other visual skills. The aim is to improve the functioning of the muscles that control eye movements as well as help the brain process visual information more efficiently.
The options described above may be enough for some patients with a mild injury, but most patients need more than just neuro-optometric rehabilitation.
As we discussed above, in addition to vision problems, patients may experience a variety of other symptoms, including cognitive issues, headaches, and emotional challenges. These patients need a multidisciplinary and integrated approach to address the root problems caused by their head injury rather than a treatment that addresses only one type of symptom. This is what we offer at Cognitive FX. Vision therapy and other neuro-optometric tools are necessary to help resolve visual symptoms, but they’re only a part of the puzzle.
Treatment at Cognitive FX: A Holistic Approach to Treating Lingering Symptoms From TBI

Instead of treating visual symptoms in isolation, our treatment — called Enhanced Performance in Cognition (EPIC) — is an intense, individualized program designed to treat each patient’s specific symptoms, including vision problems.
Before treatment begins, we perform a thorough vision assessment as part of our evaluation process. Our visual exam includes:
- Saccades: Testing the patient's ability to accurately move the eyes from one designated focal point to another in a single, quick movement.
- Convergence/Divergence: Testing how a patient’s eyes rotate inward (converge) and outward (diverge) as an object moves closer or farther away, helping to assess depth perception.
- Peripheral vision: Testing the patient’s awareness and ability to see the edges of their visual field without moving their head.
- Visual processing: Testing the patient’s ability to “See, Process, and Respond” in different situations. For example, following a coordination chart where one prompt is a cue for the right hand, another for the left, and another for both. We assess how accurately and quickly a patient can complete this task.
(In daily life, this would relate to seeing a traffic light turn yellow and then red. Do you see the light change and react appropriately and in time?)
- RightEye exam: Eye-tracking software that assesses subtleties of how a patient’s eyes are moving, which eye muscles are working properly, and which aren’t.
Importantly, we assess each of these skills from a functional and a neurological perspective. In addition to looking at the specific function itself, and how well the patient is performing it, we also look at the nerves and brain regions responsible for these tasks. This allows us to most effectively rehabilitate these skills.
However, vision is just one of several physical and cognitive systems that we assess before developing a treatment protocol. Our evaluation also includes:
- A meeting with one of our doctors to review the patient’s medical history and symptoms.
- A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
- A neurocognitive test to assess memory, concentration, reasoning, and other cognitive functions.
- A psychological evaluation to identify symptoms of anxiety, depression, and other mental health problems.
- A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
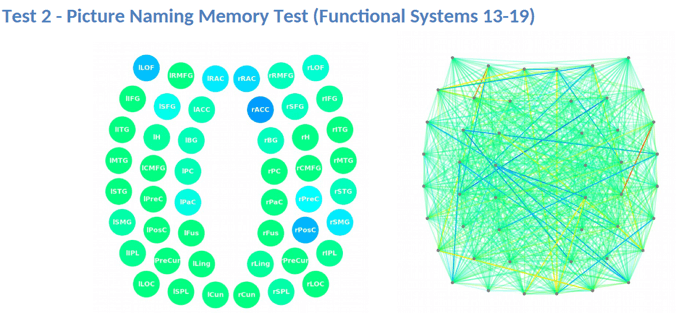
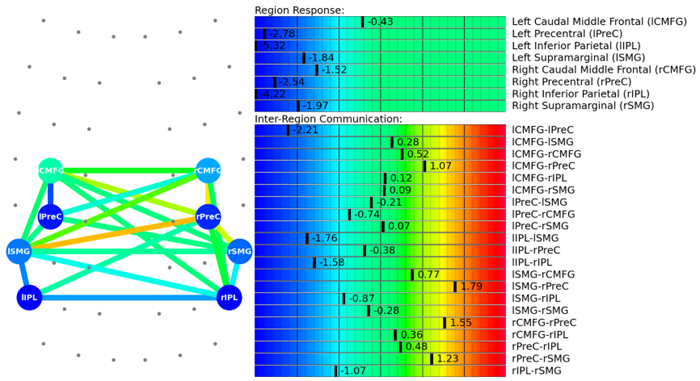
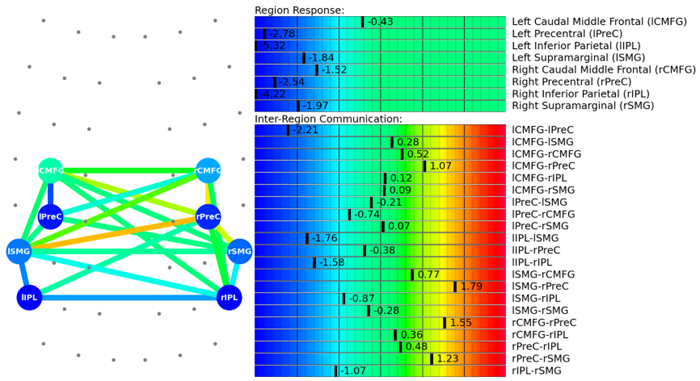
- A brain imaging scan called functional Neurocognitive Imaging (fNCI) to determine where and how the patient’s brain was affected by the injury.
The fNCI scan measures blood flow in 100 different regions of the brain while patients carry out a set of standardized cognitive tasks. It produces a series of real-time images that are combined and compared with scans from healthy people to identify the areas where NVC dysfunction is affecting normal brain function.
Regions are grouped according to function and then scored. Green scores show normal function, while yellow and red scores identify sections with neurovascular coupling dysfunction.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
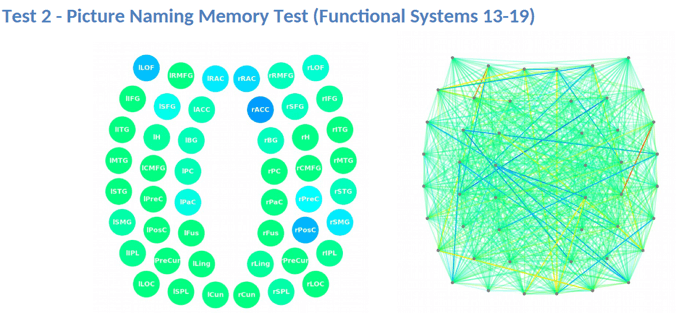
This information provides our staff with huge advantages when it comes to treating patients. For example, if we see visual systems such as target search, visual feature detection, or visual-spatial mapping aren’t working as they should, we can tailor exercises to work on those specific areas of the brain during therapy.
Sometimes, if we just assess vision on functional tasks, we may see that the patient performs very well. However, we often find on our fNCI that the brain regions and functional systems in charge of particular tasks are working very hard to do them, leading to fatigue and an increase in symptoms.
If we didn't have the lens of the fNCI, we would assess that skill as "normal", when in fact, a visual skill that we do repetitively all day long is coming at a large energy cost.
Finally, the fNCI allows us to see how visual systems are performing in context with the other key functional systems of the brain, enabling us to coordinate different types of therapies together.
After patients complete this evaluation, our team combines all the information and designs a customized treatment plan to target exactly the areas of the brain that show dysfunction for each patient.
During treatment week, patients go through an intense regime of aerobic exercise and a variety of different therapeutic interventions. Patients will receive most of the therapies listed below, but the exact combination of exercises within each therapy varies considerably, depending on the results of the brain scan.
|
Cognitive
therapy
|
- The aim is to engage key brain regions and rehabilitate cognitive skills, such as memory, attention, decision-making, and reasoning.
- Patients engage in cognitive activities, such as solving logic puzzles and identifying word patterns.
|
Occupational
therapy |
- Patients engage in exercises that help the brain, body, and eyes coordinate with each other.
- Therapists help patients readjust to their daily activities by focusing on difficulties identified on their fNCI scan, including compensatory strategies for work and school as they recover.
|
Neuromuscular
therapy |
- The aim is to relieve headaches and neck pain, rehabilitate balance, improve body-brain coordination, and promote physical activity.
- Patients receive massages, stretches, and soft tissue manipulation to increase blood flow.
- Patients engage in cognitive games and physical therapy exercises.
|
Sensorimotor
therapy |
- The aim is to improve cognitive and physical skills and reduce symptoms of depression.
- Patients follow simple movement patterns in time with a metronome to address cognitive, visual, and vestibular symptoms.
|
Visual skill &
processing
therapy |
- The aim is to address vision problems, such as blurred vision, difficulty focusing, and light sensitivity.
- Patients engage in different exercises, including Dynavision, visual tracking exercises, the Brock String, and some other computerized technologies.
- If patients need further therapy after treatment, our therapists can help find a suitable neuro-optometric rehabilitation program.
|
| Neuro integration therapy |
- The aim is to assess the visual, vestibular, and proprioceptive systems and their functions, and integrate them to improve patients’ ability to function in the world.
- Patients receive help with a variety of vestibular issues, including poor posture, dizziness, and vertigo. Vision exercises are often incorporated as well, such as saccades, near/far focusing, convergence/divergence, peripheral awareness, and hand/foot/eye coordination.
- Patients engage in gaze stabilization and balance exercises. For example, patients catch a ball while standing on a balance board or walk in a figure eight pattern while keeping their eyes focused on a point.
|
| Psychotherapy |
- Patients meet with a clinical psychologist to evaluate their mental health status.
- For patients suffering from depression and anxiety, our therapists recommend cognitive behavioral therapy (CBT). We do not offer this type of therapy but can refer them to a specialist.
- Patients learn mindfulness exercises and other relaxation strategies to improve their quality of life.
|
Almost all of our therapies include a visual component, though some focus on vision more heavily than others. Some examples include Dynavision and the Brock string.

Dynavision (shown above) is a computerized light board where patients push buttons as they light up in different patterns on the board. Sometimes, you’ll simply hit every button that lights up as quickly as you can after noticing it. Other times, you’ll need to exercise selective button-slamming skills by hitting only the red while avoiding the green.
Dynavision is great for oculomotor coordination and for activating several brain regions involved in movement, cognition, and vision.
For patients with visual perception issues, we also use the Brock string (shown below). This tool helps retrain the eyes to work together when you focus on beads located at different distances along the string.

In neurointegration therapy, you’ll perform exercises designed to help the brain, eyes, inner ear, and body to work together harmoniously.
The overall impact of these therapies working in combination is greater than if you were just pursuing one type of therapy at a time. When you activate the whole brain, positive changes tend to happen faster and in larger bursts because of the way the treatment works as a whole.
Sometimes, we’ll see patients who had been receiving vision therapy but who hit a plateau in treatment. When they come to Cognitive FX and have the neurovascular coupling component addressed, it’s much easier for their system to respond to vision therapy and resume improving.
That said, the eyes are slow to change and can take anywhere from six months to a year of vision therapy to recover fully. Treatment at Cognitive FX — whether EPIC 1 for one week, or EPIC 2 for two weeks — can provide a significant reduction in symptom burden and resolve many of the underlying issues, but there is no replacement for consistency in vision rehabilitation. We can give you a referral for a vision specialist in your hometown and teach you specific exercises to do at home.
A second follow-up fNCI at the end of the treatment allows our team to see how brain function is improving. 90% of our patients experience improvements during treatment, and most continue improving at home.
After your follow-up scan, a member of our team will analyze your results and give you some “homework.” Your homework will include some combination of aerobic exercise, cognitive games, and cognitive rest as you continue your recovery journey.
Ways to Cope with TBI Visual Symptoms at Home

As TBIs can cause so many different visual problems, each patient needs to find the best way to cope with their symptoms.
Some of the strategies we suggest include:
- Use technology to your advantage. Devices such as computers and mobile phones come with adjustable settings. This means you can make larger text or increase contrast. You can also rely on text-to-speech apps if you’re struggling to read a document.
- Use clocks and other devices at home with large text. You can also find phones with large buttons that are easy to see.
- At work, take frequent breaks, especially if your job relies heavily on your vision. This includes reading or using electronic devices. Follow the 20-20-20 rule: look away from what you’re doing every 20 minutes and focus on something at least 20 feet away for 20 seconds.
- Avoid bothersome light sources. Fluorescent lights can be irritating for some patients. As much as possible, rely on natural light.
- If you live alone and struggle to do your daily tasks, consider getting home help to help with household chores.
- If you’re experiencing dizziness, take things at a slower pace. For example, read slowly or take your time to focus on things more carefully than you did before your injury.
- Wearing tinted sunglasses both indoors and outdoors may help. Get help from a vision specialist to find the best color for you.
- Remove all clutter from your home and work. Designate one specific place for everyday items. For example, if you drop the car keys in the same place every day, it avoids having to look for them and reduces strain on the visual system.
- Don’t be afraid to ask for help. This can be from friends and family, as well as occasional encounters, such as someone standing at a bus stop with you or someone working in a supermarket.
- Learn some exercises for relieving eye strain from our YouTube video.
- Try our at-home headache management course: Our course on improving your headaches at home also includes a section on addressing vision-related issues. You may find that it provides much-needed relief as you wait for your treatment program to begin.
Note: If you’re experiencing symptoms (such as vision problems) that won’t resolve after a brain injury, you’re not alone. Our patients report, on average, a 60% improvement in symptoms after just one week of treatment. To see if you are eligible for treatment, sign up for a consultation.