A transient ischemic attack (TIA), often called a mini-stroke, occurs when blood flow to the brain is temporarily blocked. If a TIA affects areas responsible for vision — such as the eyes or the visual processing centers in the brain — it can cause sudden vision loss, double vision, or blurry vision. In some cases, this may be a medical emergency requiring immediate attention.
While TIA symptoms often resolve within hours, seeking urgent medical care is crucial. Although TIAs are not typically life-threatening, they serve as a warning sign, offering patients an opportunity to take preventive measures and reduce the risk of future strokes.
Most TIA-related vision issues are temporary, but some patients experience lingering symptoms. Additionally, vision problems are rarely the only complication — many patients also struggle with dizziness, brain fog, anxiety, and other cognitive or emotional challenges. Despite this, standard treatment often focuses on lifestyle changes and long-term medication to prevent a stroke, leaving some patients without effective solutions for ongoing symptoms.
At Cognitive FX, we take a different approach. Using advanced brain imaging techniques and a multidisciplinary treatment model, we address the full spectrum of TIA-related symptoms, rather than treating each issue in isolation. By tailoring therapy to each patient’s unique needs, we help them regain function and improve their quality of life more effectively than conventional methods alone.
In this article, we cover:
Note: If you’re experiencing symptoms (such as vision problems) that won’t resolve after a transient ischemic attack, you’re not alone. 95% of our patients experience statistically-verified restoration of brain function. To see if you’re eligible for treatment, sign up for a consultation.
Can TIAs Cause Vision Problems?
Yes, TIAs can affect vision. Studies estimate that 10% to 30% of TIA patients experience vision problems, which makes sense given the brain’s role in processing visual information. Patients may develop temporary eyesight issues if a TIA disrupts blood flow to the areas responsible for vision. In some cases, vision problems are the only symptom of a TIA, a condition known as ocular or retinal TIA.
Common Vision Symptoms of a TIA
During a TIA, the following vision issues may occur, though they typically resolve within a few hours:
- Blurry vision in one or both eyes
- Double vision in one or both eyes
- Temporary loss of vision in one or both eyes
- Difficulty with eye and eyelid movements
Other TIA symptoms include:
- Facial drooping (usually on one side)
- Weakness or numbness in an arm, leg, or one side of the body
- Mental confusion
- Speech difficulties, including slurred speech and trouble understanding others
- Difficulty walking
- Loss of balance and coordination
- Dizziness or vertigo
- Severe headache
- Difficulty swallowing
The best way to recognize if you are having a TIA is with the BE FAST acronym:
|
B
|
Balance
|
Are you dizzy? Have you fallen?
|
|
E
|
Eyesight
|
Have you lost your eyesight? Is your vision blurry?
|
|
|
|
|
|
F
|
Facial
|
Can you smile? Is your mouth drooping?
|
|
A
|
Arm
|
Can you raise both arms and keep them in that position? Do you have muscle tingling?
|
|
S
|
Speech
|
Can you speak clearly? Is your speech slurred?
|
|
T
|
Time
|
Seek immediate medical assistance if you have any of these signs.
|
The Most Common Vision Problem After a TIA: Transient Monocular Vision Loss (TMVL)
When TIAs interrupt blood supply to the eyes, they can cause transient monocular vision loss (TMVL) — a temporary, sudden loss of vision in one eye. This condition, also known as amaurosis fugax (Latin for “dark fleeting”), is the most common TIA-related vision problem, affecting about one-third of patients who experience visual symptoms.
TMVL is caused when blood circulation is blocked in the retina or, less commonly, the optic nerve. Patients typically experience:
- Cloudy or blurred vision
- Partial or complete vision loss, usually in one eye (but rarely in both)
Many patients describe TMVL as if a dark curtain is being pulled over their eye, with vision gradually fading from top to bottom or from the periphery to the center. The vision loss is temporary and usually lasts from a few seconds to several minutes.
Recovery follows the same pattern as the initial loss — patients often feel like the "curtain" is lifting or that their vision is clearing like fog. However, vision typically returns slower than it was lost.
Other Vision Issues That Can Occur After a TIA
In addition to transient monocular vision loss (TMVL), TIAs can cause other vision-related problems, including:
Homonymous Hemianopia (Partial Vision Loss in Both Eyes)
Approximately 12% of TIA patients with vision problems experience homonymous hemianopia, a condition that affects the same side of the visual field in both eyes. Patients lose sight on either the right or left side of their visual field — meaning in right homonymous hemianopia, the right side of vision is lost in both eyes.
This condition typically occurs when a TIA affects the brain’s temporal, parietal, or occipital lobe. Patients may:
- Run into objects, trip, or fall
- Knock things over
- Lose their place while reading
- Be startled by people or objects appearing from their blind spot
Diplopia (Double Vision)
About 13% of TIA patients experience diplopia, or double vision, when the TIA affects the nerves controlling eye movement. This occurs when the eyes can’t move together properly, making it difficult to maintain focus. Instead of seeing two distinct images, some patients report overlapping or blurred vision.
Diplopia may be constant or position-dependent, meaning it occurs only when looking in certain directions (e.g., left, right, up, or down). It is commonly linked to TIA effects on the brainstem or cerebellum, areas responsible for coordinating eye movements.
Bilateral Vision Loss (Lone Bilateral Blindness)
This rare condition affects about 4% of TIA patients with vision problems, causing temporary loss of vision in both eyes simultaneously. Some patients experience total blindness, while others describe it as blurry vision or “looking through a veil.”
Bilateral vision loss may also be accompanied by:
- Double vision
- Vertigo
- Other neurological symptoms
Notably, this symptom is associated with a higher risk of stroke, making preventative care essential for affected patients.
Bilateral Positive Visual Phenomena
Some TIA patients experience false visual images, known as positive visual phenomena. These occur when the brain misinterprets visual input, leading to distorted images or hallucinations. Patients may see:
- Flashing lights
- Zigzag lines
- Scintillations (sparkling or flickering lights)
- Distorted or hallucinated objects
In most cases, these symptoms last from a few moments to several hours.
Spatial Inattention (Visual Neglect)
If a TIA affects the brain’s visual processing centers, patients may struggle to interpret what they see, a condition known as visual neglect or spatial inattention.
Patients with this condition may:
- Ignore food on one side of their plate
- Avoid shaving or applying makeup on one side of their face
- Fail to notice objects or people on their affected side, causing them to bump into things frequently
Interestingly, patients are often unaware of their deficit because their brain doesn’t recognize that anything is missing.
Sensitivity to Light (Photophobia)
Between 5-10% of TIA patients with vision issues report light sensitivity, where bright lights feel uncomfortable, and adjusting to different lighting conditions becomes difficult. Many also experience:
- Headaches triggered by light exposure
- Eye pain or discomfort when looking at certain visual stimuli
Dry Eye Syndrome (Keratoconjunctivitis Sicca)
Dry eyes after a TIA can occur due to nerve or muscle dysfunction affecting the eyelids. If patients struggle to blink or fully close their eyes, tear evaporation increases, leading to:
- A burning or gritty sensation in the eyes
- Itchy, irritated eyes
How Do TIAs Cause Vision Problems?
TIAs can cause vision problems in multiple ways, affecting visual processing areas, blood flow regulation, autonomic nervous system function, sensory integration, and even as a side effect of medication.
1. Direct Damage to Visual Processing Areas
When a TIA disrupts blood flow, it can directly affect brain regions responsible for vision, leading to temporary or lasting symptoms. These areas include:
-
The Eyes – Capture and process light, converting it into neural signals.
-
The Optic Nerve – Transmits visual information from the retina to the brain.
-
The Visual Cortex (Occipital Lobe) – The brain’s primary vision center, responsible for processing visual information.
-
The Parietal Lobe – Helps with spatial awareness and depth perception.
-
The Temporal Lobe – Stores and processes visual memories.
Damage or disruption in any of these areas can result in blurred vision, double vision, partial vision loss, or difficulties recognizing objects and spatial relationships.
2. Neurovascular Coupling (NVC) Disruption
TIAs also impact vision by disrupting the brain’s ability to regulate blood flow.
Normally, brain cells signal nearby blood vessels to deliver oxygen and nutrients as needed. However, during a TIA, blood flow is temporarily restricted or blocked, depriving brain cells of essential resources. Even after circulation resumes, the connection between neurons and blood vessels — known as neurovascular coupling (NVC ) — can remain impaired.
This disruption may:
-
Weaken affected brain areas, making it harder to process visual information.
-
Lead to microscopic cell death, especially in deeper brain regions with small blood vessels.
-
Cause long-term visual disturbances, even after the TIA resolves.
Clusters of damaged brain cells may appear as tiny white spots on MRI scans, often labeled as “nonspecific findings.” While not immediately life-threatening, these areas once played critical roles in brain function, including vision.

3. Dysfunction of the Autonomic Nervous System (ANS)
TIAs can also interfere with the Autonomic Nervous System (ANS), which regulates involuntary functions like pupil size, eye focus, heart rate, and blood pressure.
The ANS has two main branches:
After a TIA, the SNS can become overactive, keeping the body in a state of heightened alert even when there’s no danger. This can:
-
Disrupt eye focus, making it difficult to adjust to different distances.
-
Alter pupil reactions, leading to light sensitivity or difficulty adapting to brightness changes.
This imbalance can contribute to many of the vision symptoms associated with TIAs.
4. Mismatched Sensory Signaling
For clear vision, the brain must integrate input from three sources:
-
The Eyes (visual data)
-
The Vestibular System (balance and motion)
-
Proprioception (the body's sense of movement and position)
After a TIA, these signals can become mismatched, forcing the brain to work harder to interpret its surroundings. This can cause:
- Blurry or unstable vision
- Balance problems
- Dizziness or vertigo
Even simple tasks like walking or reading can feel disorienting when these systems are out of sync.
5. Medication Side Effects
Some medications commonly prescribed after a TIA can also cause vision problems by affecting the retina, optic nerve, or other eye structures.
Medications that may impact vision include:
-
NSAIDs (e.g., ibuprofen, aspirin) – May cause dry eyes, redness, and light sensitivity.
-
Antidepressants – Can lead to increased eye pressure, blurred vision, dry eyes, or double vision.
-
Antihistamines – May cause dry, itchy, or burning eyes, along with blurred vision or excessive tearing.
-
High Blood Pressure Medications – Can contribute to dry and irritated eyes.
Patients experiencing persistent or worsening vision problems should discuss medication side effects with their doctor.
Prognosis: How Do Vision Symptoms Affect Patient Outcomes?
With proper medical care, patients whose TIA symptoms primarily involve vision tend to have a better overall prognosis than those with other TIA symptoms. They are:
One possible explanation is that the retina is more sensitive than brain tissue, meaning even small blockages can cause noticeable vision symptoms. In contrast, similar blockages in other brain regions may not immediately trigger symptoms. In practical terms, this means vision-related TIAs serve as an earlier warning, prompting some patients to seek medical attention sooner than those without visual disturbances.
Despite being included in the BE FAST acronym for stroke and TIA recognition, patients and medical professionals often overlook vision symptoms. Because symptoms are brief and mild, many people fail to recognize they’ve had a TIA and don’t seek medical help. This delay can be dangerous, as even a mild TIA significantly increases stroke risk.
Seeking prompt medical care is critical — even if vision issues are the only symptom — as early intervention can prevent a more severe stroke.
How Are TIA-Related Vision Symptoms Treated?
If you experience a sudden loss of vision, seek medical care immediately, even if your symptoms resolve within minutes. Undergoing an eye examination is still very important, as diagnostic clues can sometimes help your doctor narrow down the possible causes. In some cases, blood tests may also be required to assess risk factors and guide treatment decisions.
Treatment for TIA-related vision symptoms focuses on rehabilitation, prevention, and lifestyle changes to reduce the risk of future TIAs or strokes.
Vision Therapy (Neuro-Optometric Vision Rehabilitation)
Vision therapy can be beneficial for patients who experience lingering vision symptoms. This structured approach to rehabilitation uses targeted exercises to improve visual function and processing skills.
Key benefits of vision therapy include:
-
Improving visual acuity: Vision therapy can strengthen eye muscles, coordination, and eye-teaming abilities. One effective exercise is the Brock String, which involves focusing on beads along a string to enhance depth perception and focus at different distances.
-
Enhancing visual processing skills: Some TIA patients struggle with interpreting visual information. Exercises targeting visual memory, discrimination, and closure help improve how the brain processes images. A common technique involves using colored lights to stimulate the visual system.
-
Addressing visual field deficits: Patients with hemianopia or other visual field issues can learn compensatory strategies to navigate their environment more effectively. Training often focuses on enhancing peripheral awareness and developing systematic scanning techniques.
-
Reducing visual discomfort: TIA patients often experience eye strain, headaches, or light sensitivity. Vision therapy teaches relaxation techniques and strategies to reduce eye fatigue, such as adjusting focus between near and far objects.
-
Improving quality of life: By restoring visual skills, vision therapy helps TIA patients resume daily activities such as reading, driving, and socializing with greater ease and confidence.
Preventative Measures
Since TIA patients face an increased risk of future TIAs or strokes, doctors often recommend a combination of medication and lifestyle changes (and in some cases surgery) to reduce this risk.
Medication for Stroke Prevention
Most patients who experience an ischemic stroke or TIA will need medication to reduce the risk of another TIA or a more serious stroke. Examples include:
-
Antiplatelets, such as aspirin, clopidogrel, and ticagrelor, are blood thinners commonly used for many TIA patients to lower the risk of a future stroke.
-
Anticoagulants, such as warfarin and dabigatran, to help prevent the formation of blood clots.
-
Hypertensive medication for patients with high blood pressure (hypertension).
-
Lipid-lowering medication for patients with cardiovascular problems.
-
Medication to control cholesterol, such as statins, to reduce high cholesterol.
Lifestyle Changes
Patients can significantly reduce their risk of a stroke by making healthy lifestyle changes, including:
-
Quitting smoking: Continuing to smoke after a TIA doubles the risk of another TIA or stroke and increases mortality rates. Giving up is not easy, but it’s one of the best things patients can do to help reduce the risk of another stroke. The risk starts to decrease as soon as patients quit, and within a few years, the risk is similar to that of a non-smoker.
-
Staying physically active: Regular exercise improves circulation, lowers blood pressure, stabilizes blood sugar, and reduces cholesterol. The recommended guideline per week is:
-
150 minutes of moderate-intensity exercise (e.g., brisk walking, cycling) OR
-
75 minutes of vigorous exercise (e.g., running, swimming, uphill biking)
-
Limiting alcohol intake: Excessive alcohol consumption raises blood pressure, triggers atrial fibrillation, and increases the risk of stroke. TIA patients taking medication should consult a doctor about safe alcohol consumption.
-
Eating a healthy diet: Eating a diet high in fat and processed foods increases the risk of a stroke. Patients should follow a balanced diet with at least five portions of fruits and vegetables every day. Fruit and vegetables contain a range of vitamins, minerals, fiber, and antioxidants such as vitamins A, C, and E and beta-carotene, which help reduce the risk of stroke.
-
Maintain a healthy weight: Obesity increases the risk of high blood pressure, cardiovascular disease/heart disease, and type 2 diabetes, which in turn increases your risk of a stroke. Losing as little as 5% to 10% of body weight can significantly reduce stroke risk. Sustainable changes in diet and exercise are key to long-term weight management.
Surgical Interventions
For some patients, the following surgical procedures may be recommended to improve blood flow and prevent strokes:
-
Carotid Endarterectomy: Removes fatty deposits from the carotid arteries.
-
Angioplasty & Stenting: Uses a balloon-like device to open clogged arteries, with a stent to keep them open.
How We Treat Lingering TIA Symptoms (Including Vision Problems) at Cognitive FX
As we’ve discussed, while most patients recover from TIAs within days, some experience persistent issues that require more comprehensive rehabilitation.
At Cognitive FX, we specialize in treating the underlying brain dysfunction that can occur as a result of TIAs and other brain injuries. We help patients recover from long-term TIA effects using advanced imaging and personalized therapies, improving function and quality of life.
Treatment Overview
Before treatment begins, every patient undergoes a comprehensive vision assessment, even if they haven’t reported visual issues. This includes:
-
Saccades – Evaluating eye movement accuracy when shifting focus between points.
-
Convergence/Divergence – Assessing how the eyes work together for depth perception.
-
Peripheral Vision – Measuring awareness of objects at the edges of the visual field.
-
Visual Processing – Testing reaction time and coordination in real-world scenarios (e.g., recognizing and responding to a changing traffic light).
-
RightEye Exam – Using eye-tracking software to analyze muscle function and movement precision.
We assess these skills from both a functional and neurological perspective, examining not just performance but also the underlying brain regions and nerves responsible for vision. This ensures targeted rehabilitation when needed.
However, vision is just one part of our comprehensive evaluation before designing a treatment plan. We also conduct:
-
Medical Review – A doctor reviews personal medical history, family history, symptoms, and concerns.
-
Physical Exam – Checking balance, coordination, reaction time, and motor skills.
-
Neurocognitive Test – Assessing memory, focus, and reasoning abilities.
-
Psychological Evaluation – Identifying anxiety, depression, or other mental health concerns.
-
MRI Scan – Magnetic resonance imaging examining brain and cervical spine structure for underlying injuries.
-
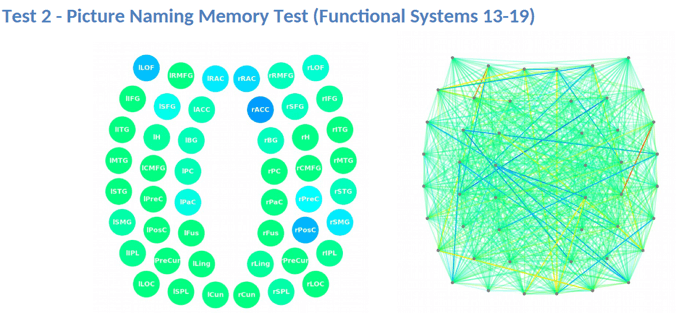
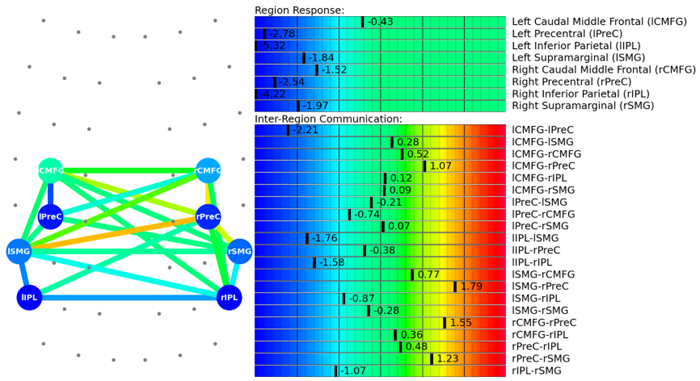
Functional Neurocognitive Imaging (fNCI) Scan – Measuring blood flow in 100 brain regions during standardized cognitive tasks to pinpoint neurovascular dysfunction.
Regions are grouped according to function and then scored. Green scores show normal function, while yellow and red scores identify sections with neurovascular coupling dysfunction.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while areas in varying shades of blue are less active than normal.
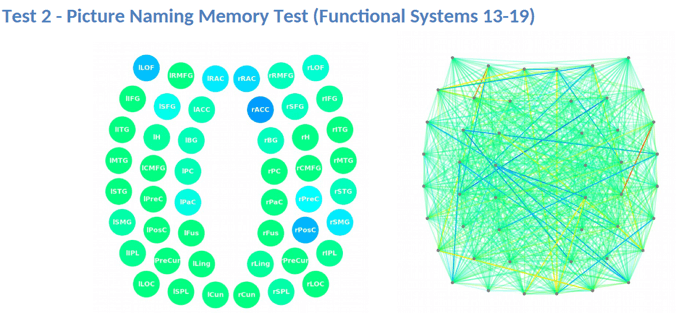
This information provides our staff with huge advantages when it comes to treating patients. For example, if we see visual systems such as target search, visual feature detection, or visual-spatial mapping aren’t working as they should, we can tailor exercises to work on those specific areas of the brain during therapy.
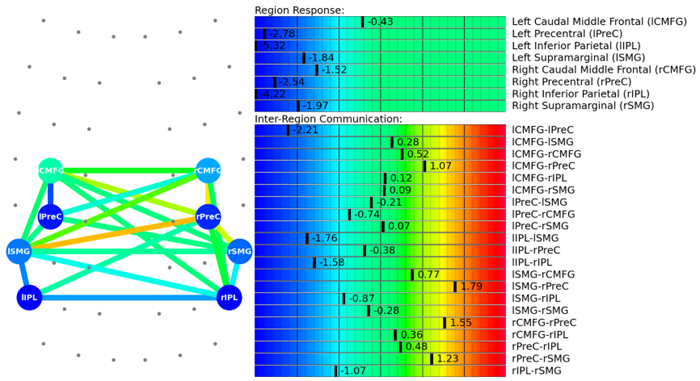
Sometimes, patients perform well on standard tests, yet fNCI reveals that key brain regions are overworking, leading to fatigue and symptom flare-ups. Without this insight, we might assess a skill as “normal,” when in reality, a routine visual task is draining excessive energy.
fNCI also helps us understand how visual systems interact with other brain functions, allowing us to coordinate therapies more effectively. After evaluation, our team analyzes the data and designs a personalized treatment plan to target each patient’s specific dysfunctions.
During treatment week, patients undergo a rigorous regimen of aerobic exercise and tailored therapeutic interventions. While most will receive multiple therapies, the exact approach is customized based on their brain scan results.
|
Cognitive
therapy
|
-
The aim is to engage key brain regions and rehabilitate cognitive skills, such as memory, attention, decision-making, and reasoning.
-
Patients engage in cognitive activities, such as solving logic puzzles and identifying word patterns.
|
|
Occupational
therapy
|
-
Patients engage in exercises that help the brain, body, and eyes coordinate with each other.
-
Therapists help patients readjust to their daily activities by focusing on difficulties identified on their fNCI scan, including compensatory strategies for work and school as they recover.
|
|
Neuromuscular
therapy
|
-
The aim is to relieve headaches and neck pain, rehabilitate balance, improve body-brain coordination, and promote physical activity.
-
Patients receive massages, stretches, and soft tissue manipulation to increase blood flow.
-
Patients engage in cognitive games and physical therapy exercises.
|
|
Sensorimotor
therapy
|
-
The aim is to improve cognitive and physical skills and reduce symptoms of depression.
-
Patients follow simple movement patterns in time with a metronome to address cognitive, visual, and vestibular symptoms.
|
|
Visual skill &
processing
therapy
|
-
The aim is to address vision problems, such as blurred vision, difficulty focusing, and light sensitivity.
-
Patients engage in different exercises, including Dynavision, visual tracking exercises, the Brock String, and other computerized technologies.
-
If patients need further therapy after treatment, our therapists can help find a suitable neuro-optometric rehabilitation program.
|
|
Neurointegration
therapy
|
-
The aim is to assess the visual, vestibular, and proprioceptive systems and their functions, and integrate them to improve patients’ ability to function in the world.
-
Patients receive help with various vestibular issues, including poor posture, dizziness, and vertigo. Vision exercises such as saccades, near/far focusing, convergence/divergence, peripheral awareness, and hand/foot/eye coordination are also often incorporated.
-
Patients engage in gaze stabilization and balance exercises. For example, patients catch a ball while standing on a balance board or walk in a figure eight pattern while keeping their eyes focused on a point.
|
|
Psychotherapy
|
-
Patients meet with a clinical psychologist to evaluate their mental health status.
-
For patients suffering from depression and anxiety, our therapists recommend cognitive behavioral therapy (CBT). We do not offer this type of therapy, but we can refer them to a specialist.
-
Patients learn mindfulness exercises and other relaxation strategies to improve their quality of life.
|
Nearly all of our therapies incorporate a visual component, though some focus more heavily on vision than others. Key examples include:
-
Dynavision – A computerized light board that enhances oculomotor coordination, cognitive processing, and reaction time by requiring patients to hit buttons as they light up in various patterns.
-
Brock String – Helps retrain the eyes to work together by focusing on beads at different distances, improving depth perception and eye coordination.
-
Neurointegration Therapy – Exercises designed to synchronize the brain, eyes, inner ear, and body, enhancing overall sensory processing.
Engaging multiple brain systems accelerates recovery more effectively than isolated therapy. However, vision changes happen gradually and may require six months to a year of rehabilitation. While treatment at Cognitive FX significantly reduces symptoms, some patients benefit from ongoing vision therapy. We provide referrals and at-home exercises to support continued progress.
A follow-up fNCI scan at the end of treatment measures improvements in brain function. 90% of our patients show progress, and most continue improving at home. After the scan, a team member reviews your results and assigns “homework,” including aerobic exercise, vision exercises, cognitive games, and structured rest to support long-term recovery.
Schedule a consultation with our team to determine if our program is right for you.






.png?height=175&name=Vision%20Problems%20After%20COVID%20Causes%20and%20Treatment%20(1).png)



