Eye twitching is typically mild and short-lived, but for some patients with post-concussion syndrome (PCS), it can become a persistent and uncomfortable symptom. While often overlooked, eye twitching after a head injury may be a sign of cranial nerve or brainstem dysfunction.
Unfortunately, conventional treatments tend to focus only on managing the symptom rather than addressing its neurological root cause. At Cognitive FX, we take a different approach — using functional brain imaging and targeted therapies to retrain the brain and cranial nerves involved in eye control.
In this article, we’ll cover:
Note: If you’re experiencing symptoms (such as vision problems) that won’t resolve after a traumatic brain injury, you’re not alone. 95% of our patients experience statistically verified restoration of brain function. To see if you are eligible for treatment, sign up for a consultation.
What Does Eye Twitching Feel Like After a Brain Injury?
Eye twitching — an involuntary spasm of the eyelid muscles — isn’t among the most common post-concussion symptoms, but it does affect some patients. It usually impacts the upper eyelid and feels like a fluttering or gentle tug, as if someone is lightly pulling at the lid.
The twitching may last only a few seconds but recur many times throughout the day. It can happen every few seconds or much less frequently — the pattern is often unpredictable. In most cases, it’s painless and mild. But in more severe cases, it can involve forceful eyelid closure lasting for minutes or longer.
Patients may also experience additional visual symptoms, including:
- Eye irritation/eye pain
- Increased blinking
- Light sensitivity (photophobia)
- Dry eyes
- Blurred vision
- Double vision
- Facial muscle spasms
What Causes Eye Twitching After a Concussion?
Eye twitching after a traumatic brain injury (TBI) can have several neurological causes. Some involve direct damage to nerves or muscles, while others stem from more generalized brain dysfunction.
Cranial Nerve Damage
Several cranial nerves play a role in eyelid and eye muscle control. Damage to any of the following may result in twitching or spasms:
-
Cranial Nerve VII (Facial Nerve): Damage to this nerve may trigger the muscle responsible for closing the eyelids to malfunction, which in turn can cause eye twitching.
-
Cranial Nerve III (Oculomotor Nerve): This controls eye movement. Damage can lead to twitching, eyelid drooping, eye misalignment, or double vision.
-
Cranial Nerve V (Trigeminal Nerve): This cranial nerve regulates some of the facial muscles around the eyes. Damage may result in involuntary twitching, spasms, or even forced closure of the eyelid.
Damage to Brain Regions That Control Cranial Nerves
Even if the nerves themselves are intact, damage to the brainstem, thalamus, or basal ganglia — areas of the brain responsible for processing input from cranial nerves — can disrupt communication and lead to eye twitching.
Ocular Muscle Spasms
In some cases, the muscles directly responsible for eye and eyelid movement become irritated or overworked, especially the extraocular muscles and ciliary muscles (involved in focusing). Dysfunction here can contribute to light sensitivity, eye strain, twitching, or problems focusing and tracking objects.
Fatigue and Sleep Disruption
Even without direct nerve or muscle damage, eye twitching can result from fatigue or poor sleep — both common symptoms after a concussion. When the brain is exhausted, it becomes harder to regulate muscle activity, including the tiny muscles around the eyes.
Conventional Treatments vs. Neurological Rehab
Standard treatments for vision problems after a mild traumatic brain injury typically aim to manage symptoms rather than resolve the root cause. These approaches may include:
-
Warm compresses to relax the eyelid muscles
-
Lifestyle changes, like reducing caffeine, alcohol, or screen time
-
Botulinum (Botox) injections to temporarily paralyze the twitching muscle (requires ongoing treatment and may cause side effects like drooping or dry eyes)
-
Medications, such as muscle relaxants or anticonvulsants
-
Surgery (e.g., myectomy) in severe, rare cases
-
Vision therapy (best conventional option), which may help train eye movement and focus, but isn’t typically designed for brain-injury-related eye problems
While these treatments may provide temporary relief, they don’t address the underlying neurological dysfunction — especially when the cause is rooted in post-concussion brain changes.
How Cognitive FX Treats Eye Twitching After Brain Injury
At Cognitive FX, we provide personalized treatment for individuals suffering from lingering symptoms after brain injury. We help patients with physical symptoms (e.g. headaches, brain fog, balance problems, vision problems), cognitive symptoms (e.g. memory and concentration difficulties), and emotional symptoms (e.g. depression, anxiety, etc.).
When it comes to eye twitching, our goal is to identify which cranial nerves and brain regions may be affected and then retrain those systems through functional rehabilitation.
Cranial Nerve Retraining
We use specific exercises to activate and restore function in the nerves responsible for eyelid control. For example:
-
Cranial Nerve Neuromechanics — Our proprietary, precise method of tensioning and mobilizing specific cranial nerves to improve their connectivity and mobility within the brainstem and skull.
-
Eye-opening and closing drills retrain the brain and facial muscles to work together properly.
-
Sensory exercises target nerve input around the eye to improve feedback and control.
These therapies are grounded in functional neurology and draw on methods from advanced training systems like Z-Health. Most clinics don’t offer this level of cranial nerve rehabilitation.
Full-Brain Healing
Instead of treating visual symptoms in isolation, our treatment — called Enhanced Performance in Cognition (EPIC) — is an intense, individualized program designed to treat each patient’s specific symptoms, including vision problems.
Before treatment begins, we perform a thorough vision assessment as part of our evaluation process. Our visual exam includes:
-
Saccades: Testing the patient's ability to accurately move the eyes from one designated focal point to another in a single, quick movement.
-
Convergence/Divergence: Testing how a patient’s eyes rotate inward (converge) and outward (diverge) as an object moves closer or farther away, helping to assess depth perception.
-
Peripheral vision: Testing the patient’s awareness and ability to see the edges of their visual field without moving their head.
-
Visual processing: Testing the patient’s ability to “See, Process, and Respond” in different situations. For example, following a coordination chart where one prompt is a cue for the right hand, another for the left, and another for both. We assess how accurately and quickly a patient can complete this task. (In daily life, this would relate to seeing a traffic light turn yellow and then red. Do you see the light change and react appropriately and in time?)
-
RightEye exam: Eye-tracking software that assesses subtleties of how a patient’s eyes are moving, which eye muscles are working properly, and which aren’t.
Importantly, we assess each of these skills from a functional and a neurological perspective. In addition to looking at the specific function itself, and how well the patient is performing it, we also look at the nerves and brain regions responsible for these tasks. This allows us to most effectively rehabilitate these skills.
However, vision is just one of several physical and cognitive systems that we assess before developing a treatment protocol. Our evaluation also includes:
-
A meeting with one of our doctors to review the patient’s medical history and symptoms.
-
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
-
A neurocognitive test to assess memory, concentration, reasoning, and other cognitive functions.
-
A psychological evaluation to identify symptoms of anxiety, depression, and other mental health problems.
-
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
-
A brain imaging scan called functional Neurocognitive Imaging (fNCI) to determine where and how the patient’s brain was affected by the injury.
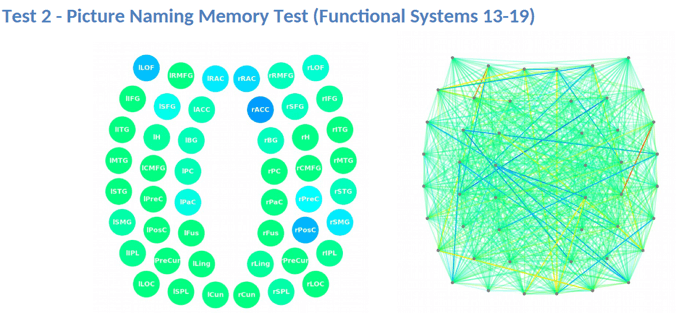
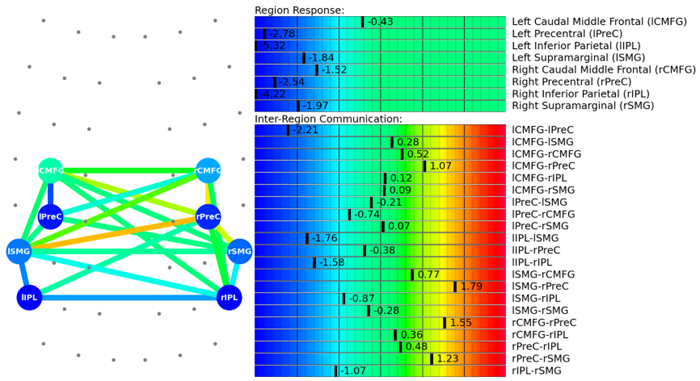
The fNCI scan measures blood flow in 100 different regions of the brain while patients carry out a set of standardized cognitive tasks. It produces a series of real-time images that are combined and compared with scans from healthy people to identify the areas where neurovascular coupling disruption is affecting normal brain function.
Regions are grouped according to function and then scored. Green scores show normal function, while yellow and red scores identify sections with neurovascular coupling dysregulation.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
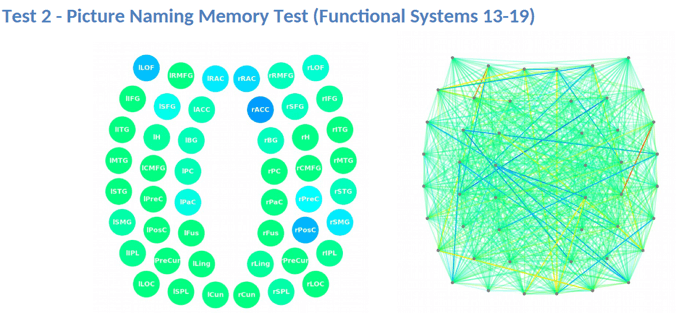
This information provides our staff with huge advantages when it comes to treating patients. For example, if we see visual systems such as target search, visual feature detection, or visual-spatial mapping aren’t working as they should, we can tailor exercises to work on those specific areas of the brain during therapy.
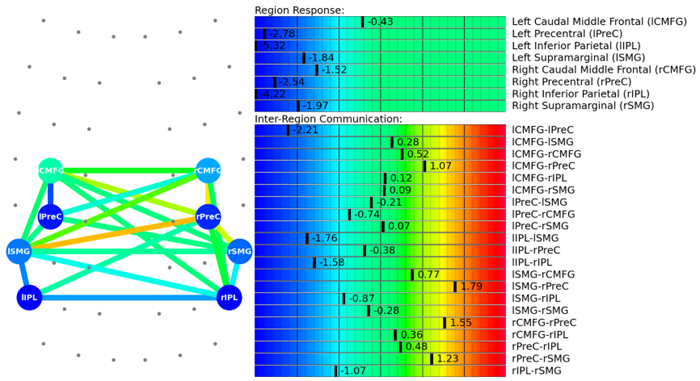
Sometimes, if we just assess vision on functional tasks, we may see that the patient performs very well. However, we often find on our fNCI that the brain regions and functional systems in charge of particular tasks are working very hard to do them, leading to fatigue and an increase in symptoms.
If we didn't have the lens of the fNCI, we would assess that skill as "normal", when in fact, a visual skill that we do repetitively all day long is coming at a large energy cost.
Finally, the fNCI allows us to see how visual systems are performing in context with the other key functional systems of the brain, enabling us to coordinate different types of therapies together.
After patients complete this evaluation, our team combines all the information and designs a customized treatment plan to target exactly the areas of the brain that show dysfunction for each patient.
During treatment week, patients go through an intense regimen of aerobic exercise and a variety of different therapeutic interventions. Patients will receive most of the therapies listed below, but the exact combination of exercises within each therapy varies considerably, depending on the results of the brain scan.
|
Cognitive
therapy
|
-
The aim is to engage key brain regions and rehabilitate cognitive skills, such as memory, attention, decision-making, and reasoning.
-
Patients engage in cognitive activities, such as solving logic puzzles and identifying word patterns.
|
|
Occupational
therapy
|
-
Patients engage in exercises that help the brain, body, and eyes coordinate with each other.
-
Therapists help patients readjust to their daily activities by focusing on difficulties identified on their fNCI scan, including compensatory strategies for work and school as they recover.
|
|
Neuromuscular
therapy
|
-
The aim is to relieve headaches and neck pain, rehabilitate balance, improve body-brain coordination, and promote physical activity.
-
Patients receive massages, stretches, and soft tissue manipulation to increase blood flow.
-
Patients engage in cognitive games and physical therapy exercises.
|
|
Sensorimotor
therapy
|
-
The aim is to improve cognitive and physical skills and reduce symptoms of depression.
-
Patients follow simple movement patterns in time with a metronome to address cognitive, visual, and vestibular symptoms.
|
|
Visual skill &
processing
therapy
|
-
The aim is to address vision problems, such as blurred vision, difficulty focusing, and light sensitivity.
-
Patients engage in different exercises, including Dynavision, visual tracking exercises, the Brock String, and some other computerized technologies.
-
If patients need further therapy after treatment, our therapists can help find a suitable neuro-optometric rehabilitation program.
|
|
Neuro-integration
therapy
|
-
The aim is to assess the visual, vestibular, and proprioceptive systems and their functions, and integrate them to improve patients’ ability to function in the world.
-
Patients receive help with a variety of vestibular issues, including poor posture, dizziness, and vertigo. Vision exercises are often incorporated as well, such as saccades, near/far focusing, convergence/divergence, peripheral awareness, and hand/foot/eye coordination.
-
Patients engage in gaze stabilization and balance exercises. For example, patients catch a ball while standing on a balance board or walk in a figure eight pattern while keeping their eyes focused on a point.
|
|
Psychotherapy
|
-
Patients meet with a clinical psychologist to evaluate their mental health status.
-
For patients suffering from depression and anxiety, our therapists recommend cognitive behavioral therapy (CBT). We do not offer this type of therapy but can refer them to a specialist.
-
Patients learn mindfulness exercises and other relaxation strategies to improve their quality of life.
|
Almost all of our therapies include a visual component, though some focus on vision more heavily than others. Some examples include Dynavision and the Brock string.

Dynavision (shown above) is a computerized light board where patients push buttons as they light up in different patterns on the board. Sometimes, you’ll simply hit every button that lights up as quickly as you can after noticing it. Other times, you’ll need to exercise selective button-slamming skills by hitting only the red while avoiding the green.
Dynavision is great for oculomotor coordination and for activating several brain regions involved in movement, cognition, and vision.
For patients with visual perception issues, we also use the Brock string (shown below). This tool helps retrain the eyes to work together when you focus on beads located at different distances along the string.

In neurointegration therapy, you’ll perform exercises designed to help the brain, eyes, inner ear, and body work together harmoniously.
The overall impact of these therapies working in combination is greater than if you were just pursuing one type of therapy at a time. When you activate the whole brain, positive changes tend to happen faster and in larger bursts because of the way the treatment works as a whole.
Sometimes, we’ll see patients who have been receiving vision therapy but who hit a plateau in treatment. When they come to Cognitive FX and have the neurovascular coupling component addressed, it’s much easier for their system to respond to vision therapy and resume improving.
That said, the eyes are slow to change and can take anywhere from six months to a year of vision therapy to recover fully. Treatment at Cognitive FX — whether EPIC 1 for one week, or EPIC 2 for two weeks — can provide a significant reduction in symptom burden and resolve many of the underlying issues, but there is no replacement for consistency in vision rehabilitation. We can give you a referral for a vision specialist in your hometown and teach you specific exercises to do at home.
A second follow-up fNCI at the end of the treatment allows our team to see how brain function is improving. 90% of our patients experience improvements during treatment, and most continue improving at home.
After your follow-up scan, a member of our team will analyze your results and give you some “homework.” Your homework will include some combination of aerobic exercise, cognitive games, and cognitive rest as you continue your recovery journey.
Tips for Managing Eye Twitching at Home
For mild symptoms, the following self-care strategies may offer relief:
- Get enough sleep
- Reduce caffeine and alcohol intake
- Use artificial tears to relieve eye dryness
- Limit screen time and take frequent breaks
- Practice stress reduction techniques (breathing exercises, meditation, light physical activity)
- Wear sunglasses in bright environments
You Don’t Have to Live With It Forever
Eye twitching may seem minor compared to other post-concussion symptoms, but it can still disrupt your comfort and daily life — especially when it’s part of a larger pattern of symptoms resulting from dysfunction. Fortunately, help is available.
At Cognitive FX, we specialize in identifying the root causes of lingering brain injury symptoms and helping patients retrain their brains for lasting recovery — eye twitching included.
If you’re experiencing symptoms (such as vision problems) that won’t resolve after a traumatic brain injury, you’re not alone. 95% of our patients experience statistically verified restoration of brain function. To see if you are eligible for treatment, sign up for a consultation.