How to Tackle Post Traumatic Brain Injury Syndrome
“Post-traumatic brain injury syndrome” refers to long-term repercussions from concussions and other head injuries. Someone using this term could be referring to one of three conditions:
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Recovering from a traumatic brain injury (TBI) often means dealing with physical symptoms, such as headaches, balance issues, weak muscles, and vision problems. These symptoms can affect every aspect of life, making even simple tasks difficult.
Physical therapy can help you regain some of the abilities you lost due to the brain injury and speed up your overall recovery. Tailored exercises can help address neurologic problems, improve coordination and balance, address vision issues, relax neck and head muscles, and help you overcome exercise intolerance.
With that said, TBIs cause more than just physical symptoms. For example, patients also experience cognitive symptoms such as brain fog, difficulty concentrating and problem-solving, as well as emotional symptoms such as increased anxiety or depression.
As such, treating TBIs effectively requires a more comprehensive plan of care — involving physical therapy alongside a variety of other types of therapy (such as cognitive therapy, speech therapy, occupational therapy, and others) to address your symptoms holistically.
As much as physical therapy can alleviate and treat some symptoms and neurological conditions, it should not be the sole type of therapy treating brain injuries.
In this article, we’ll cover:
If you've experienced one or more head injuries and your symptoms persist, you're not alone and you're not imagining it. Help is available. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-head injury symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. Schedule a consultation to see if you’re eligible for treatment.
People typically think of seeing a physical therapist for rehabilitation after an acute injury, such as an ACL tear or a bone fracture, but physical therapy can also help patients after a head injury.
In recent years, there’s been more awareness and acceptance of the benefits of physical therapy in treating inpatients and outpatients with TBIs (including mild traumatic brain injuries), especially when physical therapists are part of a multidisciplinary treatment team. In 2017, the American Physical Therapy Association wrote about growing research to support the benefits of using physical therapy in concussion management (Beyond Rest: Physical Therapists and Concussion Management).
Physical therapists offer various interventions and treatments for brain injury rehabilitation, including exercises that help with specific symptoms, as we’ll discuss later in this article. These specialized healthcare providers also teach patients how to stay physically active within the restrictions of their symptoms and help develop a plan to return to normal daily activities while avoiding re-injury.
However, as we touched on above, the benefits of physical therapy for TBI patients are limited. This is because:
Treatments are not typically tailored to the specific brain areas affected by the injury, making it challenging to address a patient’s unique needs.
Physical therapy exercises aren’t designed to treat the other emotional and cognitive symptoms that TBI patients experience.
In contrast, at Cognitive FX, we use functional neurocognitive imaging (more on this below) to identify the exact areas of the brain affected for each patient and deploy multidisciplinary therapy to treat patients holistically (addressing emotional and cognitive symptoms alongside physical ones), resulting in higher success rates than other TBI treatments and therapies.
Some of the TBI symptoms and impairments that can be alleviated with physical therapy include neck and shoulder pain, muscle spasticity, vision problems, balance issues, and exercise intolerance.
About two-thirds of patients experience neck pain immediately after a traumatic injury, and almost half still have some degree of persistent neck and shoulder pain more than a month afterward. Often, neck or shoulder pain during the first few days after the injury is associated with a worse clinical outcome if left untreated.
Neck muscles provide support for the head. In the split second before impact, those muscles tighten to provide protection. This can lead to chronic tension as the muscles stay “stuck” in this protective mode, even after it’s no longer necessary. It limits mobility, creates strain on the neck muscles, and puts pressure on the cervical spine and head.
Symptoms include:

At Cognitive FX, we use neuromuscular and manual therapy to help patients find relief from these symptoms. This approach consists primarily of massages, stretches, and manipulation of soft tissue around the neck area to help muscles relax, increase blood flow in the head and neck, and reduce local inflammation.
When neck muscles are relaxed, they can better support the head, allowing patients to carry on with other activities and therapies without the additional stress of tight muscles. The aim is for these muscles to return to normal function instead of causing pain.
Further reading: Post-concussion syndrome neck pain: Causes & treatment options
Spasticity is an uncontrolled overactivity of muscles caused by disrupted signals coming from the brain. It’s common in patients with more severe traumatic brain injuries (TBIs). Patients feel constantly tightened muscles and cannot relax or stretch. Some also report muscle weakness, loss of fine motor control, and overactive reflexes when certain joints move uncontrollably.
Symptoms may include:
Moderate cases of muscle spasticity can be treated with stretching exercises to increase flexibility and reduce muscle tightness. Patients with more severe cases may need braces or splints to help with mobility and flexibility. This is not something we offer at Cognitive FX, but we can offer a referral to patients if we feel they would benefit from follow-up therapy to address their muscle spasticity.
More than two-thirds of patients experience vision-related symptoms after a TBI. This high frequency is not surprising, given that more than half of the brain’s pathways are dedicated to controlling vision and eye movement. Impact on the frontal and temporal lobes, for example, is particularly prone to causing vision issues after a head injury.
Common symptoms include:

Vision therapy involves a series of visual exercises designed to correct the problems caused by the head injury. For example, patients engage in a type of exercise called pencil push-ups, in which they hold a pencil in front of their eyes at arm’s length and then slowly bring the pencil towards the nose. The aim is to keep focus while the pencil is getting closer to the eyes. When the pencil appears as a double image, patients should move the pencil away from the nose again. Another vision therapy that we use at Cognitive FX is called the Brock String — a device that helps the patient focus on objects at different distances and gain greater control over eye teaming.
Further reading: Traumatic brain injury vision problems: Common symptoms & why multidisciplinary treatment is often necessary (and more effective)
One of the most common symptoms after a TBI involves problems with balance and motor function, which indicates problems with proprioception. Between 40% to 60% of patients experience dizziness, vertigo, unsteadiness, or lightheadedness after a head injury. These symptoms can be even worse in patients with moderate to severe TBIs, with 75% of patients experiencing lightheadedness, 38% vertigo, and 46% imbalance.
Patients often report these symptoms when they change positions, such as standing up or lying down. These symptoms severely restrict daily activities and limit participation in social life. More severe symptoms are often associated with a longer recovery, increased risk of falling, gait abnormalities, and other balance deficits.
Many areas in the brain are involved in controlling balance, but the most important is the vestibular system. Located in the inner ear, the vestibular system provides the brain with information which is crucial to maintaining balance, like what direction the head is facing and how the body is moving.
If a TBI disrupts normal functioning in the vestibular organ or the vestibular nerve, patients may experience:
We find that many patients use the terms dizziness and vertigo interchangeably, but they actually refer to two different types of sensation. Dizziness refers to a feeling of being off-balance. Patients describe it as being lightheaded and woozy. When patients are dizzy, they may struggle to walk or feel like they’re going to fall. In contrast, vertigo refers to a feeling that your surroundings are moving. Patients may feel a spinning, whirling, or tipping sensation.

Vestibular therapy is a form of physical therapy developed specifically to address balance issues. After a vestibular evaluation, patients undergo balance training exercises to reduce dizziness, headaches, and other problems related to posture. The aim is to help coordinate communication in the vestibular system.
For example, one of the balance exercises we do at Cognitive FX involves patients practicing balance while standing on a Bosu ball (an inflated rubber hemisphere attached to a rigid platform). With the dome side facing up, this device provides an unstable surface to practice balance while the device itself is stable. Then, we add another physical component to the exercise by having the patient catch and toss balls (a good oculomotor exercise). To add a cognitive element, we might ask the patient to name something that starts with the letter “g” when catching the ball and list animals in reverse alphabetical order when tossing the ball back to the therapist. In this way, we’re engaging the body and the brain at the same time.
It doesn’t matter if patients complete the exercise correctly. Often, they hit an “invisible wall,” struggle to find the right word, or lose their balance repeatedly. What matters is that the brain regions that have been overcompensating for weaker areas are finally redirected to their proper tasks, leaving the underactive regions without the usual support.
This forces the underactive brain areas to find alternative pathways. Over time, the brain identifies more efficient routes, adopts them, and TBI symptoms diminish or resolve.
Further reading: How to get the best vestibular therapy for concussion symptoms
Many patients experience low muscle strength, poor mobility, and gait problems after a TBI. These problems are common in patients with moderate to severe injuries, but even patients with mild injuries experience high-level mobility limitations, which can persist longer-term. Not surprisingly, these mobility challenges make it difficult for patients to engage in everyday tasks and lower their quality of life.
Symptoms include:
Physical therapists can suggest exercises to improve strength, flexibility, balance, coordination, and walking ability. These exercises include gait training, range-of-motion exercises, resistance training, and aerobic conditioning. Some examples include walking on a treadmill or going from sitting to standing.
Cardiorespiratory Problems
Reduced cardiorespiratory fitness and other cardiovascular problems are common after brain damage, especially moderate to severe injuries. Prolonged physical inactivity after the injury often causes these problems.
Treatment of Cardiorespiratory Problems with Physical Therapy
Therapists can suggest a variety of low-impact cardiovascular exercises to improve brain function, reduce blood pressure, and even help manage heart rate. These exercises also help patients maintain a healthy lifestyle after their injury, which is important if you want your body to heal properly.
Examples of cardiovascular exercises may include:
It’s important to start these exercises as soon as possible after the injury. Ideally, the exercise regimen should be modified to fit each patient’s needs, which is what we do at Cognitive FX. There is strong evidence to support the effectiveness of fitness training in TBI patients, including improvements in cardiovascular fitness and strength and reductions in depressive symptoms and fatigue. Evidence-based guidelines recommend exercise three to five times a week, 20 to 60 minutes in duration.
Struggling with physical activity is common after a TBI. Patients report exacerbated symptoms, such as headaches, nausea, dizziness, brain fog, changes in blood pressure, and extreme fatigue when they try to exercise.
For some, this occurs during or immediately after exercise. For others, it may take a few hours for these symptoms to show up. Most patients, however, end up stopping exercise altogether because they can’t cope with the symptoms it causes.
Further reading: How cardio exercise helps patients recover

At Cognitive FX, an initial step during therapy is establishing the patient’s sub-symptom threshold, which is how much the patient can exercise without triggering symptoms dramatically. In simple terms, patients reach their threshold if the severity of one symptom increases excessively or they notice the worsening of multiple symptoms.
With this information, our therapists can guide each patient through the correct aerobic exercise sessions, either on a treadmill or on a stationary bike. Our therapists adapt these sessions based on how the patient reacts. They stop exercises at the first signs of symptom exacerbation or if patients have a dangerously high heart rate. If patients respond well, we can gradually increase the intensity and/or duration of exercise.
Physical therapy sessions play a key role in helping patients return to their pre-injury level of functioning and improving their overall health and well-being. However, traditional physical therapy often focuses solely on specific physical symptoms, leaving other critical issues — such as difficulty thinking, brain fog, mood swings, and problems sleeping — untreated.
At Cognitive FX, we take a more comprehensive approach by addressing not just physical symptoms but also cognitive and emotional challenges caused by traumatic brain injury (TBI). Unlike traditional therapy, we go beyond symptom management. For example, our specialized vestibular therapy helps improve balance and coordination while reducing the brain’s workload by enhancing joint efficiency and optimizing how the body moves. By focusing on the entire body rather than isolated symptoms, we aim to restore overall function and efficiency, allowing patients to achieve long-term recovery and resilience.
At Cognitive FX, our clinicians specialize in treating patients with lingering symptoms from brain injuries, including patients with post-concussion syndrome (PCS), as well as other causes of head trauma, such as bacterial and viral brain infections, carbon monoxide poisoning, “chemo” brain, transient ischemic attack, and COVID-19.
We use a multidisciplinary approach that is much more effective than a single therapy. Instead of treating physical symptoms in isolation, our treatment — called Enhanced Performance in Cognition (EPIC) — is an intense, individualized program designed to treat each patient’s specific symptoms, including physical, cognitive, and emotional symptoms.
Our treatment process begins with an in-depth evaluation which includes:
A meeting with one of our doctors to review the patient’s medical history and symptoms.
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
A neurocognitive test to assess memory, concentration, reasoning, and other cognitive functions.
A psychological evaluation to identify symptoms of anxiety, depression, and other mental health problems.
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
A brain imaging scan called functional Neurocognitive Imaging (fNCI) to determine where and how the patient’s brain was affected by the injury.
The fNCI scan measures blood flow in 100 different regions of the brain while patients carry out a set of standardized cognitive tasks. It produces a series of real-time images that are combined and compared with scans from healthy people to identify the areas where neurovascular coupling (NVC) dysfunction is affecting normal brain function.
Regions are grouped according to function and then scored. Green scores show normal function, while yellow and red scores identify sections with neurovascular coupling dysfunction.

The scan also measures how these regions communicate with each other. Again, regions in green show normal activity, while regions in varying shades of blue are less active than normal.
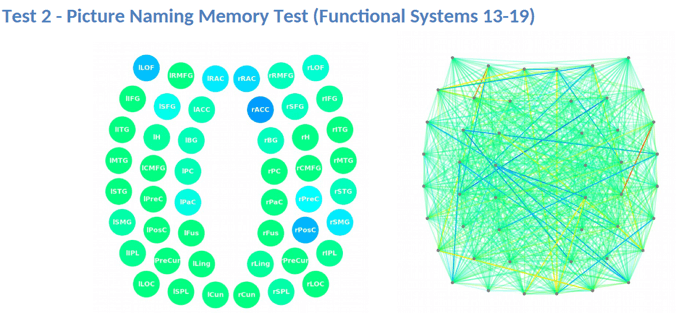
This information provides our staff with huge advantages when treating patients. For example, if we see visual systems such as target search, visual feature detection, or visual-spatial mapping that aren’t working as they should, we can tailor exercises to work on those specific areas of the brain during therapy.
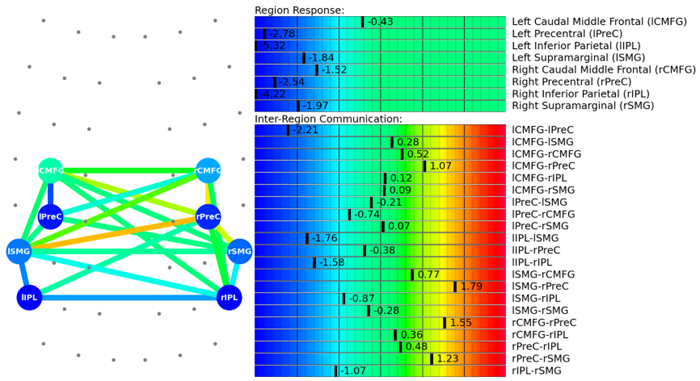
Our therapists then use the scan results to design a custom-made treatment plan for each patient, addressing the affected areas identified by the scan. This way, we can focus on the root cause of the dysfunction instead of treating isolated symptoms of a TBI.
During EPIC treatment, patients go through a three-stage cycle:
Prepare
The first step of our treatment involves a series of short bursts of cardio, followed by controlled breathing exercises. The aim is to promote blood flow in the brain and trigger the release of neurochemicals to improve the brain’s ability to respond to therapy.
One of these chemicals is called brain-derived neurotrophic factor (BDNF), which promotes the growth of brain cells and improves communication between different areas of the brain. In practical terms, every time you exercise, BDNF makes your brain more flexible and able to benefit more from subsequent therapy.
In addition, exercise also helps regulate the autonomic nervous system (ANS). Communication between two parts of the ANS — the sympathetic and parasympathetic nervous system — is often disrupted after a TBI, but aerobic exercise can bring them together again. This is visible when, after a few sessions of aerobic training, patients can continue to exercise without going over their symptom threshold (as explained above) and experiencing severe or multiple symptoms.
Our therapists constantly monitor patients during these sessions. They are trained to adjust the exercises if patients struggle or start to experience trouble breathing, heart issues, or any other medical conditions.
Activate

After exercise, patients complete a series of different therapies including:
Recover
During the day, patients also have periods of rest, including:
Neuromuscular massage to the neck and shoulders to relieve tension, improve circulation, and alleviate pain.
Relaxing in a dark room with ambient sounds, while listening to binaural beats. The app produces two close sound frequencies that the brain averages into one single frequency. After a while, natural brain waves mimic that frequency, a process similar to what you may experience through meditation.
Mindfulness techniques involve breathing techniques, guided imagery, and other practices to relax the body and mind and help reduce stress.
At the end of treatment, patients undergo a second scan to see how their brains are adapting to therapy. For some patients, the changes are significant, while for others, the brain takes longer to respond and change. Nevertheless, 90% of our patients experience improvements in their symptoms during treatment. Most of these patients go on to continue improving at home.
After treatment, our team also meets up with you to review your scan, review other test results, and give you “homework.” Your homework will include some combination of aerobic exercise, cognitive games, and cognitive rest to continue your recovery journey.
You may find it helpful to read the recovery case studies from some of our patients. Here are a few links to get you started:
Quieren is a Cognitive FX patient from the Netherlands who suffered from PCS after a bike accident.
Sam Gray sought treatment 33 years after a brain bleed.
Myrthe van Boon is a mother of two who struggled with debilitating post-concussion symptoms for years before finding Cognitive FX.
Olivia Seitz is a former figure skater who found symptom relief after more than a decade of chronic illness.
Sam Pembleton was an adolescent hit by a soccer ball in the head; she tried treatment methods for five years before finding Cognitive FX.
These patients all completed video testimonials about their initial injury and their experience at Cognitive FX.
If you've experienced one or more head injuries and your symptoms persist, you're not alone and you're not imagining it. Help is available. Peer-reviewed research shows that 77% of patients treated at Cognitive FX experienced significant improvement in their post-head injury symptoms. Cognitive FX is the only post-concussion treatment clinic with third-party validated outcomes. Schedule a consultation to see if you’re eligible for treatment.
Below are some of the recommendations we send to patients ahead of their scheduled rehabilitation process to help maximize the benefits of treatment week. These are also things that anyone suffering from post-concussion syndrome can do at home to help with daily living.
Engage in regular exercise: If you’re experiencing exercise intolerance, you may not feel great if exercise exacerbates your symptoms, but physical activity is crucial to your recovery. Start slowly and gradually increase duration and intensity as you feel better.
Practice breathing exercises: Take a few minutes every day to focus on proper breathing. Focus on breathing out for a longer period and breathing in for a short period; hold your breath briefly (one or two seconds) after breathing out.
Find a way to relax during the day: Spend ten to fifteen minutes a day relaxing. You can practice breathing during this time, meditate, listen to calming music, or just sit outside and enjoy nature.
Eat a healthy diet: Focus on eating whole, nutrient-dense foods. Avoid sugary, fatty, and highly processed foods.
Download an app for physical therapy exercises: Use an app to suggest some exercises to do at home. Make sure you ask your doctor before you start.
Don’t give up: Some days will be better than others, but don’t give up. Even if your recovery takes longer than expected, don’t lose hope that you will feel better. Many patients start to accept their symptoms as their new normal. But you don’t have to live with severe symptoms forever.
Contact us for a free consultation — we’d be happy to advise you on the next steps for your current situation.

Toshi graduated from Brigham Young University Idaho with a degree in exercise science in 2016. He then graduated from Idaho State University with his Doctorate in Physical Therapy in 2019. While in school, he did rotations in vestibular therapy, outpatient orthopedic, pediatric and acute care settings. At Cognitive FX, Toshi is a Neuromuscular Therapist. He hopes to utilize his knowledge of vestibular therapy and orthopedics to help patients receive the care they need.

“Post-traumatic brain injury syndrome” refers to long-term repercussions from concussions and other head injuries. Someone using this term could be referring to one of three conditions:

Dry needling and acupuncture can help relieve certain post-concussion symptoms. They are not a cure-all, either for acute concussion or post-concussion syndrome, but if you suffer from headaches,...

Recovering from post-concussion syndrome (PCS) is challenging, but with the right guidance, substantial progress and symptom relief are possible, even years after the initial injury.
In post-concussion syndrome (PCS), a patient with a mild traumatic brain injury (mTBI) experiences persistent symptoms from the injury. If left untreated, the symptoms might last months, years, or...

Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...

If you’ve suffered a concussion, you may have already encountered the Post-Concussion Symptom Scale (PCSS). This self-report questionnaire is one of the most widely used tools for documenting...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY