A Guide to Post-concussion Syndrome on Reddit
Post-concussion syndrome is downright frustrating to experience. Doctors often miss it during diagnosis, and even if they do make the diagnosis, treatment methods vary considerably from clinic to...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Modern traditional medicine has transformed the way we diagnose and treat disease and injury. And in most cases, it is extremely effective. But it doesn’t always provide the solutions patients need to improve their quality of life, especially when they suffer from poorly characterized ailments (such as unexplained chronic pain, fibromyalgia, or movement disorders).
If you know what it’s like to see doctor after doctor who just can’t seem to help, then you know the appeal of alternative medicine. And if you’re exploring functional neurology (also known as chiropractic neurology), you probably have a lot of questions.
Depending on who you ask, you can get dramatically different answers.

Full disclosure, we’re not functional neurologists. Our team includes a clinical neuropsychologist, cognitive scientist and neuroimaging expert, a neurosurgeon, a neuroradiologist, a clinical neuroscientist, a clinical psychologist, and many other trained health professionals.
We work together to diagnose and treat patients with long-lasting symptoms from concussions and other mild head trauma (if you’re curious, we explain more of what we do at the end of this post). We do not practice functional neurology, but we do get questions about the field and what it has to offer from our post-concussion patients.
Since our patients want to understand their options better — and have expressed confusion about the difference between neurology and functional neurology — we’ve endeavored to answer as many of those questions as we can. In this post, we’ll do our best to explain:
If you’re experiencing symptoms that won’t go away after a concussion, we can help. On average, our patients improve by 75% after treatment. To learn about diagnosis and treatment options, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
Functional neurology is a treatment discipline for various neurological disorders. Functional neurologists may have subspecialties, but in general, they treat brain injury patients, degenerative disorders (such as dementia), movement disorders, vestibular challenges (i.e. balance and dizziness issues), or any other neurological disease or disorder of unknown origin (typically something that traditional doctors have not been able to diagnose and treat successfully).
Functional neurology does not include surgery or pharmaceutical solutions, but may employ some combination of chiropractic manipulation, various therapies, and recommended lifestyle changes.
The explanation which functional neurology provides for neurological disorders is still a hypothesis and difficult to convey in plain language, but here’s the short version based on a recent review of functional neurology.
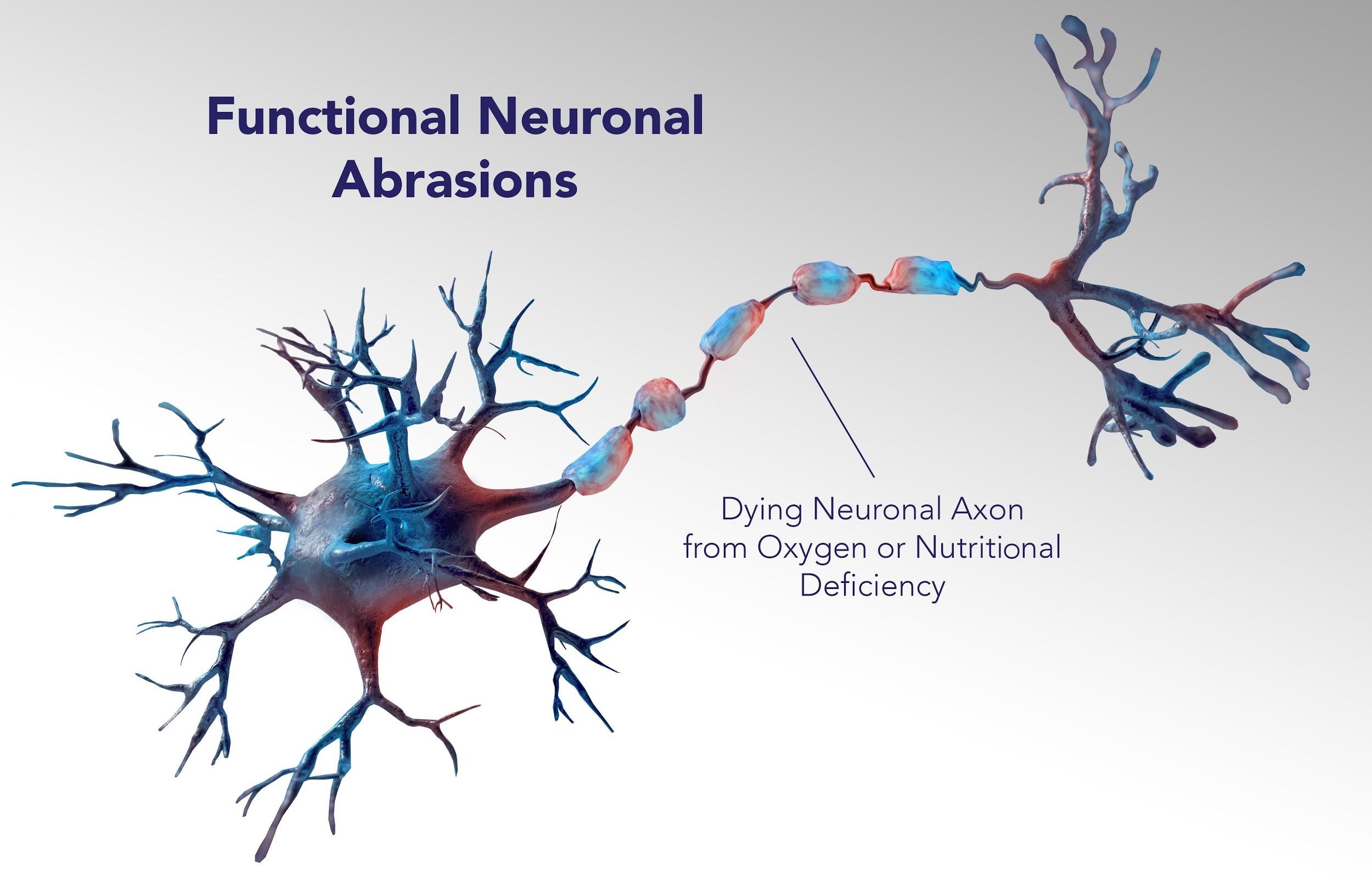
Functional neurology treats the source of a patient’s ailments as “functional aberrations of the neuraxis” — meaning, clusters of neurons which aren’t working together in the way they are supposed to — in various locations throughout the central nervous system.
Functional neurologists attempt to assess the “central integrative state,” or CIS, of functional units of neurons within the nervous system to determine where those functional aberrations are. The CIS is essentially how they refer to the current healthiness of those neurons.
Functional neurologists believe functional aberrations come from lesions, which are the result of some deficiency — perhaps there are dead cells (worst case scenario), or maybe they aren’t getting enough oxygen or nutrition.
Whatever the case, these aberrations cause communication snafus throughout the central nervous system and lead to hyper- or hypo-functional areas of the brain. In turn, this situation results in “diverse motor, sensory, visceral, or cognitive symptoms”.
Many functional neurologists are also interested in fatigability (can you maintain a healthy response to a certain stimulus?) and hemisphericity (the belief that neurological symptoms come from some imbalance between the two halves of the brain or an area therein).
While their treatment protocols are highly varied, many functional neurologists base treatment on the idea that stimulation of an area is enough to engage the brain’s inherent neuroplasticity, which is its ability to heal itself from certain injuries and conditions.
Note: Neuroplasticity is a proven phenomenon and forms the basis of many emergent therapies. We’ve written before about how neuroplasticity can be leveraged to recover from minor traumatic brain injury.
For example, one treatment that functional neurologists use in the case of vestibular disorders (trouble with balance, dizziness, nausea, and so forth) is the GyroStim. It is considered an experimental device since it has not been cleared by the FDA for use in diagnosis or treatment, but its effect bears some similarity to the Epley Maneuver and other traditional therapies for vertigo.
Because functional neurology is such a new field, treatments are not yet standardized. Functional neurologists adjust treatment regimens based on what their patients need. While some treatments may not be effective, others may be very effective. For patients who have not had luck via traditional medicine, functional neurologists’ willingness to try new therapies and borrow what works from other disciplines is often a breath of fresh air.
Many functional neurologists have happy patients (and this is no small feat, considering the difficulty and range of their ailments). It is difficult to say with certainty exactly which aspects of a patient’s recovery are due to functional neurology and which aspects are due to things such as lifestyle changes or the placebo effect, which can sometimes be more powerful the more complicated the treatment provided.
This is not to say that functional neurology isn’t a legitimate treatment. But from a strictly scientific perspective, there is more work to do for functional neurologists to demonstrate:
Having said that, it’s also important to understand the context of trying to do research on the effectiveness of therapy as applied to neurological conditions. It is difficult to do a true, randomized, double-blind, controlled trial (RCT) when you’re using a complex type of treatment that is highly individualized and can vary based on the responsiveness of the patient during treatment and on spontaneous adjustments by the therapists.
In addition, it is nearly impossible to create a true placebo condition with either approach, much less create a “blind” placebo situation, wherein the therapist does not know whether they are administering the true therapy or the placebo one. We’ve run into the same difficulties in our own research.
If there is one criticism we would mention here, it’s that many of the functional neurology studies conducted have been with such small groups of people that, statistically speaking, you can’t adequately draw conclusions about what happened. In our own research on EPIC treatment, we've used large numbers of subjects and attempted to control for placebo by comparing patients who do EPIC treatment with patients who do not undergo treatment of any kind. We do think that functional neurology would benefit from more rigorously designed research studies.
Again, that's not to say that whatever treatment a functional neurologist chooses won’t work. Whether you want to give functional neurology a try is your decision. Most of the therapies and techniques used are at the very least harmless and in many cases appear to help patients. However, any treatment program is an investment of time and money, so it’s worth asking if there’s a better alternative for your condition (something we’ll discuss shortly).
To become a board-certified functional neurologist, you have to undergo 350 credit hours of extra training (specifically in functional neurology) after completing an MD (Doctor of Medicine), DO (Doctor of Osteopathic Medicine), DC (Doctor of Chiropractic), ND (Naturopathic Doctor), or PT (Physical Therapist). That said, the vast majority of practicing functional neurologists are chiropractors.
If you decide to visit a functional neurologist, make sure they are properly credentialed. “Functional neurologist” is not intended to be a title anyone can grant themselves. They should be certified by the American Chiropractic Neurology Board.

Traditional neurologists are medical doctors; functional neurologists are not, by virtue of their functional neurology training, medical doctors. If their initial degree was in traditional medicine, they may be a medical doctor; however, most functional neurologists start with a chiropractic degree. Understandably, there has been some pushback from the medical community over the name “functional neurologist,” since the name can be confusing for many patients.
In this section, we’ll outline key differences between the two. We’ll also discuss which conditions are more appropriately treated by each.
Traditional medical neurologists get (you guessed it) a full, traditional medical education. They spend time learning about chemical and metabolic processes in the body so they can treat the underlying causes of known conditions. They learn when and how to prescribe medication, order and interpret diagnostic imaging, and so forth.
They are at their best when your neurological condition can be treated and/or managed by medication. For example, people who suffer from migraines and epilepsy are typically well served by visiting a neurologist. Patients with degenerative disorders — think Alzheimer’s, Parkinson’s disease, multiple sclerosis — can also benefit from seeing a neurologist, although they’re often co-managed by a neurologist and a neuropsychologist. The neurologist oversees medical treatment, and the neuropsychologist monitors disease progression, cognitive symptoms, and therapy regimens.
These conditions cannot be treated by spinal adjustments, but they can be helped with traditional medicine, which is why a neurologist is the better choice.
For the purposes of this piece, we will assume that functional neurologists begin with chiropractic training. Chiropractors spend years learning about the central nervous system and the spine. They spend more time during diagnosis and treatment looking at whole-body care and the effects of lifestyle on health than do most neurologists.
To become a chiropractic neurologist, they complete additional coursework on neurological disorders and the functional neurology approach to treating them.
Functional neurologists are in their element while treating symptoms of unknown cause, especially if they are related to the vestibular (balance) system. They can also help patients with neck soreness, back pain, and other symptoms relating to the spine because of their chiropractic training.

When it comes to concussions (or other head trauma, such as carbon monoxide poisoning), who to see depends a lot more on the specific healthcare provider and their specialty. If you’re looking for help treating a concussion or similar condition, it’s important to find someone with experience treating mild traumatic brain injuries (mTBIs). Why? Because it’s a complex issue for which traditional methods (rest, or perhaps medication) have fallen short.
Keep in mind that not all neurologists are trained in concussion care. Many traditional neurologists will order a structural MRI or CT scan if you come to them after a head injury. If that scan comes back negative, there isn’t much they can do for you. They might offer prescriptions to alleviate certain symptoms or, if you’re lucky, refer you for some therapies.
But keep in mind that most medications were not tested on people with brain injuries. We don’t fully know what effects they have, and they may even inhibit your recovery.
On the other hand, functional neurologists will look at how the whole body is impacted by your condition and may prescribe some combination of visual, vestibular, and occupational therapy. They’re likely to devote more time to exploring what’s wrong, beginning with a thorough exam (something they call a neurological examination) after identifying their patient’s symptoms.
Because of that, they’re more likely to help people with post-concussion syndrome (which occurs when symptoms of a concussion do not disappear with time) than many neurologists, particularly for patients with dizziness and balance disorders.
Keep in mind that most functional neurologists don’t have access to advanced neuroimaging (such as MRI, fMRI, SPECT, and CT scans), which can be invaluable during brain injury detection and diagnosis. We don’t want to minimize their accomplishments — there are many positive stories from concussion patients in the care of functional neurologists — but it’s important to know all the facts going into such an important decision.
In summary, if you’re choosing between a neurologist who doesn’t specialize in concussion treatment and a functional neurologist who has clinical experience with concussion patients, we’d pick the latter.
However, life often doesn’t consist of forced dichotomies such as these, and we actually recommend an alternative for post-concussion care. For example, for post-concussion patients with emotional or cognitive symptoms (instead of or in addition to balance issues), we recommend neither a neurologist nor a functional neurologist. Instead, a neuropsychologist (like our own Dr. Alina Fong) would be better equipped to help.
If you’re frustrated with your medical providers after suffering head trauma, and you’re enduring symptoms that won’t go away, you’re in good company. Even though up to 30% of concussion patients develop post-concussion syndrome (PCS), many doctors aren’t aware of the condition, let alone know how to treat it beyond “rest in a dark room and hope you feel better.”
Fortunately, there are much better ways to recover from a concussion than resting in a dark room. And if you do have PCS, we can not only see how the concussion affected your brain function, but we can provide intense therapy to help your brain recover, too.
Note: If you’re skeptical at this point, that’s totally fair. After all, we just mentioned how important it is to have therapies and treatment methods that are backed up by research. You can view our peer-reviewed papers here. We incorporate both our own research and findings that come out of highly-respected labs at UCSF, Stanford, UBMD, and more.
You can read more about post-concussion treatment and how it works on other posts we’ve written, but we’ll highlight some of our advantages over other post-concussion treatment programs below:

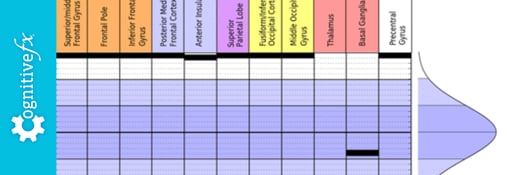
fNCI is a type of fMRI (functional magnetic resonance imaging). Instead of showing brain structure like a standard MRI does, fMRI shows blood flow. Using the norms and testing protocols we developed by studying thousands of brains, we’re able to detect characteristic hyperactivity and hypoactivity in regions of PCS patients’ brains.
For example, if your thalamus isn’t fully activating when it should, we can see that (and explain why you’ve had such bad light sensitivity or difficulty sleeping). Once we know precisely which parts of your brain were affected by the concussion(s) and how, we can tailor your treatment program accordingly.
In addition, each patient has an initial fNCI scan and a final fNCI scan. This allows us to see objectively how much your brain has improved during the course of treatment.
We’ve been able to bring together many diverse therapies that are all impactful during concussion treatment. While many clinics can only provide siloed physical, cognitive, and occupational therapy, we’re able to provide:
And more. Oftentimes, the boundaries between these treatments are blurred. You might find yourself tapping your heel in time to a metronome while reading arrow directions off a chart as a therapist not-so-subtly tries to distract you in the background. Next, you might balance on a Bosu ball while tapping the green Dynavision buttons with your left hand and the red ones with your right.
All of the exercises we incorporate into the treatment regimen are designed to challenge your brain, pushing those hypoactive brain regions to engage. With the right incentive (not just stimulation), our brains will engage their inherent neuroplasticity, resulting in healthier signaling habits that we can see on the second fNCI scan.

While we tailor each treatment plan according to symptoms and fNCI scan results, the building blocks of treatment stay the same. We employ and improve the same methods over and over to help the hundreds of patients that come to us for treatment each year.
In contrast, if you see a neurologist for post-concussion syndrome, that doctor will likely refer you to separate therapists for treatment (if you manage to get a referral at all). And if you see a functional neurologist, you’ll be getting their own, homebrewed version of treatment. While aspects of that treatment may be effective (we wouldn’t suggest otherwise), it is not as rigorously or consistently tested as our methods are.

If you’re wondering what treatment at our clinic is really like, we invite you to read our patient’s recovery stories — Olivia, a former figure skater who suffered for years from post-concussion syndrome without knowing why; Sam, a student who spent five years trying every concussion clinic in Ontario before finding us; or Myrthe, a mother who was told she would never recover from her skiing accident.
You can also watch as many patient testimonial videos as you like.
If you’re interested in learning more about what you can do to recover, schedule a consultation. We’ll help you understand your options and determine if you’re eligible for treatment.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

Post-concussion syndrome is downright frustrating to experience. Doctors often miss it during diagnosis, and even if they do make the diagnosis, treatment methods vary considerably from clinic to...

The fight with cancer is difficult enough, so it’s understandable if you’re frustrated and confused by the cognitive symptoms that can crop up after chemotherapy. Memory problems? Clouded thinking?...
“Eat right and exercise” – this advice is nothing new, you’re tired of hearing it and you’re tempted to tune it out right now – but it’s not going away. In fact, when it comes to brain health, this...

If you notice symptoms after a concussion, it’s best not to wait to seek treatment. If you’re the type to “wait it out” and see if things get better, then we recommend waiting no longer than three...

You lie awake at 2 a.m., exhausted but unable to sleep. When sleep finally comes, strange dreams jolt you awake. Morning arrives and you feel like you never rested at all.
fMRI (functional Magnetic Resonance Imaging) is often a more sensitive method for detecting brain injury such as concussion than a standard MRI (Magnetic Resonance Imaging) brain scan. fNCI...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY