Many people are surprised to learn that concussions can have long-term effects if left untreated. Chronic concussion syndrome is a less common term for persistent post-concussion symptoms (also known as post-concussion syndrome, or PCS). If you suffer from headaches, brain fog, vision issues, fatigue, short-term memory problems, irritability, feelings of overwhelm, or other persistent symptoms after a head injury, you might have chronic concussion syndrome.
In this post, we’ll explain what causes those stubborn symptoms, along with what you can do to be rid of them:
If you’re experiencing symptoms that won’t resolve after a minor head injury, you’re not alone. And you’re not crazy. 90% of our patients show symptom improvement after just one week of treatment at our center specializing in post-concussion therapy. To see if you are eligible for treatment, sign up for a consultation.
What Is Chronic Concussion Syndrome (Persistent Post-concussive Symptoms)?
.jpg?width=1000&height=445&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(5).jpg)
Chronic concussion syndrome (post-concussion syndrome, or PCS) can be diagnosed once you’ve experienced persistent symptoms for at least three months after sustaining a head injury. Concussions can come from jostling, whiplash, or a direct blow to the head.
While any concussive event (falls, car accidents, contact sports, violence, and so forth) can result in symptoms, most people recover after one to two weeks. Up to 30% go on to develop persistent symptoms which do not go away without treatment. You do not have to experience loss of consciousness to develop serious symptoms following the initial injury, nor do you have to have sustained previous concussions. Symptoms can develop days or even weeks after the concussion.
While concussions are certainly the most common way to develop chronic head injury symptoms, they aren’t the only way. You might also develop PCS after one of these closed-head injuries:
What all of these injuries have in common is a change in neurovascular coupling (NVC). Neurovascular coupling is the dynamic relationship between neurons and the blood vessels that supply them. After a concussion, your immune system causes inflammation around the injury. The affected parts of your brain experience a temporary breakdown of tiny structures in and around those cells.
The result is dysfunctional NVC: a mismatch between how much oxygen your neurons need at a given time and what’s delivered in that moment. When those cells don’t receive what they need, they may not be able to complete the tasks assigned to them (such as encoding a new memory, filtering out unnecessary sound and noise, and so forth). While your brain might be able to complete the task by using other neural pathways, these pathways will be less efficient and tire you out more quickly.
In patients suffering from persistent symptoms, dysfunctional neurovascular coupling causes hypoactive brain regions (regions that aren’t responding as much as they should to stimuli). These brain regions typically cannot heal themselves; instead, it takes an intentional therapeutic approach to restore healthier neurovascular signaling pathways.
If NVC dysfunction seems confusing to you, conceptualize it as road traffic. A healthy brain would distribute the “traffic” — i.e., the signaling and blood flow dynamics needed for a task such as reading — equally along existing pathways. NVC dysfunction is like getting stuck in a traffic jam or taking a frontage road instead of the highway. It’s inefficient and requires more fuel to get to the same place.
Some symptoms of PCS are related to which brain regions were affected by your brain injury. For example, if you have poor neurovascular function in your superior frontal gyrus, you might struggle with executive function (decision making, planning, etc.). But some symptoms come from the overall effect of neurovascular coupling abnormalities on the brain. NVC dysfunction causes post-injury neural fatigue that can lead to irritability, headaches, brain fog, and more.
Other Causes of Chronic Post-concussion Symptoms
While neurovascular coupling dysfunction is the most common culprit, chronic symptoms following a concussion often stem from a combination of secondary conditions.
The autonomic nervous system (ANS) can become dysfunctional after a brain injury. It controls or influences most organ systems in the body, governing processes such as your heart rate, blood pressure, digestion speed, body temperature, pupillary response, and more. Widespread neurological dysfunction following brain trauma could indicate ANS dysfunction. Common symptoms of ANS dysfunction are listed in the following section.
.jpg?width=552&height=419&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(7).jpg)
Brain regions critical for proper hormone regulation — such as the pituitary gland and the hypothalamus — can be injured by mild or severe traumatic brain injury as well. Patients with chronic concussion symptoms should visit an endocrinologist or other doctor able to diagnose and treat post-injury hormone dysfunction.
Vision functions can be affected by head trauma as well. Vision dysfunction often requires vision therapy to correct. In the meantime, post-concussion vision problems can be responsible for a host of symptoms, from headaches to difficulty reading to feeling overwhelmed while grocery shopping.
Some patients also experience changes in vestibular function following a head injury. The vestibular system, located in the inner ear, communicates closely with the visual system, the body (proprioceptive system), and the brain to determine your orientation in space. Concussions can disrupt communication, resulting in symptoms such as dizziness, nausea with motion, vomiting, and sleep disturbances. Fortunately, post-concussion vestibular therapy is often effective in resolving these symptoms.
Which Concussion Symptoms Can Become Chronic?
.jpg?width=552&height=414&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(8).jpg)
While the exact numbers change with time, we see a consistent pattern in our patients who suffer from chronic symptoms following a minor head injury. Changes in emotional regulation and mental health are the most common, followed by brain fog, difficulty focusing, headaches, and short-term memory problems.
But the total number of symptoms that you could experience goes far beyond that list, especially when you consider the symptoms of post-concussion autonomic dysfunction listed in this chart:-1.jpg?width=552&height=582&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(1)-1.jpg)
For in-depth discussions on what causes common physical and cognitive symptoms after a concussion and how to resolve them, please see the following posts:
How Long Do Chronic Concussion Symptoms Last
-1.jpg?width=552&height=368&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(2)-1.jpg) Sam Pembleton (pictured above in red) suffered from chronic concussion symptoms for five years after getting hit in the head with a soccer ball.
Sam Pembleton (pictured above in red) suffered from chronic concussion symptoms for five years after getting hit in the head with a soccer ball.
Chronic concussion symptoms can last for years until they’re treated properly. One study found that just 27% of post-concussion syndrome patients meeting diagnostic criteria at three months post-injury made a full recovery. In this study of wartime concussive injuries, 72% of study participants experienced a worsening of their symptoms after five years.
But not all news on long-term recovery from mild TBI is grim: We’ve found no difference in recovery rates for our patients based on their age or the length of time passed since their injury. On average, our patients report a 60% improvement in their symptoms after one week of treatment in our clinic. Our follow-up research confirmed that they continue to improve at home after treatment.
Further reading: Recovering from post-concussion syndrome and How to handle sport-related concussion recovery
Ultimately, once you’ve developed chronic symptoms, how long your symptoms last depends on the quality of treatment you receive. Many PCS patients have not received any therapy for their symptoms. Some have been given medications to manage symptoms (but these meds don’t resolve the root issue). And those who have had some treatment often have not gone through multidisciplinary treatment programs that were personalized for their needs. The therapy might not have been at the right pace or intensity to correct neurovascular coupling dysfunction.
One of our patients, Sam Pembleton, received treatment at all of the sports medicine and concussion clinics she could find in Ontario with no real symptom improvement. She even flew to a renowned clinic in Boston, but they sent her home because she wasn’t responding to treatment. She suffered from persistent post-concussion symptoms for five years before she came to Cognitive FX. After treatment at our clinic, she was able to work, finish school, go out with friends, and simply enjoy life again.
One of our other patients, Myrthe van Boon, was told by her neurologist that she would never recover from her skiing head injury. But she began to improve partway through her treatment week at Cognitive FX. Now, she’s able to laugh, dance, and care for her daughters as a healthy mom.
Post-concussion syndrome is not one-size-fits-all. The brain regions affected by your brain injury are not necessarily the same as the regions that were damaged in someone else. But unlike Cognitive FX, most treatment facilities don’t have the brain imaging technology to determine precisely how and where the patient experienced neurotrauma.
That’s why providing each patient with a functional neurocognitive imaging scan (fNCI) is so important to our work. Using the scan (along with evaluations of ANS, vision, vestibular, and brain stem function), we can determine where brain function was negatively impacted and in what way. We can then tailor your treatment regimen accordingly, which is why patients like Sam and Myrthe, who tried many different doctors, were able to make progress under our care, but not elsewhere.
Further reading: Can a CT scan show brain damage from post-concussion syndrome?
How to Recover From Chronic Concussion Syndrome
-1.jpg?width=552&height=306&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(4)-1.jpg)
At Cognitive FX, we offer treatment of post-concussion syndrome. We tackle neurovascular coupling dysfunction, autonomic dysfunction, vision issues, and vestibular problems. Because treatment often results in better sleep, symptoms stemming from poor sleep quality often improve as well.
How We Evaluate Chronic Concussion Patients
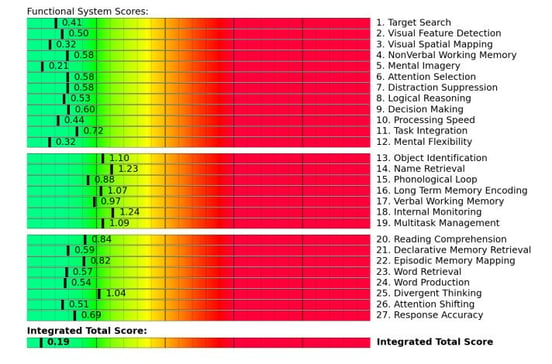
All patients receive a functional Neurocognitive Imaging (fNCI) scan before and after treatment. fNCI is a type of functional MRI that looks at blood flow dynamics throughout 56 regions of the brain while the patient performs a series of standardized cognitive tasks. We also evaluate connections between imaged brain regions.
We can infer cognitive impairment in brain regions involved in specific tasks, such as visual-spatial mapping, attention shifting, verbal working memory, name retrieval, and multitasking. The following is an example scan from a patient who experienced NVC dysfunction after an acquired brain injury:
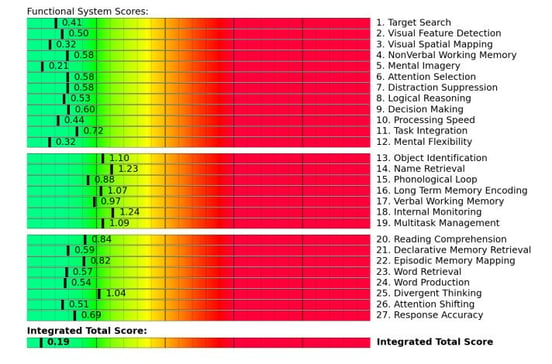
Scores in red or yellow generally indicate a need for rehabilitation. These results give us a clear idea of which brain regions are struggling. In addition, we can evaluate which brain regions have healthy communication patterns (are or are not synchronized with each other as expected) or unhealthy communication patterns (are more or less active than they should be relative to certain other regions).
-2.jpg?width=552&height=256&name=image9%20(1)-2.jpg)
For example, the scan above shows the right anterior cingulate cortex (rACC, in blue) as underactive. rACC plays a key part in sustained attention and is involved in other types of attention as well. Knowing that, the therapists could include sustained attention exercises for the patient during treatment.
Some patients will have localized dysfunction (as shown above) and others will have widespread dysfunction throughout the brain. Both can cause the same degree of symptoms. Knowing the cause helps us to treat the condition more accurately.
In addition, we evaluate all patients for their vision, ANS, and vestibular function, along with neuropsychological testing and evaluation of reaction times. Some concussion symptoms stem from deficits in these areas and not just from NVC dysfunction. Therefore, conducting these additional evaluations is key to treating the whole person. We then tailor your treatment regimen according to your ability and needs.
What Treatment Involves
.jpg?width=1999&height=1333&name=How%20Do%20You%20Know%20If%20You%20Have%20a%20Concussion%20(5).jpg)
Treatment for persistent post-concussion syndrome involves a three-step cycle that repeats: Prepare, Activate, and Recover.
Prepare.jpg?width=1999&height=1333&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(1).jpg)
Every day includes supervised cardiovascular exercise followed by controlled breathing. Short bursts of cardio followed by breathing decrease sympathetic nervous system dominance, helping the ANS to function better as a whole. Cardio also improves blood flow in the brain and releases neurochemicals that make it easier for the brain to benefit from therapy. For example, exercise releases brain-derived neurotrophic factor (BDNF), which improves cognitive flexibility and has been shown to improve therapy outcomes in mild traumatic brain injury (mTBI) patients.
If you have exercise intolerance, your therapists will teach you how to exercise at the sub-symptom threshold. Post-injury exercise is key for brain health and recovery.
Activate
.jpg?width=248&height=372&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(6).jpg) Therapy at Cognitive FX is multidisciplinary. You’ll work with a rotation of therapists who are experts in brain injury rehabilitation. Some of the therapies you may receive include…
Therapy at Cognitive FX is multidisciplinary. You’ll work with a rotation of therapists who are experts in brain injury rehabilitation. Some of the therapies you may receive include…
Some therapies combine disciplines for greater effect. For example, you might balance on a Bosu board (exercising your vestibular system and the part of the brain governing balance) while tossing color-coded tennis balls back and forth (hand-eye coordination and reflex response) and adding or subtracting from a running tally based on which ball you caught (memory, problem-solving, attention, etc.).
Or, during neurointegration therapy, you might draw the mirror image of a given pattern while the therapist asks you simple questions.
These therapies are designed to engage your brain’s natural ability for recovery (neuroplasticity) to help restore healthy neurovascular communication throughout the brain.
Further reading: Neuroplasticity therapy for brain injury recovery
Recover
-1.jpg?width=552&height=246&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(3)-1.jpg)
Taking moments to let your brain rest is imperative if you are to do so much therapy in one day. Some examples of scheduled brain breaks include…
- Neuromuscular massage. Therapists massage the neck and shoulders to relieve chronic pain and tension, relax muscles involved in vision, improve circulation, and alleviate headache pain.
- Brainwaves. The binaural beats app we use produces two frequencies that are very close together. If you listen to a different frequency in each ear, your brain will average them together to produce one frequency. We set the parameters so that the frequency your brain creates is the same frequency you would experience through meditation. This frequency will propagate in your brain waves as you listen. As a result, you gain some of the restorative benefits of meditation without being an expert in meditation.
- Mindfulness. Patients learn mindfulness techniques during their time at the clinic.
What Comes Next for Recovery
.jpg?width=1000&height=445&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(2).jpg)
All of our patients receive a take-home packet with brain exercises and recommendations for continued therapy at home. If you need a referral to a specialist in your area, our clinicians will discuss that as well.
Four key elements of continued recovery are consistent exercise, a brain-healthy diet, good sleep habits, and patience. You may find these resources helpful in the process:
One aspect of recovery we do not address is medications. There is no medicine clinically proven to treat post-concussion syndrome. Many well-intentioned health care providers prescribe meds to alleviate specific symptoms, such as antidepressants for mood changes or sleep problems and anti-seizure meds for headaches. These medications can’t address the underlying problem (NVC, autonomic issues, etc.) and so are only temporary fixes, if they help at all. That’s one of the reasons therapy is so important — medications simply aren’t enough to cause a full recovery for most patients.
Due to side effects, post-injury metabolic changes, and other risk factors, some medications can actually cause worse symptoms than the original injury. Oftentimes, these meds don’t help at all and are even more dangerous for pediatric patients because adolescents metabolize medication differently than adults do. For an in-depth discussion of how and when medication for PCS is helpful, along with when it’s not, read our post on medication for post-concussion syndrome.
On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation.

.jpg?width=1000&height=445&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(5).jpg)
.jpg?width=552&height=419&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(7).jpg)
.jpg?width=552&height=414&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(8).jpg)
-1.jpg?width=552&height=582&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(1)-1.jpg)
-1.jpg?width=552&height=368&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(2)-1.jpg)
-1.jpg?width=552&height=306&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(4)-1.jpg)
-2.jpg?width=552&height=256&name=image9%20(1)-2.jpg)
.jpg?width=1999&height=1333&name=How%20Do%20You%20Know%20If%20You%20Have%20a%20Concussion%20(5).jpg)
.jpg?width=1999&height=1333&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(1).jpg)
.jpg?width=248&height=372&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(6).jpg) Therapy at Cognitive FX is multidisciplinary. You’ll work with a rotation of therapists who are experts in brain injury rehabilitation. Some of the therapies you may receive include…
Therapy at Cognitive FX is multidisciplinary. You’ll work with a rotation of therapists who are experts in brain injury rehabilitation. Some of the therapies you may receive include…-1.jpg?width=552&height=246&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(3)-1.jpg)
.jpg?width=1000&height=445&name=How%20to%20Recover%20from%20Chronic%20Concussion%20Syndrome%20(2).jpg)