The fight with cancer is difficult enough, so it’s understandable if you’re frustrated and confused by the cognitive symptoms that can crop up after chemotherapy. Memory problems? Clouded thinking? Fatigue? No thanks!
The good news is that you’re not losing your mind: Cognitive impairment after chemotherapy is a real medical condition, and it is treatable.
Oncologists have known about cognitive symptoms after chemo since the 1980s, but many cancer survivors aren’t treated for the condition. Many doctors don’t know how to treat these symptoms in their patients. Some oncology doctors are simply slow to notice it in their patients. Others mistake the symptoms of chemo brain on mental health. Patients often think they just have to live with the changes.
Treatment for chemo brain is relatively new. But that doesn’t mean you shouldn’t have access to it. In this post, we give you a full look at:
We don’t treat cancer; it’s not our specialty. But we do treat brain injury, and chemo brain is a brain injury. Because of that, we’ve had some success treating chemo brain patients. We’ll explain how and why in this post.
If you’re suffering from lingering cognitive symptoms after chemotherapy, you’re not alone. If you have completed your cancer treatment and want to reverse chemo brain, sign up for a consultation with our team. We’ll take a look at your symptoms and medical history, then advise you on the next steps in your recovery.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
What Causes Chemo Brain?
Chemotherapy drugs target rapidly proliferating cells, aka cells that multiply quickly. This is because cancer cells replicate more quickly than most of the cells in your body. But some cells proliferate more quickly than others — for example, your skin, eye, and hair cells.
Since most chemotherapy agents are not able to focus exclusively on cancer cells, they will kill some of the other cells in your body, too. Chemotherapy is effectively one big gamble that the drugs will kill the cancer cells faster than your healthy cells.
Unfortunately, that means every part of your system can take a hit from chemo — such as your vascular system, your blood-brain barrier, and all your organs. Hair cells and eye cells may sustain heavier losses since they reproduce more rapidly than other cells; it’s why many cancer patients lose their hair during treatment.
All the dying cells cause inflammation and other problems, which in turn affect cognitive function in over 60% of chemotherapy patients. Some experience chemo brain for only a short while, and others have it for years after their cancer treatment. There may be a connection between previous brain injury (even a “mild” concussion) and developing the longer-lasting chemo brain symptoms; more on that later.
While the changes aren’t structural — your brain will likely look normal on a regular MRI because the damage is subcellular — scientists have observed changes in the brain with functional MRI (fMRI) after chemotherapy. fMRI looks at blood flow patterns throughout the brain and sheds light on brain function, which is why it is a useful imaging tool for chemo brain.
Note: Chemotherapy isn’t the only cancer therapy known to cause chemo brain. Radiation and other common treatments may result in cognitive difficulties as well. Even leukemia and lymphoma patients who received blood and marrow transplants have an increased risk of developing chemo brain. Cancer treatment is complicated, and chemotherapy is just one contributor to cognitive changes.
Chemotherapy Can Cause Neurovascular Coupling Dysfunction
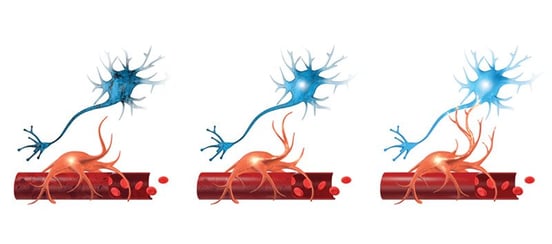
The culprit behind cognitive changes after a brain injury is neurovascular coupling dysfunction. It’s also a key but little-known component of chemo brain.
Neurovascular coupling (NVC) is the relationship between your neurons and the blood vessels that supply them with what they need to do their jobs. When your neurons fire, they need a certain amount of oxygen and other resources. The brain doesn’t have an infinite supply of those resources, so it needs to deliver them efficiently for you to function at your best.
Your brain cells — neurons and glial cells (the support and immune cells of the brain) — and the blood vessels that supply them have regular, established methods of communicating with each other. But chemotherapy can disrupt that healthy communication pattern. Chemo drugs like methotrexate reduce the population of new, healthy glial cells and cause inflammation (which we know to be a key part of developing NVC dysfunction after traumatic brain injury). That inflammation pulls the focus of remaining glial cells away from the neurons they assist and into “fight the invader” mode.
In addition, chemotherapy may also have a negative impact on vascular structure, which further exacerbates the communication problems your brain experiences during and after chemotherapy.
Over time, all these issues make your brain cells supremely unhappy. When chemo finally stops and the inflammation subsides, your brain cells will try to piece their regular communication patterns back together. In some cancer patients, this process works just fine. But for those who develop chemo brain, those communication patterns don’t return to normal without a little outside help.
The result is NVC dysfunction. Think of NVC dysfunction like a traffic jam in your brain. Roads that used to be clear are congested with cars, so you have to drive the long way around to get to your destination (if you can even get there at all). Doing so takes a lot of extra time and energy and is generally a frustrating experience. This might happen in some areas of the brain and not others, resulting in some brain regions that are hypoactive (not doing what they should be) and some that are hyperactive (doing too much, or taking too many resources to get the job done).
The result is the symptoms associated with chemo brain.
The Symptoms: Chemo Brain Fog, Fatigue, and More
Cognitive chemo brain symptoms include:
- Brain fog.
- Difficulty concentrating or changes in attention.
- Poor executive function (decision-making, multitasking, planning, etc.).
- Sleep problems.
- Trouble recalling words in conversation.
- Worse short-term memory and working memory.
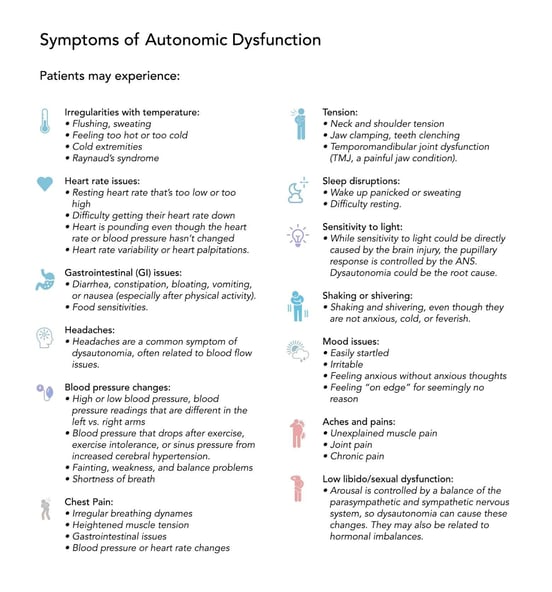
Because chemotherapy’s effects are so widespread throughout the body, it can also cause dysautonomia, which means you may experience any number of these symptoms, too:
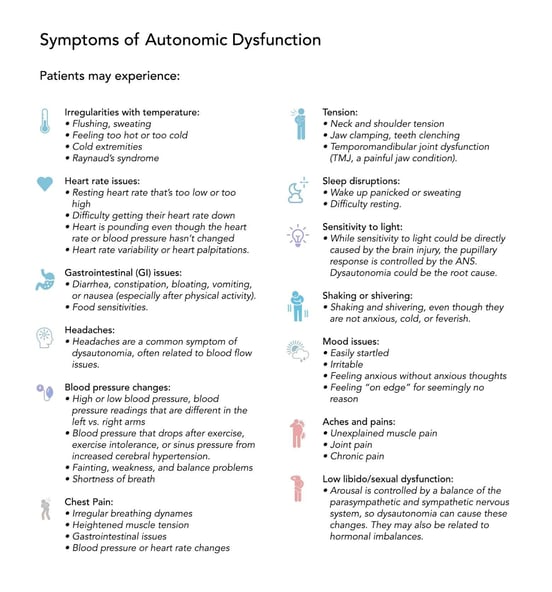 While less common, you might also notice symptoms of vestibular dysfunction such as dizziness, nausea, motion sickness, and balance problems.
While less common, you might also notice symptoms of vestibular dysfunction such as dizziness, nausea, motion sickness, and balance problems.
The long and short term effects of chemotherapy may be different in men and women. Peripheral neuropathy is a more common side effect of chemotherapy in men, whereas symptoms such as vomiting, nausea, diarrhea, and hair loss are more common in women. Therefore, the chemo brain symptoms you experience may be different based on your sex.
Head Injuries and Chemotherapy Treatment
Most of the patients we’ve seen and treated for chemo brain also had a brain injury. Either they had a concussion (or multiple concussions) and then were treated for cancer, or they were treated for cancer and later had a head injury. The reality is that most of us have had at least one head injury. And even if it seemed inconsequential at the time, it might predispose you to long-term cognitive dysfunction from another stressor, such as chemotherapy.
In each of our patients, chemotherapy either caused new symptoms to emerge or increased the severity of their pre-existing symptoms. But in all cases, those symptoms resolved or were greatly reduced after treatment. This resolution in symptoms was accompanied by improved functional MRI scan results. As a result, we are confident that the same treatment we provide for other brain injury patients works for chemo brain as well, since the symptoms all stem from the same source: neurovascular coupling dysfunction.
Is Chemo Brain Permanent?

Chemo brain may resolve on its own a few months after you finish chemotherapy, or it might stretch on for years, if left untreated. Chemo brain has been studied the most in breast cancer survivors. We don’t know if they’re more likely to get it, or if it simply appears that way because of the number of studies done on that patient population.
If your cognitive problems and other symptoms persist six months after you stop chemotherapy, you may want to seek treatment. If you still have chemo brain twelve months after ending cancer treatment, we strongly recommend seeking medical assistance. You can always start treatment for chemo brain earlier if you’re eager to feel better sooner.
While you’re waiting, we recommend that you try some at-home strategies (covered below). If you’re checking all the boxes and it’s still not helping, you may want to come in for treatment sooner than twelve months out.
If you’re relying on compensatory behaviors (such as writing lists for everything), that’s a sign of functional brain change; it’s not healthy to rely on coping mechanisms indefinitely. It’s better to receive treatment and get your brain working better. Different types of chemotherapy have different average recovery times for chemo brain, so you can ask your doctor about your specific situation.
All that said, will you return to 100% of your normal, pre-chemo self? It’s hard to say. Chemo takes a big toll on your system. While your brain has neuroplasticity working in its favor, certain cells will not grow back if damaged during chemotherapy. There are no guarantees for how much you’ll recover.
That said, most people make significant progress with a good treatment program. Their symptoms decline, their quality of life improves, and they have the tools to fight off additional cognitive decline down the road. While your body may never be quite the same, you survived cancer. And that’s a beautiful thing.
Treatment for Chemo Brain
In this section, we cover two aspects of treatment: What you’ll do in our clinic, and what you can do at home to facilitate your recovery.
Treatment for Chemo Brain at Cognitive FX

Cognitive rehabilitation is one of the treatment options mentioned by the American Cancer Society (ACS). But many cognitive rehabilitation programs are not designed to resolve neurovascular coupling dysfunction, and most aren’t tailored to your unique brain injury.
At Cognitive FX, we offer a robust treatment protocol for “invisible” brain injuries such as chemo brain, post-concussion syndrome, carbon monoxide poisoning, bacterial and viral disease (even COVID), and more. We’ve successfully treated patients from around the United States and across the world.
95% of patients who complete our Enhanced Performance in Cognition (EPIC) Treatment program show statistically verified improvement of their brain function. The average patient improvement after one week of treatment is 77.5%.
We know this because each patient undergoes brain imaging before and after treatment. Chemo brain shows up on an fMRI if you have the right data and analytics. We use a testing regimen known as fNCI: functional neurocognitive imaging. From that imaging, we learn which brain regions were affected by your injury so we can tailor your treatment to what you need.
Most healthcare professionals don’t know how your brain, specifically, was affected by chemo. So they string together some cognitive therapy exercises and hope you improve. Instead, we use proven, multidisciplinary therapies that encourage neuroplasticity (your brain’s ability to change and heal) so you can start feeling better.
Our treatment team includes a neuropsychologist, a neuroscientist, a neuroradiologist, a psychologist, neuromuscular therapists, neurocognitive therapists, neurological occupational therapists, and others. All of these specialists work together to create an intense, individualized treatment regimen based on your fNCI results, physical evaluations, and the specific symptoms you report.
You’ll do some combination of neuromuscular therapy, cognitive therapy, occupational therapy, sensorimotor therapy, vestibular therapy, and more.
Here’s an example of an exercise that challenged one of our patients, Sam Pembleton:
“It was an hour-long therapy, and it was just one-on-one with someone. You’d do a cognitive activity, like sorting through a deck of cards, but at the same time someone would give you a four-letter sentence and you'd have to arrange it alphabetically while you were still sorting through the cards. It was a lot of multitasking!”
That multitasking was challenging Sam’s brain to use the hypoactive brain regions instead of relying entirely on healthier ones to improve her cognitive functioning.
Aimee, one of our patients, completes a Dynavision exercise.
Another example is using the Dynavision board to hit lights as they appear in varying patterns and speeds. Dynavision therapy helps with your brain’s processing speed, quick response times, hand-eye coordination, and more.
In addition to cognitive and physical therapies, patients learn mindfulness and good breathing techniques. These help calm your autonomic nervous system and give your brain a chance to decompress.
Our patients also meet with our psychologist at least twice during their treatment. She evaluates any emotional symptoms you’re experiencing and makes recommendations for further treatment, if needed.
Exercises You Can Do at Home
There are steps you can take to feel better while you’re at home, too. This includes:
Order matters in this case. We recommend following the prepare, activate, rest cycle: physical exercise to boost the blood to your brain, followed by at least fifteen minutes of cognitive exertion, then ten to fifteen minutes of quiet rest (meditation or Brainwaves and measured breathing).
A Few More To-Do’s to Feel Better

Two more often-overlooked factors could play into how you’re feeling after chemotherapy: hormones and functional vision changes.
If you haven’t gotten your hormone levels checked since you finished chemo, talk to your doctor and ask for hormone testing. Suboptimal hormone levels could contribute to your symptoms.
In addition, we recommend you get evaluated for functional vision changes. Seeing 20/20 is just the beginning of healthy eyesight! Many people don’t know that their cognitive symptoms (such as headaches or even “chemo fog”) could be related to issues like eye teaming, eye tracking, peripheral vision changes, and more.
Finally, if you’re not sure if your symptoms are from chemo brain but want to learn more, schedule a consultation with our team. We’ll take a look at your symptoms and medical history, then advise you on the next steps in your recovery.



 While less common, you might also notice symptoms of vestibular dysfunction such as dizziness, nausea, motion sickness, and balance problems.
While less common, you might also notice symptoms of vestibular dysfunction such as dizziness, nausea, motion sickness, and balance problems.