If you're reading this, you probably know the feeling. You walk into a room and forget why. You search for words that used to come easily. You feel like you're thinking through mud, and no amount of sleep seems to help.
Maybe your doctor ran tests and told you everything looks "normal." Maybe well-meaning friends have suggested you just need more rest. But you know something changed after COVID, and you want answers.
Here's what we can tell you with certainty: post-COVID brain fog is real, it's measurable, and for most people, it's treatable. Research published in 2024 and 2025 has finally uncovered why COVID affects the brain the way it does—and that understanding is leading to better treatment options.
At Cognitive FX, we've treated hundreds of long COVID patients using the same approach that's helped over 1,000 concussion patients annually for more than a decade. Why? Because the brain dysfunction looks remarkably similar. And our outcomes reflect that: 77% of patients achieve meaningful symptom improvement, validated by independent researchers.
What Causes Brain Fog After COVID? The 2025 Science
For years, researchers debated whether long COVID symptoms were "real" or psychological. That debate is over. Multiple studies using advanced brain imaging have documented exactly what's happening inside the brains of people with persistent cognitive symptoms.
Your Blood-Brain Barrier May Be Compromised
One of the most significant discoveries came from a 2024 study published in Nature Neuroscience. Researchers used specialized MRI scans to examine the blood-brain barrier (BBB) in long COVID patients with brain fog.
What they found was striking: the protective barrier that normally keeps inflammatory substances out of the brain was leaking. This wasn't subtle damage visible only with the most sensitive equipment. It was measurable disruption, particularly in the temporal lobes and frontal cortex—regions critical for memory, attention, and executive function.
Even more concerning, this barrier dysfunction persisted for up to a year after the initial infection. The researchers also identified a specific inflammatory marker called TGFβ that was significantly elevated in patients with brain fog and correlated directly with the degree of barrier leakage.
Blood Clots Are Driving Brain Inflammation
A paradigm-shifting study published in Nature in 2024 revealed that abnormal blood clotting plays a central role in COVID's effects on the brain—not as a secondary consequence, but as a primary driver of damage.
The SARS-CoV-2 spike protein directly binds to fibrin (a clotting protein), creating structurally abnormal clots with enhanced inflammatory properties. These abnormal clots activate toxic responses in brain immune cells called microglia, triggering neuroinflammation that can persist long after the virus itself is cleared.
This discovery is so significant that a fibrin-targeting treatment is now in Phase 1 clinical trials.
Your Autonomic Nervous System May Be Dysregulated
If you've noticed your heart racing when you stand up, extreme fatigue after minimal exertion, or symptoms that seem to come and go unpredictably, your autonomic nervous system may be involved.
Research published in Circulation: Arrhythmia and Electrophysiology found that approximately 31% of highly symptomatic long COVID patients meet the diagnostic criteria for POTS (Postural Orthostatic Tachycardia Syndrome). This autonomic dysfunction directly affects blood flow to the brain, contributing to cognitive symptoms.
The connection makes sense: when your body can't properly regulate blood pressure and heart rate, your brain doesn't receive consistent oxygen and nutrient delivery. The result feels like brain fog because, at a physiological level, your brain isn't getting what it needs to function optimally.
Neuroinflammation Can Persist for Years
Studies using PET scans designed to detect brain inflammation have found evidence of ongoing inflammatory activity more than two years after COVID infection in some patients. This sustained microglial activation releases pro-inflammatory cytokines that interfere with normal brain function.
One particularly striking finding: researchers detected brain temperature increases of up to 1.75°C in olfactory and cognitive regions of long COVID patients. Your brain is literally running hot.

Why Standard Treatments Often Don't Work
If you've tried cognitive rehabilitation programs, brain training apps, or other commonly recommended treatments without much success, you're not alone. In November 2025, the NIH released results from the RECOVER-NEURO trial, the largest study to date examining treatments for long COVID cognitive symptoms.
The findings were disappointing for many patients: none of the tested interventions—including computerized cognitive training (BrainHQ), standard cognitive rehabilitation (PASC-CoRE), or brain stimulation combined with cognitive training—showed any benefit over the comparison groups.
All groups improved modestly over time, but no specific treatment outperformed the others. Standard approaches to cognitive rehabilitation simply didn't move the needle.
This doesn't mean treatment is hopeless. It means that isolated, single-modality approaches aren't enough for a condition affecting multiple brain systems simultaneously.
The brain fog caused by COVID doesn't respond to brain training apps for the same reason a sprained ankle doesn't heal from watching videos about walking. The underlying dysfunction needs to be addressed directly.
Can COVID-19 Cause Brain Fog?

One of the most common neurological symptoms reported by long COVID patients is "brain fog," with some studies suggesting that as many as 80% of patients experience ongoing issues with memory and fuzzy thinking.
Some patients describe how the fog makes them feel numb, as if an impenetrable haze blocks access to their thoughts. It can affect memory, visual and spatial skills, executive function, multitasking ability, and the ability to process information. When these essential brain functions don’t work properly, it becomes difficult to understand, focus, and even remember simple things. Basically, when brain fog happens, your brain doesn’t serve you as well as you would expect.
We've all experienced it at some point — perhaps from jet lag making your thoughts sluggish as if it were 3 AM, or from medication leaving you feeling fuzzy for hours. Whatever the cause, you just had to wait for your brain to return to normal.
For many COVID-19 long haulers, however, this fog is permanent and much more serious. Typical complaints include memory problems, difficulty retaining information, trouble finding the right words, and a general feeling of being overwhelmed by the smallest task. These patients didn’t actually experience anything during their COVID-19 infection that could explain this cognitive dysfunction, like a stroke or a seizure. Yet, they’re coming out with a cognitive impairment that can seriously impact their quality of life.
That’s often in addition to other ongoing symptoms like fatigue, breathing issues, poor sleep quality, and more.
How Does COVID-19 Cause Brain Fog?
One of the ways researchers believe COVID-19 causes brain fog is via an inflammatory response in the body that quickly escalates to neuroinflammation in the brain. A study found increased levels of inflammatory cytokines localized in the brain for weeks after COVID-19 infection. In simple terms, cytokines are molecules produced by the immune system that are involved in fighting infections. However, an excessive and uncontrolled inflammatory reaction in the brain interferes with communication between nerve cells and may contribute to brain fog.
A second explanation involves restricted blood flow to the brain as a result of general hypoxia due to breathing problems. In fact, one of the first imaging-based studies of neurological injury in COVID-19 patients found the same metabolic disturbances in both the brains of long COVID patients and those who had suffered oxygen deprivation.
This restricted blood flow to the brain disrupts the connection between nerve cells and the blood vessels that supply them — known as neurovascular coupling (NVC) — and hinders the distribution of oxygen and energy to the areas of the brain that need it. This is known as neurovascular coupling dysfunction, and it’s one of the leading causes of lingering symptoms — like COVID-19 brain fog — after the virus is gone. It’s also one of the main mechanisms behind lingering symptoms from traumatic brain injury (TBI).
A third possible cause involves dysfunction of the autonomic nervous system (ANS), which is another overlap between long COVID and TBIs. In a healthy person, the ANS regularly sends messages from the brain to the heart, bowel, stomach, and other organs to either speed them up or slow them down, depending on what’s needed. This is done with the help of the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), which have opposing roles. The SNS, which is considered the “fight or flight” system, is characterized by quick responses mobilizing the body for action, while the PNS is the “rest and digest” part, which controls how the body slows down and returns to normal.
However, in long COVID patients, the sympathetic nervous system is often overactive, making it harder to regulate how the body adapts to each situation. For example, a study showed that long-haulers had a lower SNS response when they had to suddenly plunge their hands in icy water compared to healthy individuals, but SNS activity remained high when patients were resting (as opposed to returning to normal quickly, as it should).
Finally, some patients may develop brain fog indirectly as a consequence of other symptoms also caused by long COVID, like vision problems.
Eye specialists are starting to notice that many patients who have seemingly recovered from COVID-19 are now beginning to develop eye-related complications. While some people experience symptoms like blurry vision and conjunctivitis while they are still ill with the virus, the impact of COVID-19 on vision seems to last a lot longer.
For example, one of the health conditions that plagues long COVID patients is retinopathy, where the blood supply to the retina is blocked, or at least restricted, causing blurred vision. This, in turn, causes brain fatigue for these patients, which may end up revealing itself as brain fog, fatigue, feelings of overwhelm, forgetfulness, and more.
Treatment for COVID Brain Fog

A Different Approach: Treating the Underlying Brain Dysfunction
At Cognitive FX, we've spent over 15 years treating patients with persistent cognitive symptoms after concussion. When we began seeing long COVID patients, we noticed something immediately: the patterns of brain dysfunction looked remarkably similar.
This wasn't just our clinical observation. A 2024 University of Denver study tested concussion assessment tools on long COVID patients and found significant deficits matching traumatic brain injury patterns. The researchers concluded that long COVID patients had "effectively experienced a traumatic injury to the brain."
A comprehensive review published in the International Journal of Molecular Sciences in 2025 made the connection explicit, stating that rehabilitation strategies developed for post-traumatic brain injury could be adapted for long COVID.
This overlap isn't coincidental. Both conditions involve:
- Neurovascular coupling dysfunction: The brain's ability to direct blood flow to active regions becomes impaired
- Blood-brain barrier disruption: Though triggered differently, the downstream effects are similar
- Neuroinflammation: Microglial activation and cytokine release affect brain function
- Autonomic dysregulation: The nervous system struggles to maintain proper balance
- Similar patterns on functional brain imaging: Disrupted connectivity networks, particularly involving the default mode network
How Our Treatment Works
Our approach differs fundamentally from what was tested in the RECOVER-NEURO trial. Rather than relying on a single type of therapy delivered over weeks or months, we use functional neuroimaging to identify exactly which brain regions and systems are affected, then deliver intensive, multidisciplinary treatment targeting those specific areas.
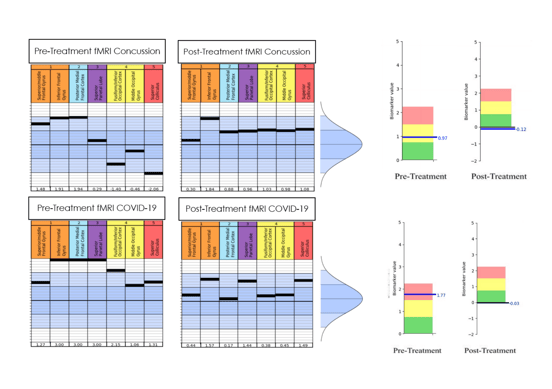
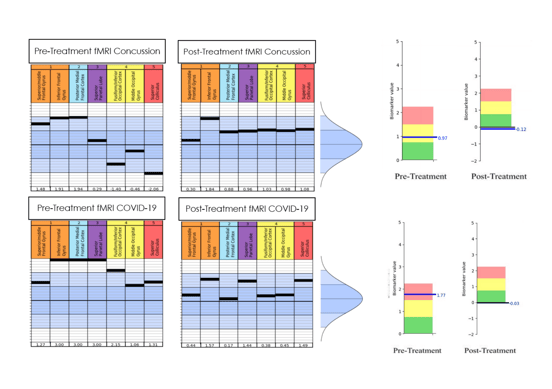
Functional NeuroCognitive Imaging (fNCI): Before treatment begins, you'll undergo our proprietary brain scan that measures how 100+ regions of your brain activate and communicate during cognitive tasks. This isn't a structural MRI looking for visible damage—it's a functional assessment that reveals the patterns of dysfunction causing your symptoms.
The scan takes about 45 minutes and provides a detailed map of your brain function compared to healthy controls. This information guides every aspect of your treatment plan.
EPIC Treatment (Enhanced Performance in Cognition): Our one-week intensive program combines multiple evidence-based therapies delivered by a multidisciplinary team:
- Neuromuscular therapy to address physical tension patterns affecting brain blood flow
- Cognitive therapy targeting specific areas of dysfunction identified on your scan
- Vestibular and balance training to restore sensory integration
- Autonomic regulation exercises particularly important for long COVID patients
- Cardiovascular exercise carefully calibrated to improve brain blood flow without triggering post-exertional symptoms
- Vision and occupational therapy addressing the visual processing issues common in both PCS and long COVID
Throughout the week, therapists continuously adjust your program based on how you're responding. This isn't a one-size-fits-all protocol—it's precision medicine for your brain.
Our Outcomes
We measure what matters: whether patients actually get better.
In our post-concussion syndrome patients, 77% achieve meaningful symptom improvement after one week of treatment. This outcome has been validated by independent researchers, not just our internal data.
For long COVID patients specifically, 60% report improvement in brain fog symptoms. While we're continuing to refine our protocols for this population, these results compare favorably to what's been achieved elsewhere—particularly given that the NIH's large-scale trial found no differential benefit from standard cognitive rehabilitation approaches.

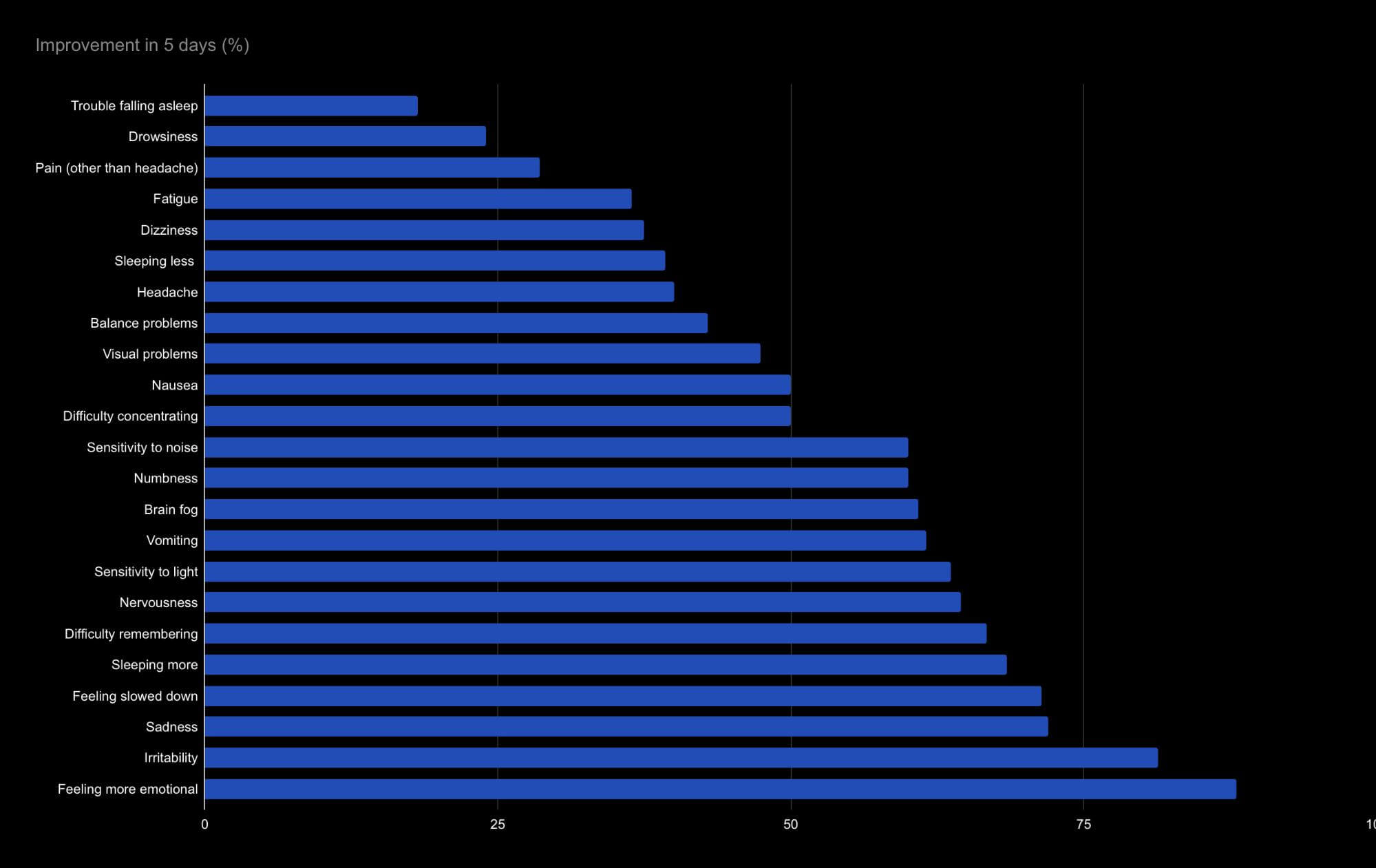
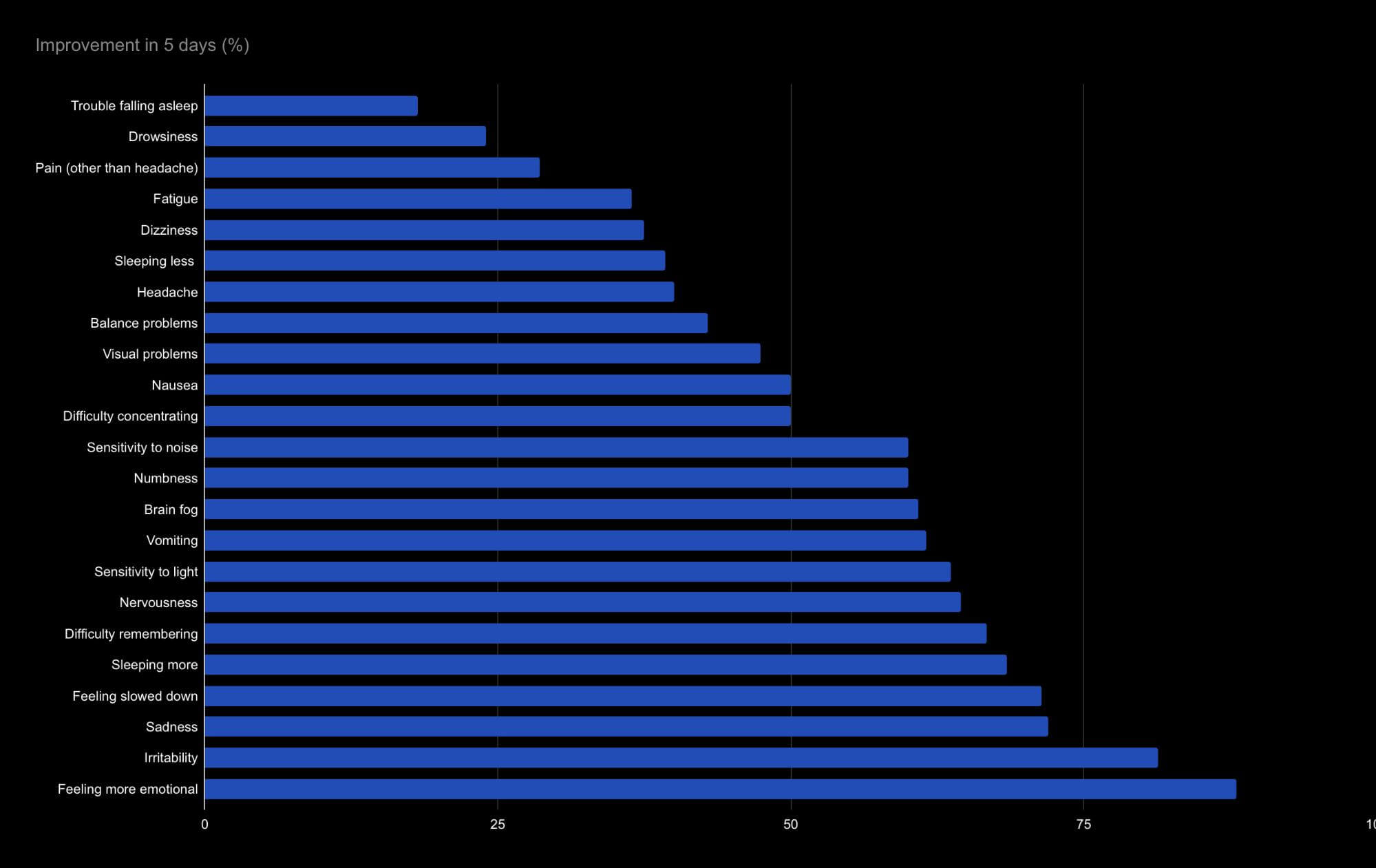
On the last day of treatment, patients undergo a second scan to see how much their brains changed. The average improvement on the second brain scan is currently 112%. Self-reported symptom improvements after one week vary widely, from an almost 90% improvement in emotional symptoms to less than 20% improvement in falling asleep.
On average, long haulers saw their symptoms reduced by half after a week of treatment. Neurological and cognitive symptoms, such as sadness and difficulty remembering, seem to improve more quickly than physical symptoms, such as drowsiness and headaches. However, we’ve only treated 17 patients and we need more data to draw any significant conclusions.
In terms of brain fog, patients experienced a 60% improvement, which is likely to significantly impact their quality of life, allowing for more clear thinking and better memory.
Our sister clinic, Neural Effects, has also successfully treated patients with COVID-19, but their treatment is designed to be more immediate, typically between 4 and 12 weeks after the initial infection, when patients still have symptoms. Treatment includes breathing exercises combined with physical and cognitive therapy, which helped these patients achieve a full recovery.
To discuss your specific symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
What Does Recovery Actually Look Like?
Setting realistic expectations matters. Here's what research tells us about recovery timelines:
Early recovery (within 3 months): A large German study published in Scientific Reports found that 48% of long COVID patients become symptom-free within the first 12 weeks. If you're still experiencing significant symptoms beyond this window, targeted treatment becomes more important.
Typical recovery timeline: Most patients who recover do so within 6-18 months. However, "recovery" doesn't always mean complete resolution—many patients experience meaningful improvement that allows them to return to normal activities even if some residual symptoms remain.
Chronic symptoms: The RECOVER cohort study published in Nature Communications in 2025 found that about 5% of long COVID patients maintain persistently high symptom burden, while another 12% experience non-resolving, intermittent symptoms. Perhaps most concerning, 14% actually had increasing symptoms at 15-month follow-up.
What predicts better outcomes:
- More recent infection (symptoms present for less time)
- COVID-19 vaccination
- Paxlovid treatment within 5 days of acute infection
- Younger age
- Less severe initial infection
What predicts more challenging recovery:
- Symptoms lasting more than 2 years
- ICU admission during acute COVID
- Multiple concurrent health conditions
- Female sex (possibly due to autoimmune factors)
The key message: earlier intervention generally leads to better outcomes. If you've been waiting for symptoms to resolve on their own and they haven't after several months, seeking treatment makes sense.
Other Treatments Showing Promise
While our intensive multidisciplinary approach addresses the underlying brain dysfunction, other treatments may complement recovery or help manage specific symptoms. Here's what current research supports:
Hyperbaric Oxygen Therapy (HBOT)
HBOT has accumulated the strongest randomized controlled trial evidence for long COVID cognitive symptoms. A study published in Scientific Reports found significant improvements in global cognitive function, attention, and executive function after 40 daily sessions at 2.0 atmospheres of pressure.
Importantly, brain imaging confirmed the mechanism: increased cerebral blood flow and improved white matter integrity. A one-year follow-up study found that improvements were maintained over time.
HBOT requires specialized facilities and significant time commitment (40 sessions over 8 weeks is typical), but the evidence supporting its effectiveness is solid.
Treatments for Autonomic Dysfunction
If you have POTS or other autonomic symptoms, specific medications can help:
- Midodrine: 78% efficacy rate in systematic reviews
- Ivabradine: 75% efficacy rate
- Beta-blockers: 64% efficacy rate
The NIH's RECOVER-AUTONOMIC trial is currently testing IVIG, Ivabradine, and coordinated non-drug care, with results expected in 2026.
Stellate Ganglion Block
This procedure, which involves injecting local anesthetic near a nerve cluster in the neck, has shown rapid results in smaller studies. One study found 86% of patients reported symptom reduction, with brain fog relief occurring within 15 minutes to 24 hours in 80% of symptomatic patients.
While more research is needed, this option may be worth discussing with your physician if other approaches haven't helped.
What Hasn't Worked
Extended Paxlovid courses: Two major trials (STOP-PASC at Stanford and PAX LC at Yale) found that 15-day Paxlovid courses did not improve established long COVID symptoms. Paxlovid appears helpful only when given within the first 5 days of acute infection.
Standard cognitive rehabilitation alone: As the RECOVER-NEURO trial demonstrated, computerized brain training and conventional cognitive rehab don't produce differential benefit compared to active comparators. Isolated, single-modality approaches aren't enough.
What Can I Do at Home?

Life with long COVID can be challenging, but there are some things you can do at home to help your recovery:
Practice breathing exercises
We cannot overstate the importance of practicing breathing exercises during recovery. We’ve seen patients go through cognitive therapy and simply forget to breathe because they’re concentrating on something else. Practicing diaphragmatic breathing can help decrease pain, muscle tension, and other physical and cognitive deficits. If you practice this type of breathing at home regularly, you will feel the benefits in your daily life.
Follow good sleep patterns
One bad night is not going to have a major impact, but recurrent sleep deprivation can make your brain fog worse. Aim for at least eight hours of sleep every night, but you may find that you need more to feel better. You can find some more tips about how to train your brain to sleep after brain damage here.
Eat a brain-friendly diet
Not eating a balanced diet can make it difficult for your brain to focus. Diets rich in sugar, saturated fats, or high in calories are harmful to neural function because they increase levels of oxidative stress and hinder cognitive functions.
In contrast, certain foods are rich in nutrients that can actually help your brain operate smoothly. These include, for example, omega-3 fatty acids, which are essential to support nerve cell function and can play a role in maintaining brain health throughout your life.
Pick healthy options rich in omega-3 fatty acids to include in your diet, such as fish, beans, and nuts, and avoid caffeine, alcohol, and processed foods. You can learn more about nutrition for an injured brain here.
Play brain games
The phrase “use it or lose it” really does apply to your brain. Find the time to play brain games, ideally with a memory element. If you don’t like games, try learning a new skill. As long as it’s an enjoyable process and not stressful, it can give your brain a much-needed boost while you recover from the effects of COVID-19. Here are 17 cognitive exercises you can try.
Keep moving
If you have other symptoms alongside brain fog, you may find it hard to be active. However, even gentle exercise can help your recovery. If you can’t go for a run, then go for a walk, but try to move regularly.
Pace yourself
If you find that everyday tasks leave you breathless, tired, and even “foggier” than you started, don’t try to achieve them all at the same time. Instead, break these activities into smaller chunks to do as and when you can. Make sure you take frequent breaks before you become exhausted.
Stay motivated
Think about what you would like to do and set small, achievable goals to get there. Some days will be better than others, but don’t feel discouraged. Always celebrate your successes, no matter how small.
Connect with your friends and family
Whether it’s in person, by phone, or email, don’t lose touch with friends and family. Connecting with other people can make you feel better and keep your brain engaged.
See a mental health professional
If you have any severe mood symptoms, we may recommend seeing a cognitive behavioral therapist in addition to other treatment approaches. You can read more about how this therapy helps after a brain injury here.
Frequently Asked Questions

Frequently Asked Questions
How long does brain fog last after COVID?
For most people, brain fog improves within 6-18 months. However, about 17% of patients experience persistent or worsening symptoms beyond this timeframe. Earlier treatment intervention is associated with better outcomes.
Can brain fog from COVID be permanent?
While some patients do experience very long-lasting symptoms, most improve over time, especially with appropriate treatment. Research shows that the brain changes associated with long COVID are often functional rather than structural, meaning they represent altered patterns of activity rather than permanent damage.
Is long COVID brain fog the same as "chemo brain" or post-concussion syndrome?
There are striking similarities. All three conditions involve neuroinflammation, blood-brain barrier dysfunction, and disrupted neurovascular coupling. This is why treatments developed for post-concussion syndrome can be effective for long COVID. The underlying brain dysfunction patterns overlap significantly, even though the initial triggers differ.
Will my doctor's tests show anything wrong?
Standard medical tests (blood work, structural MRI) are often normal in long COVID patients, which can be frustrating. Functional brain imaging reveals the patterns of dysfunction causing symptoms. At Cognitive FX, our fNCI scan measures how brain regions activate and communicate during cognitive tasks, identifying abnormalities that structural scans miss.
Can I get long COVID more than once?
Yes, reinfection can trigger new or worsening long COVID symptoms. Vaccination reduces this risk but doesn't eliminate it entirely.
Does insurance cover treatment?
Coverage varies by insurance plan and treatment type. Our team can help you understand your coverage options and discuss financing alternatives if needed.
Take the Next Step
Living with brain fog is exhausting. Simple tasks require enormous effort. You may have started doubting your own capabilities or worrying about your future.
But here's what the science now shows clearly: post-COVID brain fog has identifiable, measurable causes. The brain dysfunction is real, and for most people, it's treatable.
At Cognitive FX, we've successfully treated brain fog caused by concussion for over 15 years. The long COVID patients we see have remarkably similar patterns of brain dysfunction, and they respond to the same intensive, imaging-guided treatment approach.
Our EPIC treatment program takes just one week. You'll start with a comprehensive brain scan that shows exactly what's happening in your brain, then receive personalized treatment from a multidisciplinary team targeting your specific areas of dysfunction.
77% of patients improve. You could be one of them.
[Schedule Your Free Consultation]
Questions? Call us at (385) 446-4158 or email info@cognitivefxusa.com. We're available Monday through Friday, 9am-5pm Mountain Time.
References
- Greene C, et al. Blood-brain barrier disruption and sustained systemic inflammation in individuals with long COVID-associated cognitive impairment. Nature Neuroscience. 2024;27(3):421-432. doi:10.1038/s41593-024-01576-9
- Ryu JK, et al. Fibrin drives thromboinflammation and neuropathology in COVID-19. Nature. 2024. doi:10.1038/s41586-024-07873-4
- Popa E, et al. The molecular mechanisms of cognitive dysfunction in long COVID: A narrative review. International Journal of Molecular Sciences. 2025;26(11):5102. doi:10.3390/ijms26115102
- Gundersen H, et al. Prevalence and clinical impact of postural orthostatic tachycardia syndrome in highly symptomatic long COVID. Circulation: Arrhythmia and Electrophysiology. 2024. doi:10.1161/CIRCEP.124.013629
- Szögi T, et al. Novel biomarkers of mitochondrial dysfunction in long COVID patients. GeroScience. 2025;47(2):2245-2261. doi:10.1007/s11357-024-01398-4
- Knopman DS, et al. Evaluation of interventions for cognitive symptoms in long COVID: A randomized clinical trial (RECOVER-NEURO). JAMA Neurology. 2025.
- Zilberman-Itskovich S, et al. Hyperbaric oxygen therapy improves neurocognitive functions and symptoms of post-COVID condition: Randomized controlled trial. Scientific Reports. 2022. doi:10.1038/s41598-022-15565-0
- Hadanny A, et al. Long-term outcomes of hyperbaric oxygen therapy in post-COVID condition. Scientific Reports. 2024. doi:10.1038/s41598-024-53091-3
- Diexer S, et al. Insights into early recovery from long COVID—results from the German DigiHero Cohort. Scientific Reports. 2024;14:8569. doi:10.1038/s41598-024-59122-3
- Mavroudis I, et al. Post-COVID-19 syndrome and post-concussion syndrome: Similarities and differences. Biomedicines. 2024;12(7):1587. doi:10.3390/biomedicines12071587
- RECOVER-Adult Cohort. Long COVID trajectories in the prospectively followed RECOVER-Adult US cohort. Nature Communications. 2025;16:9557.
- Kesler SR, et al. Brain network connectivity in long COVID. Scientific Reports. 2024. doi:10.1038/s41598-024-73311-0
- Douaud G, et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature. 2022. doi:10.1038/s41586-022-04569-5
- Duricka D, Liu L. Stellate ganglion block for long COVID symptoms. Autonomic Neuroscience. 2024. doi:10.1016/j.autneu.2024.103195
- Uswatte G, et al. Constraint-induced cognitive therapy for long COVID brain fog. Rehabilitation Psychology. 2025. doi:10.1037/rep0000626