3-Day fMRI Guided TMS Treatment Shows Results for Chronic Post-Concussion Syndrome


Cognitive FX pioneers accelerated TMS protocol that reduces concussion symptoms by 63% in just three days
The Hidden Epidemic: When Concussion Symptoms Won't Go Away
If you're reading this, you likely know the frustration firsthand. The headaches that won't quit. The brain fog that makes work impossible. The exhaustion that sleep doesn't fix. The anxiety and depression that weren't there before your injury.
You've been told these symptoms should resolve within weeks or months. But for 10-15% of people with mild traumatic brain injury (mTBI), symptoms persist for months or even years—a condition known as post-concussion syndrome (PCS).
Traditional treatments often fall short. Physical therapy helps some symptoms but not others. Medications manage individual complaints without addressing the root cause. Cognitive rehabilitation teaches coping strategies but doesn't restore normal brain function. Many patients cycle through multiple specialists, spending thousands of dollars and months of their lives, only to see minimal improvement.
Until now, few treatments have directly targeted the underlying brain network dysfunctions that cause persistent concussion symptoms.
COGNITIVE FX
Functional Brain Imaging & Treatment
🧠 Accelerated TMS for Post-Concussion Syndrome
Groundbreaking Research Results from Cognitive FX
Post-Concussion Symptom Scale (PCSS) Results
Lower scores indicate fewer/less severe symptoms. Average improvement of 63% maintained at follow-up.
Depression Symptoms (BDI)
34% reduction in depression symptoms
Anxiety Symptoms (BAI)
60% reduction in anxiety symptoms
Objective Brain Function Improvements
These objective measurements show actual changes in brain function, not just symptom relief. All participants showed improvement regardless of symptom severity.
Treatment Outcomes: Percentage Improvement
Study Demographics
Symptom Trajectory: All Measures Combined
Study Methodology
- 11 participants with chronic post-concussion syndrome (avg 21 months since injury)
- Accelerated Protocol: 15 sessions over 3 consecutive days (5 sessions/day)
- Personalized Targeting: fMRI-guided identification of optimal stimulation location
- Intermittent Theta Burst: 1,200 pulses per session at 120% motor threshold
- Objective Measures: Task-related fMRI (fNCI) pre and post-treatment
- Follow-up: Assessments immediately post-treatment and 1-4 weeks later
Experience This Breakthrough Treatment
If you're struggling with persistent concussion symptoms, fMRI-guided accelerated TMS may offer the relief you've been seeking.
📞 Call (385) 375-8590 ✉️ Email Us
Cognitive FX
280 W River Park Dr, Ste 110
Provo, UT 84604
www.cognitivefxusa.com
The Breakthrough: fMRI-Guided Accelerated TMS for Post-Concussion Syndrome
Cognitive FX has pioneered a revolutionary approach that's changing outcomes for patients with chronic post-concussion syndrome. Our new research, recently published in medRxiv, demonstrates that a specialized form of transcranial magnetic stimulation (TMS)—delivered using personalized brain imaging and an accelerated protocol—can produce dramatic symptom relief in just three days.
What Makes This Approach Different?
1. Personalized Brain Mapping with fMRI
Unlike standard TMS protocols that use the same brain location for everyone, our approach uses advanced functional MRI (fMRI) scanning to identify the exact treatment target for each patient's unique brain connectivity patterns.
We analyze how your default mode network (DMN), cognitive control network (CCN), and salience network (SN) are functioning—the three brain networks most commonly disrupted after concussion. The fMRI scan reveals:
- Areas of abnormal brain activation during cognitive tasks
- Disrupted connections between brain regions
- Compensatory patterns your brain has developed
This personalized mapping allows us to target the precise location in your dorsolateral prefrontal cortex that will most effectively restore healthy network function.
2. Accelerated Treatment Protocol
Traditional TMS for depression requires daily sessions over 4-6 weeks. Our accelerated intermittent theta burst stimulation (iTBS) protocol compresses treatment into just 3 consecutive days:
- 5 sessions per day
- 30-minute intervals between sessions
- 1,200 magnetic pulses per session (18,000 total)
- Each session lasts only 6 minutes 32 seconds
This intensive approach induces rapid neuroplastic changes—essentially "rebooting" maladaptive brain network patterns that developed after your injury.
3. Theta Burst Stimulation Technology
iTBS delivers magnetic pulses in a specific pattern (short bursts at 50 Hz, repeated at a theta frequency of 5 Hz) designed to promote long-term potentiation—the same process your brain uses for learning and memory. This pattern is particularly effective at:
- Enhancing cortical excitability
- Strengthening healthy neural connections
- Reducing pathological connectivity patterns
- Restoring normal network communication
The Research Results: Dramatic Improvements Across All Measures
Our pilot study followed 11 patients with chronic post-concussion syndrome (average 21 months since injury) who underwent the 3-day accelerated iTBS protocol.
Symptom Improvements
Post-Concussion Symptom Scale (PCSS)
- 63% average symptom reduction immediately after treatment
- Benefits maintained at 1-4 week follow-up (62% reduction)
- 7 out of 8 participants reported >50% symptom relief
- Significant improvement across physical, cognitive, sleep, and emotional symptoms
Beck Anxiety Inventory (BAI)
- 60% reduction in anxiety symptoms at 1-4 week follow-up
- Average score decreased from 22.75 to 8.62
- Improvements persisted beyond the treatment period
Beck Depression Inventory (BDI)
- 34% reduction in depression symptoms immediately after treatment
- Effects maintained at follow-up
- Many patients reported mood improvements continuing to build post-treatment
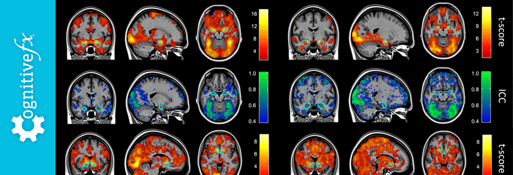
Objective Brain Function Improvements
Perhaps most remarkably, every single patient showed dramatic improvements in objective brain function measures:
Brain Region Activation
- 51.6% improvement in regional brain activation patterns
- Significantly reduced deviation from healthy control standards
- Changes visible on task-related fMRI scans
Functional Connectivity
- 56.9% improvement in inter-region brain connectivity
- Restoration of healthy communication between brain networks
- Normalization of Default Mode Network activity
- Enhanced Cognitive Control Network function
These objective changes provide biological confirmation that the treatment is directly addressing the underlying neural dysfunction—not just masking symptoms.
Why Brain Network Dysfunction Causes Persistent Concussion Symptoms
Understanding the science behind post-concussion syndrome helps explain why this treatment works so effectively.
The Three Critical Brain Networks
Default Mode Network (DMN) After concussion, the DMN often becomes overactive or poorly regulated, contributing to:
- Difficulty concentrating
- Mental fatigue
- Intrusive thoughts
- Cognitive slowness
Cognitive Control Network (CCN) Reduced CCN activity or connectivity leads to:
- Impaired working memory
- Executive function deficits
- Difficulty multitasking
- Slowed information processing
Salience Network (SN) Dysfunction in the SN, particularly involving the anterior cingulate cortex, causes:
- Chronic fatigue
- Emotional dysregulation
- Anxiety and depression
- Difficulty filtering relevant information
How TMS Restores Network Balance
By delivering precisely targeted magnetic stimulation to the dorsolateral prefrontal cortex—a critical hub connecting all three networks—we can:
- Enhance underactive cognitive control functions
- Normalize overactive default mode activity
- Restore healthy network switching via the salience network
- Reduce maladaptive compensatory patterns
The accelerated protocol delivers enough stimulation in a compressed timeframe to induce lasting neuroplastic changes, essentially "resetting" the dysfunctional patterns your brain developed after injury.
What Makes Cognitive FX's Approach Unique?
Functional Neurocognitive Imaging (fNCI)
Beyond just treating symptoms, we provide objective measures of your brain function using our proprietary fNCI protocol. This task-related fMRI assessment:
- Evaluates 62 brain regions during cognitive tasks
- Measures connectivity between 1,891 region pairs
- Compares your results to 270 healthy controls
- Identifies specific areas of dysfunction
- Tracks objective improvements after treatment
No other concussion clinic in the world offers this level of detailed, objective brain function assessment.
Evidence-Based, Research-Driven Care
This latest research builds on Cognitive FX's decade-long commitment to advancing concussion treatment through rigorous scientific investigation. Our team includes:
- Board-certified neurologists
- PhD neuroscientists
- Licensed therapists specializing in brain injury
- Expert TMS technicians
All treatments are guided by peer-reviewed research and continuously refined based on patient outcomes.
Integration with Comprehensive Rehabilitation
While accelerated TMS can produce rapid improvements, we recognize that optimal recovery often requires a multidisciplinary approach. Our treatment programs can include:
- Physical therapy for cervicogenic headaches and balance issues
- Vestibular therapy for dizziness and visual problems
- Cognitive therapy for attention and memory deficits
- Psychotherapy for emotional symptoms
- Neuromuscular therapy for neck dysfunction
The key difference: TMS can restore normal brain network function, making your brain more receptive to these other therapies.
Who Is a Candidate for Accelerated TMS?
Ideal Candidates
You may benefit from fMRI-guided accelerated TMS if you have:
- Persistent symptoms lasting 3+ months after concussion
- Failed standard treatments (physical therapy, medications, cognitive rehab)
- Multiple concussions with cumulative effects
- Comorbid depression or anxiety related to your injury
- Cognitive complaints affecting work or school
- Abnormal fMRI findings showing network dysfunction
Treatment Exclusions
For safety reasons, TMS is not appropriate if you have:
- Metal implants in the skull
- Pacemakers or other electronic implants
- History of seizures or epilepsy
- Active psychosis or severe psychiatric conditions
- Pregnancy (as a precaution)
What About Recent Injuries?
While this study focused on chronic PCS (symptoms lasting months to years), we also treated two patients with acute concussion (<3 months) who showed similar improvements. Earlier intervention may prevent chronic symptoms from developing.
What to Expect: The Treatment Experience
Pre-Treatment Assessment (Day 1)
Morning: Functional MRI Scans
- Resting-state scan to map brain connectivity (30 minutes)
- Task-based fNCI scan to assess brain function (15 minutes)
- T1-weighted structural scan for anatomical precision
Afternoon: Treatment Planning
- Our team analyzes your fMRI data
- We identify your personalized TMS target
- Motor threshold determination (the minimum stimulation intensity needed)
Treatment Days (Days 2-4)
Daily Schedule
- 5 TMS sessions throughout the day
- Each session lasts 6 minutes 32 seconds
- 30-minute rest intervals between sessions
- Total daily time commitment: approximately 3-4 hours
During Treatment
- You'll sit in a comfortable chair
- A magnetic coil is positioned against your scalp
- You'll feel a tapping sensation and hear clicking sounds
- No anesthesia or sedation needed
- You can read, listen to music, or relax between sessions
Common Side Effects (temporary and mild)
- Scalp sensitivity at the stimulation site
- Mild headache (typically resolves within hours)
- Facial muscle fatigue
- Temporary symptom fluctuation during treatment
Important: Nearly all participants in our study reported that any side effects resolved before the next day's treatment session.
Post-Treatment Follow-Up
Immediate Post-Treatment (Day 4 or 5)
- Repeat fNCI scan to measure brain function changes
- Symptom reassessment
- Discussion of results with your treatment team
1-4 Week Follow-Up
- Check-in to assess sustained improvements
- Many patients report continued improvement during this period
- Recommendations for ongoing supportive therapies if needed
Real Results: What Patients Experience
While we can't share individual patient stories without consent, the research data reveals common patterns:
Week 1 (During Treatment)
- Many patients notice improvements after the first day
- Incremental gains with each subsequent treatment day
- Reduced brain fog and improved mental clarity
- Better sleep quality
- Decreased headache frequency or intensity
Weeks 2-4 (Post-Treatment)
- Continued symptom reduction in most patients
- Some patients report delayed improvements (symptoms continue improving after treatment ends)
- Enhanced ability to tolerate cognitive demands
- Reduced anxiety and improved mood
- Greater stamina for work and daily activities
Long-Term (Beyond 1 Month)
- Sustained improvements in brain connectivity on follow-up scans
- Many patients report the treatment "unlocked" their ability to benefit from other therapies
- Objective brain function measures remain significantly improved
The Science Behind Lasting Results
Neuroplasticity and Network Reorganization
The brain's remarkable ability to reorganize itself—neuroplasticity—is both the problem and the solution in chronic PCS.
After concussion, your brain develops compensatory patterns to work around damaged or dysfunctional areas. While initially protective, these patterns can become maladaptive, creating:
- Inefficient neural pathways
- Excessive energy expenditure for basic tasks
- Network hyperconnectivity or hypoconnectivity
- Persistent symptoms even after structural healing
Accelerated iTBS delivers enough concentrated stimulation to overcome these entrenched patterns. By specifically targeting brain regions anti-correlated with the Default Mode Network and positively correlated with the Cognitive Control Network, we:
- Strengthen underactive executive control systems
- Reduce overactive self-referential processing
- Restore healthy network segregation and integration
- Enable more efficient neural processing
The accelerated protocol (multiple sessions per day over consecutive days) produces more robust neuroplastic changes than traditional once-daily treatments, potentially explaining the dramatic results.
Why fMRI Guidance Matters
Research shows significant individual variability in brain organization, especially after injury. What works at one brain location for one person may be suboptimal for another.
Our fMRI-guided approach ensures we're targeting:
- The region with strongest anti-correlation to your specific DMN pattern
- Areas positively connected to cognitive control regions
- Locations that can most effectively modulate your unique network dysfunction
This personalization may explain why 100% of patients in our study showed objective brain improvements, even though symptom patterns varied.
Comparing Treatment Options: Where Accelerated TMS Fits
Traditional Concussion Management
Standard Approach:
- Rest and gradual return to activity
- Symptom-specific medications
- Physical, vestibular, and vision therapy
- Cognitive rehabilitation
- Psychotherapy
Limitations:
- Often palliative rather than restorative
- Doesn't directly address network dysfunction
- Variable efficacy (many patients remain symptomatic)
- Requires months of treatment
- May not work for chronic cases
When it works: Early intervention in acute phase, straightforward symptoms
Conventional TMS for Depression
Protocol:
- Daily sessions for 4-6 weeks
- Targets left DLPFC using standard coordinates
- Primarily for treatment-resistant depression
Limitations for PCS:
- Time-intensive (20-30 sessions)
- Not personalized to brain injury patterns
- Doesn't use fMRI guidance
- Designed for depression, not concussion
When it works: Depression without brain injury
Cognitive FX Accelerated fMRI-Guided TMS
Protocol:
- 3 consecutive days
- 15 total sessions
- Personalized fMRI targeting
- Objective before/after brain measures
Advantages:
- Directly addresses network dysfunction
- Rapid symptom relief (days, not months)
- Personalized to your specific brain patterns
- Objective measures of brain changes
- Well-tolerated with minimal side effects
- Can be combined with our EPIC treatment program
Ideal for: Chronic PCS unresponsive to standard treatment, patients needing rapid improvement
Insurance Coverage and Treatment Investment
Coverage Considerations
TMS is FDA-approved for depression and is increasingly covered by insurance for that indication. Coverage for post-concussion syndrome applications is evolving. We recommend:
- Contacting your insurance provider about TMS coverage
- Asking specifically about coverage for "neuromodulation for traumatic brain injury"
- Obtaining pre-authorization when possible
Our team can provide documentation of medical necessity and assist with insurance navigation.
Investment in Your Recovery
While costs vary based on individual circumstances and insurance coverage, consider:
The Cost of Persistent Symptoms:
- Lost work productivity or inability to work
- Ongoing medications and therapies
- Reduced quality of life
- Impact on relationships and mental health
- Years of symptom management
The Value of Rapid, Objective Improvement:
- Just 3 days of treatment
- Objective brain function measures
- Potential to return to work and normal activities
- Reduced need for ongoing symptom management
- Improved response to other therapies
Many patients find that the potential for dramatic, lasting improvement justifies the investment, especially after unsuccessful standard treatments.
Frequently Asked Questions
How is this different from EPIC treatment?
Our EPIC (Enhanced Performance in Cognition) program is a comprehensive 1-week intensive rehabilitation that includes physical, cognitive, and occupational therapy guided by fMRI results. Accelerated TMS can be:
- A standalone treatment for patients who primarily need network rebalancing
- An addition to EPIC treatment for patients with severe network dysfunction
- A preparatory treatment that makes the brain more responsive to rehabilitation
Your treatment team will recommend the best approach for your specific needs.
Is the improvement permanent?
Our research shows sustained improvements at 1-4 weeks post-treatment. Long-term durability studies are ongoing. Some patients may benefit from occasional booster sessions, while others experience lasting relief. The objective brain changes we measure suggest genuine neuroplastic reorganization, not temporary symptom masking.
Does it hurt?
Most patients describe the sensation as a tapping feeling on the scalp with some facial twitching. It's typically not painful, though scalp sensitivity is common. We adjust intensity to maintain tolerability while delivering therapeutic benefit.
What if I have depression or anxiety from other causes?
TMS is FDA-approved for depression, and many of our patients have both post-concussion syndrome and mood disorders. The treatment may help both conditions, especially when they're neurologically linked.
Can I drive myself to treatment?
Yes. Unlike some brain treatments, TMS doesn't impair your ability to drive or function. Most patients drive themselves to and from sessions.
What happens if it doesn't work for me?
While our research shows significant improvements in the vast majority of patients, individual responses vary. If you don't experience sufficient benefit, we'll:
- Review your fMRI results to understand why
- Consider whether alternative or additional treatments might help
- Provide recommendations for next steps
Our goal is always an optimal outcome, whether that comes from TMS alone or combination approaches with our third party validated EPIC program.
The Future of Concussion Treatment
This research represents a paradigm shift in how we approach persistent post-concussion symptoms.
Directly measure brain network dysfunction with fMRI
Precisely target the neural circuits causing symptoms
Rapidly restore healthy brain function in days
Objectively verify improvements with follow-up imaging
Enable better response to comprehensive rehabilitation
Ongoing Research
Cognitive FX continues to advance the field through:
- Larger randomized controlled trials
- Long-term outcome studies
- Optimization of targeting protocols
- Integration with neurorehabilitation
- Extension to other brain injury populations
We're committed to continually improving outcomes through rigorous scientific investigation.
Take the Next Step: Is Accelerated TMS Right for You?
If you're struggling with persistent concussion symptoms that haven't responded to standard treatment, fMRI-guided accelerated TMS may offer the breakthrough you've been seeking.

About the author
Dr. Mark Allen, Ph.D.Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.