If you’ve undergone TMS therapy and noticed an increase in depressive symptoms, you might worry the treatment wasn’t right for you. Similarly, if you’re considering TMS, you may wonder: Could TMS make my depression worse?
Current research suggests TMS does not increase depression symptoms in most patients. However, some individuals may experience temporary changes or worsening symptoms due to specific factors.
In this article, we cover:
Possible Reasons Depression Symptoms May Worsen During or After TMS Therapy
Research shows that TMS is generally an effective treatment for reducing depression symptoms with minimal side effects. Multiple studies and clinical trials support its positive impact, which we’ll discuss later in this article.
However, while rare, some individuals may experience a temporary worsening of symptoms due to specific factors. It’s important to note that TMS is not suitable for everyone, and in certain cases, it may contribute to symptom fluctuations.
If you feel that TMS is making your depression worse, contact your healthcare provider as soon as possible. They can evaluate your treatment plan and make necessary adjustments to ensure your safety and well-being.
The following are some reasons why TMS symptoms might temporarily worsen during or after therapy:
Magnetic Coil Placed in the Wrong Location
In our view, one of the main reasons some patients experience worsened depression symptoms during TMS therapy is improper coil placement.
During a TMS session, a clinician places an electromagnetic coil over the patient’s head to stimulate the dorsolateral prefrontal cortex (DLPFC) — an area of the brain crucial for mood regulation. Research shows that individuals with depression often have reduced activity in the left DLPFC, an area linked to positivity and motivation. The goal of TMS is to stimulate nerve cells in this region, helping restore normal function and alleviate depressive symptoms.
However, accurately pinpointing the DLPFC can be challenging. The most common targeting method, the 5 cm method, estimates the correct target location by manually measuring head landmarks. While easy to implement, this approach is often imprecise due to individual differences in head size, shape, and brain structure. Even minor misalignments of the coil — by just a few millimeters — can reduce treatment effectiveness and potentially lead to unintended effects.
Newer technologies, like neuronavigation, improve targeting accuracy using brain imaging to guide coil placement. This advancement significantly reduces the risk of imprecise brain stimulation. If you're considering TMS therapy, ask your provider about their targeting methods to ensure optimal results.
Inexperienced Staff
While TMS involves some automated processes, key aspects of treatment require skilled human oversight. Proper coil placement (as discussed earlier) is one factor, but clinicians must also establish precise measurements, such as calculating the motor threshold — the intensity required to trigger a muscle response. This is typically determined by gradually increasing the magnetic pulse until the patient’s thumb twitches. Since motor threshold varies by individual, it directly influences TMS dosage.
Because these measurements rely on human precision, errors can occur — especially when performed by less experienced operators. Research has shown that operator experience significantly impacts treatment accuracy, with beginners more prone to miscalculations. Inaccurate measurements can reduce TMS effectiveness and, in some cases, contribute to worsened symptoms.
To maximize treatment success, it’s essential to receive TMS from a qualified and experienced provider who can accurately assess, monitor, and adjust the treatment as needed. When exploring TMS clinics, don’t hesitate to ask about staff training and certification to ensure you receive the highest standard of care.
TMS Dip
Some TMS patients notice early improvements, only to feel worse a few weeks into treatment. This phenomenon, known as the TMS dip, can feel discouraging — but it’s important to understand that it’s temporary. Experiencing a dip does not mean that TMS is failing or that your depression is untreatable.
For most patients, these symptoms resolve on their own without requiring changes to treatment. After a short period, many people start feeling better again.
This pattern is common in depression treatment. For example, many antidepressant medications initially worsen symptoms before leading to improvement, and TMS can follow a similar course.
If you’re going through a TMS dip, talk to your doctor. In extreme cases, your medical team can adjust your treatment plan and help you manage symptoms. The key is to stay consistent. TMS works best when treatment is completed as prescribed, and most patients recover from the dip with continued sessions.
Underlying Conditions
For patients correctly diagnosed with major depression, TMS is unlikely to worsen symptoms. However, for patients with undiagnosed or misdiagnosed mental health disorders, TMS may appear to worsen depression symptoms when, in reality, it is affecting an underlying issue.
For example, research on TMS in schizophrenia suggests it may improve emotional regulation but worsen symptoms like delusions and hallucinations. Similarly, studies on TMS in bipolar disorder show mixed results, with some findings suggesting it may increase mania or depressive episodes.
To ensure the best possible outcome, it is essential to undergo a thorough psychiatric evaluation before starting TMS. If you’re considering this treatment, speak with a qualified professional to rule out mental health conditions like bipolar disorder or schizophrenia, which may require a different treatment approach. Proper diagnosis and a comprehensive treatment plan are key to ensuring that TMS is safe and effective for you.
High Expectations
In some cases, it’s not TMS itself that worsens symptoms, but the high expectations patients place on the treatment. When results don’t match their expectations — or if they experience a temporary dip — patients may feel discouraged and assume the treatment isn’t working.
However, improvement takes time. Some patients don’t notice significant changes until they complete their full course of treatment. Progress can be gradual, and temporary setbacks are normal. The key is to stay consistent and trust the process — many individuals experience the full benefits of TMS only after completing their sessions.
Relapse After Treatment
Although TMS is effective in reducing symptoms of depression, some patients experience a relapse weeks or months after they complete treatment. Research suggests that up to 80% of patients relapse within 6 months of finishing repetitive transcranial magnetic stimulation (rTMS, the original and most common form of TMS therapy).
Given this high relapse rate, many patients benefit from maintenance TMS sessions and/or psychotherapy, which help extend remission and keep symptoms at bay. If you're considering TMS, talk to your doctor about a long-term care plan to sustain your progress and reduce the risk of relapse.
Note: We’ve also covered whether TMS can increase the risk of developing anxiety symptoms or even anxiety disorders, such as obsessive-compulsive disorder (OCD) or generalized anxiety disorder.
Why Most Patients Don't Need to Worry About TMS Worsening Depression
TMS is an FDA-approved, proven treatment for depression that is both safe and effective. While some patients experience a temporary dip during treatment, there is no evidence that TMS leads to long-term worsening of depression symptoms.
TMS Is an Effective Way to Treat Depression Symptoms
One of the key benefits of TMS is its effectiveness, especially compared to traditional antidepressant medications, which only help about one-third of patients.
Studies show that:
-
rTMS improves symptoms in about 50% of patients, with over 30% achieving remission.
-
Around 30% of patients who haven’t responded to multiple antidepressant medications still respond to treatment, with 19% achieving remission.
-
TMS is particularly effective in patients with mild to moderate depression and non-psychotic depression.
TMS Is a Safe Treatment Option
TMS is widely considered a safe procedure. Side effects are typically mild, temporary, and tend to disappear after a few sessions. Common short-term side effects of TMS include:
- Mild headaches
- Scalp discomfort at the stimulation site
- Facial twitching
- Lightheadedness
Less common side effects include dizziness, tinnitus, muscle twitching, insomnia, and gastrointestinal discomfort.
While seizures are a known risk, they are extremely rare, occurring in less than 0.01% of sessions (fewer than 1 in 10,000). Importantly, there is no evidence that TMS causes long-term memory loss or cognitive impairment.
TMS vs. Other Depression Treatments
Compared to antidepressant medications and electroconvulsive therapy (ECT), for example, TMS has fewer and milder side effects.
-
Antidepressant medications often cause fatigue, anxiety, digestive issues, and sleep disturbances.
-
ECT is associated with memory loss and cognitive side effects.
For many patients, TMS offers a safe, non-invasive alternative with a lower risk of side effects than traditional depression treatments.
SAINT™ TMS: A New TMS Protocol Producing the Best Depression Treatment Outcomes to Date
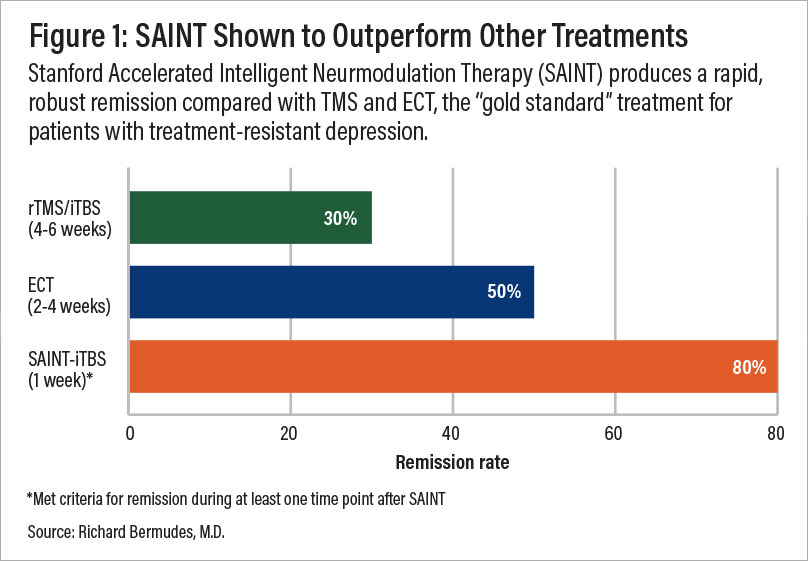
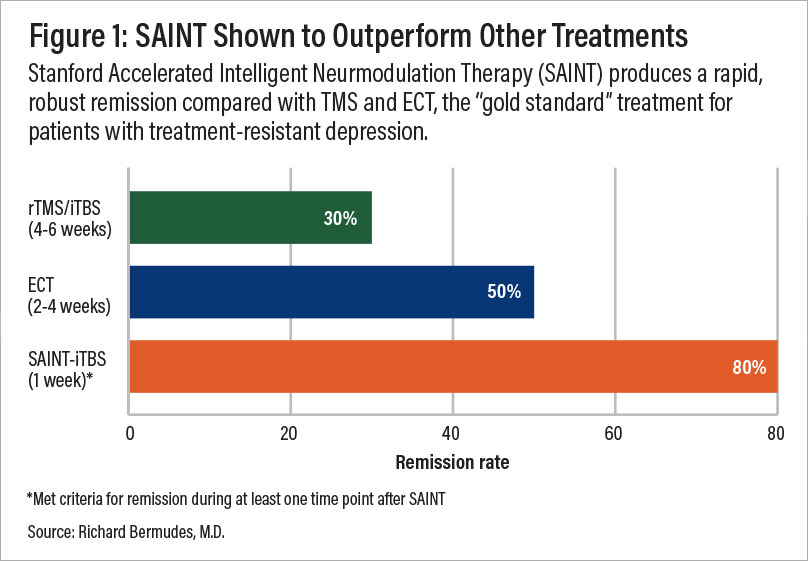
A comparison of remission rates for rTMS/iTBS, electroconvulsive therapy (ECT), and SAINT-iTBS.
TMS technology has evolved significantly, and the latest breakthrough — SAINT TMS (Stanford Intelligent Accelerated Neuromodulation Therapy) — is delivering impressive success rates for treating major depressive disorder (MDD) and treatment-resistant depression. The FDA approved SAINT TMS in 2022, and clinical trials suggest it is the most effective, precise, and efficient TMS protocol available today.
SAINT Is More Effective
While traditional rTMS is more effective than antidepressant medication, the SAINT protocol is proving to be even more successful:
-
90% of patients who didn’t respond to standard TMS achieved remission in just 3–5 days.
-
In a randomized controlled trial, 85% of first-time TMS patients responded, and 78% reached full remission within five days.
-
After four weeks, remission rates remained around 60%, demonstrating lasting benefits.
SAINT Is More Precise
As we’ve discussed, a major challenge with standard TMS is coil placement — even a few millimeters off can reduce effectiveness. Older TMS methods rely on manual head measurements, leading to variability.
-
SAINT eliminates guesswork by using functional MRI (fMRI) to pinpoint the exact brain region needing stimulation.
-
Neuronavigation technology ensures that the magnetic coil is always precisely aligned.
-
This advanced targeting leads to higher response rates and better long-term outcomes.
SAINT Is Faster
Unlike standard rTMS, which requires 40-minute sessions once a day for 4-6 weeks of treatment, SAINT is:
-
Much faster: Using Intermittent Theta-Burst Stimulation (iTBS), each session lasts just 10 minutes. Patients receive 10 treatment sessions per day for 5 days, allowing for rapid improvement.
-
Easier to complete: The one-week SAINT protocol is ideal for patients balancing work, childcare, and other commitments.
Practical Barriers That Impact Access to SAINT™ TMS
While SAINT offers significant advantages over traditional TMS, the following may make it less accessible:
- Lack of insurance coverage: Most insurance plans do not yet cover SAINT, as it is a newer protocol compared to standard TMS. However, coverage policies vary, so it’s important to check with your insurance provider to confirm your options. The Centers for Medicare and Medicaid Services (CMS) have announced that hospitals will be reimbursed $19,703 for the full SAINT protocol, as of July 1, 2025.
- High treatment costs: Currently, SAINT TMS treatments typically range from $30,000 to $36,000, making the cost a significant barrier for many patients. There are, however, close alternatives available at a significantly lower price (discussed below).
- Limited availability: Fewer than 10 clinics in the U.S. currently offer SAINT, with most providers still using rTMS. However, more clinics are beginning to adopt accelerated TMS and intermittent theta burst stimulation (iTBS) protocols, signaling a gradual shift toward newer treatment methods.
Receiving Accelerated fMRI TMS at Cognitive FX: A SAINT™ Alternative for One-Third the Price
Our clinic, based in Provo, Utah, provides an alternative to SAINT™ TMS that offers the same precision of personalized treatment targeting, combined with FDA-approved theta burst stimulation at a significantly lower cost. This approach delivers the same core elements that make SAINT™ so revolutionary.
The only difference between our treatment and SAINT (a trademark licensed to Stanford Medical) is our targeting method. Our target locations are determined by fMRI and our prescribing neuroscientist and physician, rather than their proprietary software.
As we’ve highlighted throughout this article, this protocol of TMS is:
- Safe: Widely tolerated and associated with mild, short-lasting side effects.
- Precise: fMRI ensures that the treatment target area is precisely located for each patient, accounting for variations in head size and shape. Neuronavigation ensures the magnetic coil is placed over that exact spot for every treatment session.
- Fast: Treatment courses are reduced to a single week, making it easier to complete alongside life and work commitments (compared to 4 to 6 weeks of standard TMS and accelerated TMS protocols).
To improve outcomes for our patients, we also include cognitive behavioral therapy (CBT) as a part of our treatment. When combined with the traditional method of TMS (rTMS), CBT improved response and remission rates by ~8% and ~19%, respectively. Additionally, CBT is likely to produce sustained improvement over time once treatment has concluded.
Our brain stimulation treatment is ideal for most patients with treatment-resistant depression. However, we do not treat patients under the age of 18 or over 65. Additionally, as a safety measure, we do not treat patients who have a history of seizures or who are currently actively suicidal and in need of crisis care.
Click here to learn more about receiving accelerated fMRI TMS therapy at Cognitive FX.
Cited Research