More than two years since the COVID-19 pandemic started, the list of symptoms caused by the virus keeps getting longer. In addition to the most common symptoms of a persistent dry cough, fever, and shortness of breath, many patients experience an array of seemingly random body changes both during and after the acute phase of the disease. We’ll discuss a number of them, including but not limited to:
- Skin rashes (including the toe lesions dubbed “COVID toes”)
- Hair loss
- Conjunctivitis (pink eye)
- Gastrointestinal problems
- Heart palpitations
- Loss of smell and taste
- Urinary incontinence
- Weight gain or weight loss
- Development of Type II Diabetes
Scientists are starting to piece together the mechanisms behind these effects, but it is a work in progress. Understanding the mechanisms behind COVID-19 is the only way to anticipate the symptoms it may cause and come up with better ways to treat patients.
At Cognitive FX, we offer a treatment program for some patients experiencing long COVID. While we cannot address all body changes associated with long COVID, we are often able to improve symptoms such as brain fog, sleep disruption, exercise intolerance, fatigue, and more.
In this post, we’ll talk about some of the possible causes of your long-lasting COVID symptoms and body changes, along with specific strategies for improvement in each symptom category. To learn more about our treatment program, skip to the end of this post.
Our treatment program is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 90% of our patients show symptom improvement. Plus, using advanced brain scan techniques, we can see how our patients' brains respond to treatment. Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria as compared to our post-concussion syndrome patients. To discuss your specific COVID-19 symptoms and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
How does COVID cause body changes?
There is still much we don’t know about the new coronavirus. But one thing is clear: COVID-19 can have a wide-ranging effect on the body. It all starts with basic flu symptoms, but for some patients, this disease eventually affects the lungs, heart, kidneys, and other organs. There are multiple ways that the virus can attack different areas of the body:
- Direct attack via the ACE2 receptor
- Inflammation and cytokine storms
- Blood clots
- Autonomic nervous system (ANS) disruption
- Hormone changes
- Microbiome changes
Direct Attack via ACE2 Receptor
The direct route involves a protein called the angiotensin-converting enzyme 2, or ACE2 receptor, for short. When the virus responsible for COVID-19 — the SARS-CoV-2 virus — enters the human body, it binds to this specific protein present on the surface of many cell types.
Although the respiratory system is the first to be attacked, ACE2 is present in many different organs, including the heart, kidneys, liver, and gastrointestinal tract. The SARS-CoV-2 virus can target and infect any organ that has ACE2 receptors, resulting in symptoms.
Inflammation and Cytokine Storms
Once the body recognizes this virus as pathogenic, it triggers a type of cells from the immune system called cytokines. This is a normal mechanism to help the body clear a viral infection. However, if this response is poorly regulated, it can lead to a cytokine storm capable of severely damaging the body’s tissues and organs. In long COVID patients, even after the virus has been completely eliminated from the body, this excessive immune response can remain switched on for months.
Blood Clots
The virus can also cause the formation of small blood clots. It’s still unclear why or how these blood clots develop in patients with COVID-19, but it’s either because of a direct attack on endothelial cells (cells that line the inside of blood vessels) via the ACE2 receptor or a consequence of an exaggerated immune response. These blood clots can be extremely dangerous as they can easily block blood supply to any part of the body. What’s worse, the effects of organ damage can linger and become permanent, even after the virus is eliminated.
Disruption of the Autonomic Nervous System
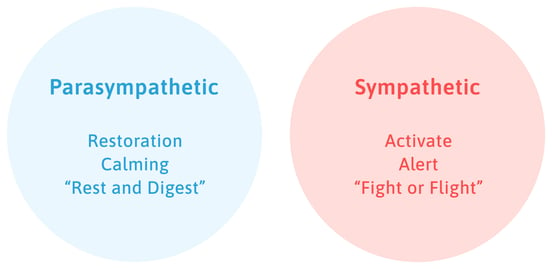
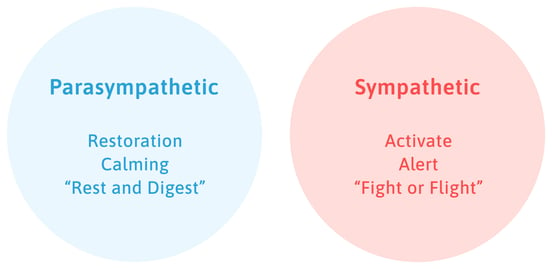
Many of the symptoms experienced after a COVID infection, including heart palpitations and changes in sweat, also indicate that the autonomic nervous system (ANS) is involved.
Two sections of the ANS operate together to regulate many vital functions in the body, including digestion, breathing rates, and blood pressure. They touch nearly every organ in the body. When the body perceives an attack or a threatening situation, the sympathetic nervous system triggers a “fight or flight” response by increasing breathing and heart rate, among other responses. In contrast, the parasympathetic nervous system brings the body back to normal via the “rest and digest” response.
Given the wide range of functions, it’s not surprising that changes in ANS function after a COVID-19 infection can have an impact on many different organs in the body.
Read more about post-COVID autonomic dysfunction here.
Hormone Changes
Many long COVID patients also experience hormonal imbalances. Both directly and indirectly, the SARS-CoV-2 virus can affect multiple endocrine glands in the body, including the…
- Pancreas (which secretes insulin)
- Ovaries and testis (which produce sex hormones such as progesterone and testosterone)
- Adrenal gland (which secretes cortisol)
- Thyroid (which secretes thyroid hormones)
This can be done via different mechanisms. For example, the pancreas and thyroid have ACE2 receptors, while the adrenal gland is victim to a heightened immune response and cytokine storm. Given the widespread functions throughout the body, hormonal imbalances can manifest with a myriad of symptoms.
Microbiome Changes
Studies show that COVID-19 can also lead to changes in the microbiome. In the gut microbiome, for example, these changes are characterized by a loss of friendly bacteria and an increase in opportunistic pathogens.
Microbes have many beneficial functions in different parts of the body, not just the gut. They stimulate the immune system, break down potentially toxic compounds, protect the skin, and control inflammation, to name just a few. Affecting the microbiome in different parts of the body can lead to a variety of different symptoms.
What body changes does COVID cause?

Individual symptoms vary widely among patients, with some symptoms persisting for months and others coming in waves.
This variability represents a significant challenge for both patients and healthcare providers, as the exact causes for each symptom remain difficult to understand. This list is still evolving, but some of the changes caused by COVID-19 include:
We’ll discuss each of them below, along with a few strategies to alleviate these symptoms.
Skin Rashes and Other Changes
COVID-19 can cause a variety of skin conditions. One of the most common problems is developing large red patches, often affecting the limbs and torso. Some patients also have skin rashes with blisters that look similar to chickenpox, while others have rings of skin discoloration. Some patients experience redness and swelling in one or more toes, a condition dubbed “COVID toes.” The affected areas can be painful to the touch, itchy, or have a burning sensation.
Although researchers don’t know exactly what causes these rashes to appear, the most likely explanations include direct infection of the skin via the ACE2 receptor, an excessive response by the immune system, or small blood clots that block blood flow to the skin. Elevated cortisol from stress due to the pandemic may also be involved. Our skin has receptors for this stress hormone and their activation results in increased inflammation, more oil production, and poor resistance to infection. Sometimes, rashes may be linked to altered blood circulation due to ANS dysfunction.
Most rashes that stem from COVID-19 only last a few days, though they may persist without treatment. In most cases, here’s how you can treat the rashes at home:
- Apply a cool compress to ease swelling and itching.
- Use over-the-counter creams to alleviate itching or swelling. Some examples include hydrocortisone cream or calamine lotion.
- Take antihistamines, which may help reduce symptoms caused by hive-like COVID-19 rashes.
- Avoid scratching affected areas, as this increases the risk of infection and scarring.
- Take stock of the products you’re currently using for skin care. Some people develop sensitive skin after COVID-19, so you might need to switch brands of shampoo, body soap, hand soap, and so forth.
- Some rashes can be stubborn and need medication. A dermatology practitioner can prescribe corticosteroids in a topical or oral formulation.
Loss of Smell and Taste
Anosmia is perhaps the most well-known symptom of COVID-19. It usually presents as a sudden loss of smell, sometimes accompanied by a loss of taste. Instead of a loss of smell, some patients describe a feeling that some things have a different or unpleasant smell (parosmia), or they’re constantly getting a whiff of something burning (phantosmia).
Curiously, olfactory neurons in the nose do not express ACE2 receptors, which means a direct attack on these cells is impossible. However, ACE2 is expressed in cells that provide structural support for these neurons, and these cells can die as a result of the infection, explaining the temporary loss of smell.
The vast majority of patients recover within two weeks. Up to 17% of patients who tested positive for COVID reported long-lasting changes in taste or sense of smell, according to a study reported by the Centers for Disease Control and Prevention (CDC). In a very small proportion of patients, however, loss of smell and taste can persist for much longer.
If you’re still experiencing loss of smell after a few weeks, smell training may be the best way to retrain your brain to smell. This treatment involves sniffing four items that have a strong and easily identifiable smell, such as garlic, coffee, or oranges. Patients must continue to do this twice a day for several months. Your doctor might also prescribe steroids, but beware of the possible side effects, which may include fluid retention, high blood pressure, and problems with mood swings and behavior.
Inflammation of the Heart
COVID-19 can damage the heart muscle and affect heart function. Some of the ways in which COVID-19 can affect your heart include:
- Faster heartbeat
- Heart palpitations
- Lower oxygen and nutrients in the blood
- Inflammation of the heart muscle (myocarditis) and heart lining (pericarditis)
Like the lungs, the heart has ACE2 receptors to which the coronavirus can attach before entering cells. Heart damage can also be the consequence of high levels of inflammation circulating in the body.
In addition, researchers believe this damage could be due to how the immune system reacts to the virus, which in turn affects the ANS. If this is the case, symptoms stem not from a cardiac problem but from a neurological issue that affects the heart. Patients may experience rapid heartbeats when standing up, brain fog, fatigue, palpitations, lightheadedness, and other symptoms.
If your symptoms don’t improve over time, or if you have a history of heart problems, we recommend that you seek medical help. Call 911 if your heart palpitations or faster heartbeat is accompanied by chest pain, dizziness, or blackouts.
Gastrointestinal Issues

According to a review that analyzed 125 studies and over 25,000 participants, the most common digestive problems after COVID infection include:
- Lack of appetite
- Distortion or lack of taste
- Diarrhea
- Nausea
- Vomiting up blood or GI bleeding
- Abdominal pain
- Indigestion
- Acid reflux
Just like it does with cells in the lungs, the SARS-CoV-2 can enter intestinal cells using the ACE2 receptor. In fact, these receptors are 100 times more common in the gastrointestinal tract than in the respiratory tract. For some patients, this attack may trigger an excessive release of cytokines or alter the gut microbiome, explaining many of the symptoms described above.
If you’re experiencing digestive problems, it’s important to follow a balanced diet and avoid any food items that may increase symptoms, such as fried or processed food. Make sure you’re hydrated at all times and add probiotics to your diet to improve gut health. If you notice a severe weight loss over a short period, visit your doctor or a nutritionist. Gastrointestinal problems can take a long time to diagnose and treat, so when in doubt, visit your doctor sooner rather than later.
Body Odor and Sweating Changes
During the pandemic, some COVID-19 patients started to notice changes in their body odor. Research is extremely limited, but one study showed that about one-fourth of patients with COVID-19 experience sweating dysfunction, which would affect body odor. Further research is needed, but the authors speculate this is the consequence of ANS dysfunction.
More specifically, sweating is under the control of the sympathetic nervous system, which regulates the body’s reaction to stressful situations. Under normal circumstances, sweating comes from glands known as eccrine glands. However, it’s possible that COVID-19-induced changes on the sympathetic nervous system stimulate the activity of another type of sweat glands known as apocrine glands. Sweat from these glands contains higher levels of proteins and fats that often result in a more pungent smell when broken down by bacteria present on the skin.
Changes in body odour may also be a consequence of living in isolation during the pandemic. Hygiene standards are easily dropped, especially for patients experiencing severe fatigue after COVID-19, and even dietary changes can cause a different body odor.
Small changes in sweating and body odor are usually not serious, but if you’re concerned about your symptoms, visit a dermatologist. At home, you can:
- Make sure you maintain good personal hygiene standards and wear clean clothes.
- Use an antiperspirant that works by pushing sweat back into your armpit’s sweat glands. This actually decreases underarm sweat production as your body receives a signal that your sweat glands are full. You can use either over-the-counter or prescription antiperspirants.
- Pay attention to what food items in your diet make your body odor more intense. Garlic, onions, and alcohol are the usual culprits.
- Find a way to reduce stress to limit sweat from the apocrine glands.
- If your body odor is coming from smelly feet, make sure you use an antibacterial soap on them every day and keep your toenails trimmed.
If you experience excessive sweating, you may have developed a condition known as hyperhidrosis. Hyperhidrosis often can’t be controlled by regular deodorants and is a medical condition requiring specific solutions to control. If you suspect hyperhidrosis, talk to your doctor about the next steps for treatment.
If the increased sweating does stem from autonomic dysfunction, then rehabilitating your ANS should help.
Reproductive Issues
One of the most surprising findings about COVID is the fact that both men and women can experience reproductive issues following an infection.
For women, there are several studies reporting changes in their period while sick with COVID-19, which then persist for some time after the infection. Symptoms include lighter or heavier flow, longer periods, irregular periods, and larger blood clots. Women might also might feel symptoms of early menopause, such as changes in body temperature and mood.
However, few studies have looked at how COVID-19 may cause these changes. A direct attack is unlikely because the lining of the uterus has very low levels of ACE2 receptors. In addition, levels of sex hormones — including follicle-stimulating hormone, estrogen, and progesterone — seem identical between healthy and sick women. It’s possible that the stress caused by the infection is enough to result in changes with your period. Changes could also result from autonomic nervous system dysfunction.
COVID-19 can also impact male reproductive health and testosterone levels. In this case, the virus can target testes directly, as this is actually one of the places in the body with the highest amount of ACE2 receptors. SARS-CoV-2 can also damage local blood vessels and lead to the formation of blood clots, potentially causing erectile dysfunction.
We’ve written in more detail here about the impact of COVID-19 and erectile dysfunction.
Tell your doctor if you’re experiencing any of these issues, especially after a COVID-19 infection. They may order some blood tests to check hormone levels and refer you to a urologist (for men) or a gynecologist (for women). You might also be referred to an endocrinologist for general hormone testing.
Type II Diabetes

Since the start of the pandemic, doctors have raised concerns about new cases of diabetes in people who had caught the virus. Researchers are still not sure if coronavirus is directly causing the new cases of diabetes or whether there are other factors that could explain the link, such as a more sedentary lifestyle and a poorer diet during the periods of isolation.
As a direct effect, COVID-19 may cause diabetes in certain patients by targeting ACE2 receptors in the pancreas, resulting in pancreatic injury and low insulin production. In addition, the virus also leads to increases in blood sugar levels, most likely caused by an excessive immune response. In more severe cases, patients may develop insulin resistance, which can lead to type II diabetes.
If you're diagnosed with diabetes after a COVID-19 infection, you should work with a medical provider to manage your condition with a healthy diet, regular exercise, and routine monitoring of your blood glucose. As type II diabetes is a progressive condition, you may eventually need insulin injections.
Kidney Problems
After a COVID-19 infection, some patients develop signs of kidney damage, even if they didn’t have any underlying kidney issues before they were infected with the virus. Common symptoms include decreased urine output and fluid retention that causes swelling in your legs, ankles, or feet. In fact, about one-third of patients hospitalized with COVID-19 experience kidney problems, with this value increasing to almost 90% in patients on mechanical ventilation.
There are several ways in which COVID-19 can trigger kidney problems. The obvious ones include through targeting of the ACE2 receptors present in the kidneys or as a consequence of an exaggerated immune response and a cytokine storm, but researchers believe other mechanisms may be at play. These include, for example, kidney damage caused by abnormally low levels of oxygen or tiny blood clots that clog blood vessels in the kidney.
It’s important to seek medical help if you experience any problems urinating. In extreme cases, patients with a severe kidney injury may need dialysis.
Eye Changes

One possible sign of COVID-19 is conjunctivitis (commonly known as pink eye). The hallmark symptom of this condition is the reddish color in the whites of the eyes that occurs when the blood vessels there become inflamed, making them more visible.
Other ocular symptoms caused by this virus include dry eyes, redness, itching, blurry vision, sensitivity to light, and the feeling that there is a foreign particle in the eye. Patients who need ventilators often develop a type of eye irritation called chemosis, which is a swelling of the eye membranes and eyelids. About 10% of patients with COVID experience some kind of eye problem, even if it’s just mild red eyes that don’t bother the patients.
Researchers still don’t know how the virus can inflict this damage on the eyes. It's possible that SARS-CoV-2 can attack the eye directly, as cells in the retina express the ACE2 receptor. Damage could also be due to an exacerbated inflammatory response to the disease in the form of a cytokine storm.
If you experience any of these symptoms, avoid rubbing your eyes or repeatedly flushing with water, as this will remove eye lubrication and increase the risk of infection. If you’re worried, discuss your symptoms with your eye care provider. There are other causes of conjunctivitis, including bacterial infection, allergens (pollen), and irritants (smoke or dust). Your doctor will be able to diagnose what you have based on your symptoms and medical history.
Hair Loss
A less well-known symptom of COVID-19 is hair loss. This is usually caused by shock hair loss (“telogen effluvium”), which happens when the growing phase of hair switches prematurely to a shedding phase, and patients lose a large amount of hair over a short period. Typically, this occurs all over the head, not just on the crown (as in the typical male pattern of baldness), and it involves about 50 to 100 hairs lost every day. Patients with telogen effluvium might also experience trichodynia, a painful sensation in the scalp.
It is thought that high fever during the COVID-19 infection and the subsequent immune response may trigger this pattern of hair loss. In addition, as this virus affects endothelial cells, it may block blood flow to hair follicles. Physical and emotional stress during the pandemic, as well as fast weight loss caused by digestive problems, may further aggravate hair loss.
Coronavirus can also lead to patchy hair loss known as alopecia areata. This happens when the body treats hair as a foreign body and starts attacking it. Researchers don’t know exactly why this happens after COVID, but it’s likely triggered when the immune system overreacts and triggers a cytokine storm.
Most patients start noticing hair loss about two to three months after the infection, when handfuls of hair come out in the shower or when brushing. In most cases, this condition is only temporary and patients will see an improvement after a few months.
Hair loss can be stressful. If you’re worried, seek medical advice from a dermatologist, especially if you don’t see any improvements after six months. It’s important that your doctor run tests to rule out other conditions such as iron deficiency or hormone imbalances. Your doctor may prescribe topical minoxidil, but this doesn’t work for all patients and may make the hair loss worse for some. Other advice includes eating a well-balanced diet, following a healthy sleep pattern, massaging your scalp in the shower, and minimizing stress by doing exercise, yoga, or meditation.
Weight Gain & Weight Loss
Nearly half of U.S. adults gained weight during the pandemic. For those working from home in isolation, this was mainly due to changes in eating habits, such as stress-induced overeating and snacking. Lockdown measures that closed gyms and kept many people inside their homes likely contributed as well.
But for COVID long haulers, this weight gain could have been caused by the virus. Studies have shown that the SARS-CoV-2 virus can attack adipose tissue, which then triggers an inflammatory response and disrupts normal metabolism. Worryingly, infection and inflammation coming from adipose tissue located next to critical organs — such as the heart or intestines — could be a potential source of further organ damage caused by COVID-19. This becomes even more concerning if you already have heart disease or other risk factors for post-COVID complications.
In contrast, some COVID patients experience rapid weight loss. In fact, about one-third of patients lose enough weight to put them at risk of malnutrition. What’s worse is that many of these patients remain malnourished for months after their original COVID infections and struggle to put the weight back on. The exact mechanism is still unclear; inflammation may be the initial trigger, but researchers believe there are other factors to explain the long-term effects.
If you experience severe body weight changes in either direction, we recommend that you visit your doctor. They can help diagnose conditions affecting your weight after COVID and put together a weight management plan to help you gain or lose weight as needed. They might want to track your body mass index (BMI) as you progress through recovery.
At home, follow a healthy lifestyle to gradually undo post-pandemic weight gain. Choose a balanced diet and engage in regular physical activity. If you need guidance, a nutritionist can coach you through healthy eating plans and make recommendations for supplements as needed.
Taking care of your mental health is important, too. Consider stress reduction activities, such as breathing exercises, yoga, and mindfulness movement exercises.
Treatment at Cognitive FX

The list of symptoms from COVID-19 is longer and more diverse than most doctors would ever have imagined before the pandemic. For some patients, ongoing problems go beyond the most common symptoms of COVID-19 (such as fatigue, headaches, shortness of breath, and brain fog) to include a wide range of body changes, from temporary skin rashes to permanent kidney problems.
At Cognitive FX, we believe the best approach to treat these patients is not to focus on individual symptoms, but instead, to look at the impact of COVID-19 as a whole. When COVID long haulers started reporting symptoms, we realized that many of their struggles overlapped with those of brain injury patients. We’ve since confirmed via brain imaging techniques that this is the case.

We work to restore healthy blood flow in the brain and to help the autonomic nervous system recover from COVID-19. Patients who go through treatment at our clinic show marked improvement in symptoms caused by those aspects of long COVID. That said, symptoms caused by other COVID shenanigans — such as tissue damage via ACE2 receptors or cytokine storms — will likely not improve. Because of that, we cannot claim to treat specific symptoms like COVID toes and heart inflammation.
That said, we can look at your medical history, brain scan, and the results of our in-person physical evaluation to put together a treatment plan for what we can influence. Before treatment starts, all patients must undergo a functional neurocognitive imaging (fNCI) scan to detect if and where the COVID-19 infection affected blood flow dynamics in the brain.
We then develop a tailored treatment plan for each patient, combining a series of therapies — including cognitive, sensorimotor, neuromuscular, vision therapy, and others — with physical exercise to promote brain and body healing.

Our treatment is called EPIC treatment, which is short for Enhanced Performance in Cognition.
Patients arrive on Monday for an evaluation, followed by therapy on Tuesday through Thursday, and a final evaluation on Friday. After treatment, our therapists meet with each patient to discuss progress and exercises to do at home while recovery continues. Continued effort at home is the best way to maximize your chances of recovery.
To determine if you’re eligible for treatment at our clinic, please sign up for a consultation with our team.
Further Reading
If you’re suffering from long-lasting symptoms after COVID-19, you may also find these resources helpful: