TMS vs. tDCS for Depression: Which Is Better?
For many people living with major depression, antidepressant medications either don’t work or only get them part of the way to recovery. Symptoms may ease for a while, but then return, or never fully...


Both Transcranial Magnetic Stimulation (TMS) and Vagus Nerve Stimulation (VNS) are FDA-approved neuromodulation treatments for depression. At first glance, they may seem similar—both use electricity to change how the brain functions—but the way they do so is very different.
TMS is a non-invasive procedure that uses magnetic fields to induce electrical currents in the brain, while VNS is an invasive therapy that requires a surgically implanted device to stimulate the vagus nerve.
If you’re deciding between the two, it’s important to understand how they work, their effectiveness, potential side effects, costs, and availability. Below, we compare these treatment options side by side so you can make an informed choice.
TMS treatment uses magnetic pulses to stimulate the dorsolateral prefrontal cortex (DLPFC)—a brain region linked to motivation, reward, and emotional regulation.
During treatment, a technician places an electromagnetic coil over the scalp. The coil delivers short bursts of magnetic energy that activate neurons in this region, helping to reset dysfunctional circuits associated with depression. Over time, repeated stimulation can rebalance brain activity and improve mood.
TMS has been used in the treatment of depression for nearly 20 years, with several different protocols now available:
Repetitive Transcranial Magnetic Stimulation (rTMS): The original and most widely used form. Sessions last ~37 minutes, five days per week, for four to six weeks.
Intermittent Theta-Burst Stimulation (iTBS): FDA-approved in 2018. Uses rapid bursts of pulses in sessions lasting just three minutes, enabling multiple sessions per day and faster results.
Deep TMS (dTMS): Uses an H-coil to reach deeper areas of the brain, approved for depression and obsessive-compulsive disorder (OCD), with ongoing research into other mental health conditions.
SAINT™ TMS: A Stanford-developed protocol combining iTBS with fMRI-guided precision targeting. It delivers accelerated treatment over just five days and has shown strikingly high response and remission rates in clinical trials.
Research shows that TMS offers substantial hope for patients who haven’t improved with antidepressant medications:
About 50% respond to rTMS, and ~30% achieve remission. Combining it with psychotherapy improves outcomes.
Standard (non-FMRI-guided) iTBS offers comparable results to rTMS.
Deep TMS may improve response rates for treatment-resistant depression (TRD), though long-term remission data is limited.
In one clinical trial of SAINT™, 85% responded and 78% achieved remission—exceptionally high for treatment-resistant patients.
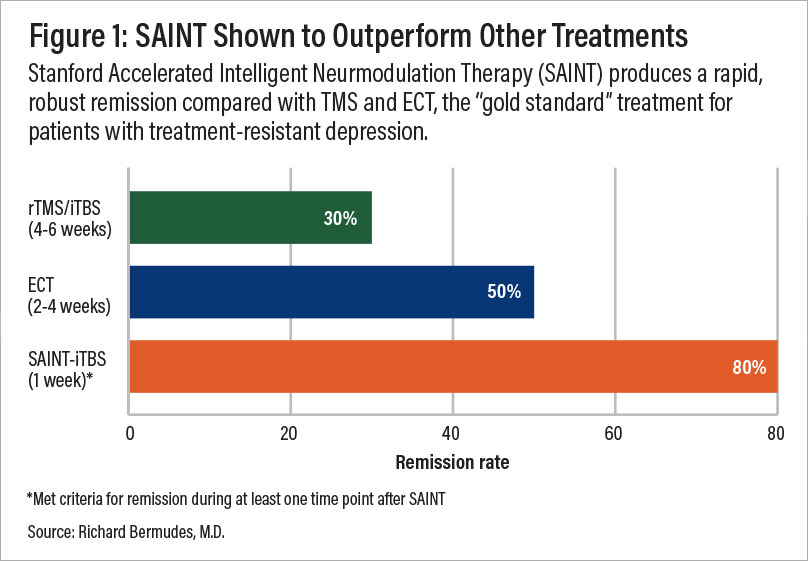
A comparison of remission rates for rTMS/iTBS, electroconvulsive therapy (ECT), and SAINT-iTBS.
One key limitation of rTMS lies in how technicians determine where to place the magnetic coil. The most common approach—the “5 cm method”—involves clinicians manually measuring the patient’s head to estimate the correct stimulation site.
While simple to perform, it does not account for individual differences in head size, shape, or brain structure. Even a deviation of just a few millimeters from the dorsolateral prefrontal cortex can significantly reduce treatment effectiveness.
To address this, Stanford researchers developed Stanford Intelligent Accelerated Neuromodulation Therapy (SAINT™), now regarded as the gold standard for treatment-resistant depression.
SAINT uses functional MRI (fMRI) to pinpoint each patient’s exact DLPFC location based on brain connectivity patterns. During treatment, neuronavigation software ensures the coil is placed over that precise spot for every session, eliminating much of the targeting inconsistency seen with traditional methods.
This precision—combined with an accelerated delivery schedule—has produced remarkable outcomes. The SAINT protocol delivers 10 sessions per day for 5 consecutive days, totaling 50 sessions. Many patients experience rapid and substantial symptom relief.
TMS is generally well-tolerated. Side effects are usually mild and short-lived, including:
Serious side effects, such as seizures, are very rare (<0.01%).
TMS may not be suitable if you have:
At Cognitive FX, we provide an accelerated fMRI-guided iTBS protocol that mirrors the precision and speed of SAINT™ TMS, but for a fraction of the cost. Learn more here, or take our quiz to see if you’re a good fit.
VNS involves a surgically implanted device, similar to a pacemaker, that sends mild electrical pulses through electrodes to the left vagus nerve in the chest. These signals travel to brain regions involved in mood regulation and can help reduce depressive symptoms.
The device is implanted under the skin during outpatient surgery and can last 3–8 years before needing battery replacement. Stimulation may be continuous or on-demand, and patients can often return home the same day.
VNS is also used for conditions such as epilepsy, chronic headaches, Parkinson’s disease, and post-stroke rehabilitation.
VNS is approved for patients with treatment-resistant depression who have failed at least four antidepressants and often electroconvulsive therapy (ECT). Patients must continue other depression treatments alongside VNS.
VNS is not a quick fix—improvements may take months to appear.
Having a VNS device is safe for most patients, but it does have some risks:
Most side effects lessen over time or can be managed by adjusting stimulation settings. The device can be turned off if problems persist.
Patients should inform doctors and security staff about the implant before MRIs or airport screenings.
VNS may not be suitable for patients who are pregnant, have respiratory or heart conditions, insulin-dependent diabetes, dysautonomia, certain psychiatric disorders, or a history of left-neck surgery involving the vagus nerve.
The total cost for vagus nerve stimulation varies significantly from clinic to clinic, so it’s worth shopping around if you’re interested in this treatment. In general, costs include:
Initial costs: Up to $10,000, covering surgery, device, general anesthesia, and follow-up programming.
Maintenance: Minimal, unless complications occur.
Insurance: Limited coverage, with strict eligibility requirements (TRD, no psychosis, informed consent, and adherence to follow-up care).
To find providers, visit LivaNova’s VNS Therapy website and use their locator tool.
| Factor | TMS | VNS |
|---|---|---|
| Mechanism | Magnetic pulses stimulate the DLPFC | Implanted device stimulates vagus nerve |
| Treatment Duration | 3–40 min per session, over 4–6 weeks (faster with accelerated TMS) | Ongoing stimulation for 3–8 years |
| Surgery | Non-invasive | Requires surgery |
| Efficacy | ~50% respond, ~30% remit (higher with accelerated protocols) | ~65% respond, ~40% remit over 5 years |
| Possible Side Effects | Mild headaches, scalp discomfort, seizures extremely rare | Surgical risks, voice changes, sleep, and breathing issues |
| Contraindications | Metal implants, seizure history, some meds, bipolar | Respiratory/heart issues, diabetes, certain psychiatric conditions |
| FDA Approval | MDD & TRD | TRD |
| Cost | $6,000–$15,000; up to $30,000+ for advanced protocols | Up to $10,000 upfront |
| Availability | rTMS widely available; limited availability for newer protocols | More limited, through specialty providers |
For patients who prefer to avoid surgery and want faster results, TMS may be the better option. Accelerated fMRI-guided iTBS, like the protocol we provide at Cognitive FX, offers rapid relief with high precision.
VNS may be more appealing to patients who want a “set it and forget it” treatment, since it requires no ongoing clinic visits once the device is implanted. However, it can take months to feel benefits, and side effects from stimulation may be more disruptive.
Ultimately, the right treatment depends on your medical history, treatment goals, and preferences.
Our clinic in Provo, Utah offers an accelerated fMRI-guided iTBS protocol that combines the core strengths of SAINT™—precision targeting and an accelerated treatment schedule—without the $30,000+ price tag.
Key differences from Magnus SAINT™ TMS:
We use advanced fMRI analysis by our neuroscientist and physician, rather than proprietary software, to determine the stimulation site.
We process scans in-house, leveraging 25 years of clinical fMRI experience from treating brain injury patients.
We pass those efficiencies on to patients: $9,000–$12,000 vs. $30,000+.
| Accelerated fMRI - TMS | Magnus SAINT™ TMS | |
|---|---|---|
| FDA-Approved iTBS | ✔ | ✔ |
| FDA-Approved Neuronavigators | ✔ | ✔ |
| FDA-Approved Figure 8 Coils | ✔ | ✔ |
| Number of Treatment Days | 5 | 5 |
| Treatments per Day | 10 | 10 |
| Total Treatments | 50 | 50 |
| Number of TMS Pulses | Approx. 90,000 | 90,000 |
| Resting motor threshold pulse intensity | 90–120% | 90–120% |
| FDA-Approved Personalized DLPFC Targeting | ✘ | ✔ |
| Personalized DLPFC Targeting Assists Doctor in Target Location | ✔ | ✘ |
| Personalized E Field Coil orientation | ✔ | ✘ |
| Cost | $9,000 to $12,000 | $30,000+ |
Our TMS treatment is:
We do not currently treat patients under 18, over 65, those with a history of seizures, or patients in acute suicidal crisis. While accelerated TMS is not covered by insurance, we can help patients access traditional rTMS through our sister clinic or other providers nationwide.
Click here to learn more about receiving accelerated fMRI TMS therapy at Cognitive FX. Or, take our quiz to see if you’re a good fit for treatment.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

For many people living with major depression, antidepressant medications either don’t work or only get them part of the way to recovery. Symptoms may ease for a while, but then return, or never fully...

While many people are learning about Transcranial Magnetic Stimulation (TMS) for the first time, this brain stimulation method has been helping patients for nearly 40 years. Originally developed as...

Transcranial magnetic stimulation (TMS) and neurofeedback are gaining popularity as non-invasive, medication-free options for treating depression—especially for people who haven’t found relief from ...

While antidepressant medications remain the most common first-line treatment for depression, research shows they only work for about one-third of patients and often come with unpleasant side effects...
If you’re wondering what to do when transcranial magnetic stimulation (TMS) doesn’t work, you might be:

Clinics across the U.S. now offer TMS therapy specifically for anxiety. While early research suggests TMS may be an effective treatment, only a handful of studies have focused exclusively on anxiety.