A Guide to Post-concussion Syndrome on Reddit
Post-concussion syndrome is downright frustrating to experience. Doctors often miss it during diagnosis, and even if they do make the diagnosis, treatment methods vary considerably from clinic to...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
Oxygen is good for the brain. A lack of oxygen is bad for the brain. So is getting more than normal levels of oxygen better for the brain?
This is the question behind using hyperbaric oxygen therapy (HBOT) to treat brain injury and other neurological disorders. It’s a treatment we considered offering at our clinic, Cognitive FX, where we specialize in treating patients with post-concussion syndrome (PCS).
HBOT has been used for decades to treat decompression sickness. It’s also approved by the U.S. Food and Drug Administration (FDA) to treat certain other conditions, such as acute carbon monoxide poisoning and wounds that aren’t healing
But some practitioners have begun to offer HBOT as an off-label treatment (meaning not approved by the FDA) for conditions such as Alzheimer’s Disease, autism, multiple sclerosis, post-traumatic stress disorder (PTSD), stroke, and post-concussion syndrome.
The health care professionals who use HBOT for mild traumatic brain injury (mTBI) are doing so because they hope that giving more of a good thing (oxygen) to the brain will help it recover.
We know that brain cells need oxygen to survive and to function properly. Brain trauma disrupts the flow of oxygen to injured parts of the brain, often leading to cell damage and dysfunction. HBOT forces much more oxygen than normal into your blood vessels, which is known to promote healing in damaged, oxygen-starved tissues. It’s reasonable to hypothesize that getting this hyper-oxygenated blood into an injured brain might be beneficial.
Unfortunately, it’s not that simple. Brain injuries vary in severity; not all brain injuries result in tissue damage that could benefit from excess oxygen. In addition, the brain uses a complex communication system, known as neurovascular coupling (NVC), to summon precise amounts of oxygen in specific regions of the brain as needed. It doesn’t need or use equal amounts of oxygen everywhere at the same time, which is what HBOT provides.
We ultimately decided against offering HBOT in our practice. Here’s why:
If you’re considering HBOT for mTBI or post-concussion syndrome treatment, we recommend pursuing other options. While we have no reason to think HBOT will harm you, we also don’t have any reason to think it will help.
In this post, we explain how we came to that conclusion, including:
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, sign up for a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
The air we breathe consists of 21% oxygen. Hyperbaric oxygen treatment provides 100% oxygen in an environment where the air pressure gradually increases to 1.5 to 3 times higher than normal. It takes place in a hyperbaric chamber, which is either a tube that resembles an MRI machine or a small room where several people wearing masks or hoods can be treated at the same time.
Breathing pure oxygen in a pressurized environment fills the lungs with oxygen more efficiently, thus sending more oxygen into the bloodstream. It is then available to be used throughout the body.
Breathing oxygen at this concentration for long periods can be toxic, so individual therapy sessions last no more than two hours. The number of HBOT sessions required depends on the condition being treated. Two or three sessions might be needed for carbon monoxide poisoning, whereas 20 to 40 visits are common to treat wounds that aren’t healing.

Temporarily increasing the amount of oxygen in the bloodstream with HBOT is beneficial by either returning blood to its normal levels of gases, as in the case of decompression sickness or carbon monoxide poisoning, or to prevent infection or promote healing of damaged tissues.
Hyperbaric oxygen therapy is a life-saving treatment for patients with hypoxia (when blood oxygen levels are too low).
Carbon monoxide is an odorless gas produced by burning fossil fuels. When you breathe it in, it replaces the oxygen in your blood. This starves your organs of oxygen. It can lead to permanent organ damage, brain damage, and even death. Carbon monoxide poisoning also causes persistent neurological dysfunction, such as memory problems, difficulty concentrating, anxiety, depression, and vestibular problems.
HBOT treats acute carbon monoxide poisoning by quickly forcing excess carbon monoxide from the blood. Research shows it can reduce the incidence of long-term cognitive impairment by up to 46% when done at this stage.
Decompression sickness happens during a rapid decrease in air pressure. In pressurized environments, excess nitrogen molecules accumulate in the blood. If they aren’t expelled slowly during decompression, dangerous bubbles form in the blood and tissue. This condition typically affects scuba divers, but it can happen to anyone working in a pressurized environment or when quickly going from high to low altitudes. HBOT quickly removes the bubbles and allows oxygen back into tissues.
Damaged tissue needs more oxygen than normal to survive and heal.
Sometimes blood vessels to the wound are damaged. This leads to swelling of the tissues and reduces the amount of oxygen needed to promote healing.
Wounds are also susceptible to infection. Oxygen improves the ability of white blood cells to fight infection. In addition, oxygen is needed to stimulate the growth of new cells and blood vessels (called angiogenesis).
HBOT can provide that extra boost of oxygen in these situations. The Undersea & Hyperbaric Medical Society has approved HBOT to treat burns, gangrene, bone and skin infections, diabetic ulcers, skin grafts, some radiation injuries, and a few other related conditions.
Hyperbaric oxygen therapy is generally safe as long as it is conducted properly; however, it is not without risk.
The most common side effects are usually minor and temporary. They include middle ear injuries, sinus pain, nearsightedness, fatigue, and headaches. More serious and much less common side effects are lung collapse, seizures, embolism, and oxygen poisoning.
The increasing off-label uses of HBOT prompted the FDA to issue a bulletin in 2013 and updated 2021, “Hyperbaric Oxygen Therapy: Get the Facts,” to help make consumers better informed when making treatment decisions. The bulletin warns that some entities falsely lead consumers to believe HBOT has been tested and approved to treat certain conditions.
HBOT is generally safe, but it’s important to make an informed decision before consenting to any treatment.
As we discussed above, hyperbaric oxygen treatment has been shown to help reduce swelling and promote healing associated with tissue damage at a wound site. This is key to understanding if and how HBOT is useful when treating brain injury.
Before we dig into those details, let’s clarify some terms used to describe head trauma. The term “traumatic brain injury” covers a broad range of injury severity.
The vast majority of TBIs are concussions. A concussion is called a mild TBI because there is no skull fracture, bleeding within the brain, or obvious brain tissue damage. It’s not usually life threatening. This doesn’t mean there’s been no harm done, however.
A blow to the head or any kind of sudden jolting causes the brain to crash into the skull, leading to some inflammation and damage to cells in the area of injury. Most people recover completely within a few days or weeks. Up to 30% of people who suffer a concussion develop post-concussion syndrome, which is when symptoms of a concussion last longer than three months after the initial injury. (Note: You can develop post-concussion syndrome after a moderate or severe TBI as well.)
Patients can also suffer mild TBI from sickness (like some bacterial and viral infections), chemical causes like chemotherapy, carbon monoxide poisoning, stroke, and more.
A moderate TBI might have some visible sign of injury on the head, a hairline fracture, or bleeding that is determined not to be life-threatening. You might be kept under observation for a while with a moderate TBI, but you don’t usually need surgery.
A severe TBI usually causes significant loss of consciousness — possibly even a coma — and often a serious skull fracture. Life-threatening bleeding usually requires immediate neurosurgery. This type of injury causes significant swelling and tissue damage. Emergency surgery for the head injury itself can also cause damage. Recovery is long and difficult, often with some permanent disability associated with it.
Researchers started investigating HBOT as a TBI treatment in the 1960’s because of its ability to slow cell death, suppress inflammation, and boost cell and blood vessel growth. Most of the research was conducted on animals until recently because of the ethical issues involved in experimenting on humans with acute, severe brain injury.
One of the biggest issues complicating research of HBOT in brain injury is the ability to conduct randomized, double-blind, placebo-controlled studies. Brain injury varies widely from person to person, making it difficult to find TBI patients to study who have similar injury severity and affected regions. Finding an objective way to measure the effects of HBOT is also an obstacle.
Several published studies failed to use a placebo. Recently, some researchers have devised and used a placebo (also known as sham treatment) for HBOT in their studies, usually by increasing the air pressure without changing the oxygen content of the air being delivered. It’s imperfect (since air pressure increases while oxygen stays the same), but it does improve the reliability of results.
Finally, it’s very expensive to conduct this type of clinical trial. Not everyone has the funding to do so.
A retrospective review of studies using HBOT in experimental and clinical TBI treatment published in 2016 reported some success when HBOT was used in the acute stage of TBI. The authors noted that most successes occurred within hours after the TBI.
However, the authors cautioned that the methods of assessing the clinical effectiveness of HBOT are imprecise and subjective in these studies, relying for the most part on neuropsychological tests such as the Rivermead Post-Concussion Symptoms Questionnaire.
A study of 56 children with severe TBI concluded that those who received HBOT had better outcomes than those with similar injuries who did not receive the treatment. The children received three treatments within a one-week period after stabilizing medically, about 10 to 12 days after injury. The authors assert that HBOT significantly improved quality of life and reduced complications in these children as compared to the control group.
The authors of both studies stressed the need for high-quality studies using an objective, clinical assessment.
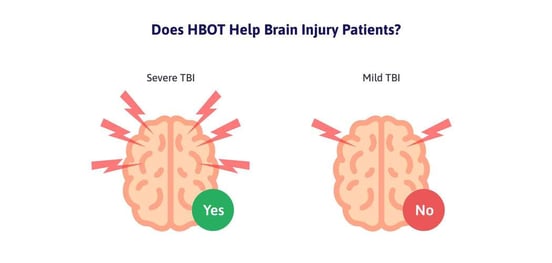
The effectiveness of HBOT in acute severe TBI could be because of the amount of swelling, tissue damage, and blood vessel damage that is present in these cases, all of which can be helped by the delivery of extra oxygen that HBOT supplies.
There is some disagreement surrounding the use of HBOT for those suffering from post-concussion syndrome after an mTBI.
Very few researchers report successful findings. And of those that do, most improvement is indistinguishable from the placebo effect. There is one study of 56 patients showing significant improvement in symptoms and increased brain activity as shown by single-photon emission computed tomography (SPECT) brain imaging scans. They did not have a placebo treatment for comparison.
While SPECT scans can detect some brain dysfunction, they can’t provide detailed information about specific areas of injury at a precise moment and are notoriously difficult to read. While the information obtained from a SPECT scan has its usefulness, it’s not enough to say with certainty that HBOT itself induced healing of brain injury.
Most research on HBOT for post-concussion syndrome (PCS) directly contradicts the findings of this research.
A comprehensive review of research using HBOT for TBI was published in 2016. It looked at 12 randomized trials. Of those studies, four focused on patients with PCS after an mTBI and included the use of a sham treatment. These studies assessed some combination of cognitive function, psychological outcomes, and self-reported post-concussion symptoms. The review revealed no difference in outcome between those who received HBOT therapy and those who had the placebo treatment.
It’s also worth noting that the United States Department of Defense commissioned five studies to determine the effectiveness of HBOT in treating post-concussion syndrome after mTBI in service members. The report to the United States Senate in January 2018 on the findings of four of those studies stated that while the hyperbaric and sham treatment caused no harm, there was no statistically significant benefit to HBOT when compared to the placebo.
These studies showed some improvement of symptoms in both groups. Researchers suspect the placebo effect is behind the improvement in the group that received the sham treatment but doesn’t rule out other factors.
If you’re experiencing emotional and physical symptoms that won’t resolve after a concussion or other mild brain injury, you’re not alone. 95% of our patients experience statistically verified restoration of brain function after treatment. To see if you are eligible for treatment, sign up for a consultation.
Getting oxygen to the brain is crucial to healthy brain function and to the elimination or reduction of symptoms of post-concussion syndrome. However, oxygen must be delivered to the right place at the right time in just the right amount. The system that governs this is neurovascular coupling: the connection between neurons and blood vessels in the brain.
Scientists are still studying precisely how this intricate communication system within the brain works, but we know that when your brain perceives a need for action, the region of the brain that controls the action calls for enough oxygen (energy) to perform it. The oxygen needs to arrive at the right time for everything to go off without a hitch.
For example, if you play a musical instrument, several areas of your brain are going to engage when it’s time to play. Your brain has to remember how to read music (or to recall memorized lines of music). Your fingers have to make the right movements to play the instrument. Proper breathing is involved too. As soon as you decide to play, the specific areas of your brain that are responsible for all these actions orchestrate this entire process. The neurons anticipate the amount of energy needed and call for it. Blood vessels respond with the delivery of oxygen exactly when it’s needed. This is neurovascular coupling in action.
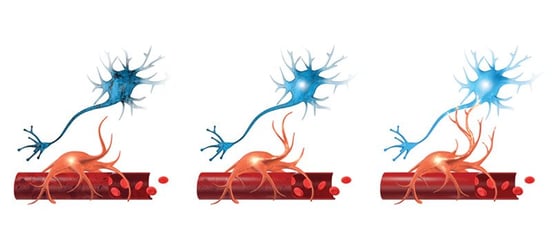
After a brain injury, cells in the area of injury often sustain some damage, making it difficult for them to send and receive messages properly. Localized inflammation often temporarily impedes the ability of blood vessels to deliver oxygen.
Often the brain tries to work around these problems by creating new pathways to deliver messages and oxygen, but these new pathways are less efficient than the original ones. It’s like when your high-speed internet goes out in the middle of a download. If it’s temporary, it’s a minor inconvenience. The internet resets and you try again. But if it keeps happening — or if your internet is permanently disabled — your productivity goes way down. Everything takes longer, and you get tired and frustrated.
Neurovascular coupling dysfunction causes most symptoms of concussion. Usually it’s only temporary after a brain injury. After a few days or weeks, the brain heals, and things go back to normal. But in the case of post-concussion syndrome, the brain continues to use the inefficient pathways that were supposed to be temporary. Some parts of the brain might try to compensate for other areas, but they don’t have the energy to work overtime indefinitely. Some areas of the brain might be getting too much oxygen, or not enough, for the targeted task.
The intricate call-and-deliver system of neurovascular coupling is at odds with the way HBOT floods the brain with highly concentrated oxygen.
Researchers at UCLA used functional magnetic resonance imaging (fMRI) to observe what happened in the brains of 14 children when they were given 100% oxygen for two minutes. (Note: fMRI is a type of MRI that can observe blood flow that is tied to brain activity.)
The increase in oxygen caused a quick decrease of carbon dioxide in their blood. Then, their blood vessels constricted, resulting in a decrease of oxygen reaching the brains and hearts of the children.
Blood vessel constriction like this can be helpful when you want to combat inflammation, but in cases of long-term post-concussion symptoms, the inflammation associated with the concussion is gone. In addition to decreasing the amount of oxygen reaching the brain, flooding the blood with oxygen interferes with the delicate balance of oxygen the brain is used to receiving.
That said, we still don’t know everything there is to know about brain injury. HBOT is effective in repairing tissue damage. It’s possible that in some cases, there could be some lingering tissue damage around the neurons caused by an mTBI. In that case, HBOT might help repair it and result in some improvement.
When administered properly, HBOT doesn’t seem to cause any harm. When potential patients ask us if they should consider it before coming to Cognitive FX for treatment, we tell them it probably won’t help, but if it’s something they really want to try, it’s probably not going to hurt anything (besides their wallets).

We designed Enhanced Performance in Cognition (EPIC) Treatment specifically to treat post-concussion syndrome. It works by repairing the neurovascular coupling dysfunction that causes symptoms.
Before treatment begins, we locate specific areas of neurovascular coupling dysfunction in the brain using a form of fMRI called functional neurocognitive imaging (fNCI). Using fNCI, we take over 7000 images of 60+ regions of the brain as the patient performs a series of specific cognitive tasks. These images allow us to see cerebral blood flow in the brain as it responds to the demands of these cognitive tasks.
During our research, we compiled a database of images from hundreds of people with and without brain injury performing those same tasks. We now have a statistical norm for each brain region to compare with each patient’s scans. Any brain region that is +/- 0.75 standard deviation from the norm indicates an area of neurovascular coupling dysfunction.
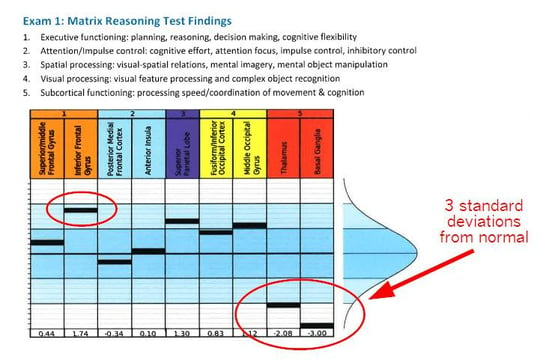 An example of results for one of our patients. She writes, “The fNCI showed that my thalamus was hypoactive and my basal ganglia was completely out to lunch. 3 standard deviations from normal basically means that there was no activation seen in that area on the fMRI. All the work was being routed around it — causing fatigue and stress on the rest of my brain.”
An example of results for one of our patients. She writes, “The fNCI showed that my thalamus was hypoactive and my basal ganglia was completely out to lunch. 3 standard deviations from normal basically means that there was no activation seen in that area on the fMRI. All the work was being routed around it — causing fatigue and stress on the rest of my brain.”
Our experienced treatment team includes a neuropsychologist, a neuroscientist, a neuroradiologist, a psychologist, and numerous therapists who are experienced working with post-concussion syndrome. We analyze the fNCI results of each patient to create an individualized treatment plan that focuses on their specific areas of dysfunction.
Treatment typically takes place during one (or more) intense week(s). It consists of a combination of therapies, including aerobic exercise (made safe even for those with exercise intolerance), neuromuscular therapy, sensorimotor therapy, cognitive exercises, balance therapy, vision therapy, and occupational therapy. We also incorporate breathing exercises, relaxation techniques, and mindfulness. Each patient meets with our psychologist to help with the emotional aspects of therapy and recovery.

It’s this unique combination of multidisciplinary therapies combined with aerobic activity that makes EPIC treatment work. Aerobic exercise naturally provides extra oxygen to the brain, also allowing it to benefit from what’s called the Post Exercise Cognitive Boost (PECB). During PECB, essential neurotransmitters and proteins that help promote blood flow are released in the brain. This allows your brain to perform cognitive tasks for longer periods of time.
These therapies challenge your brain, pushing it to abandon the inefficient pathways formed after injury and teaching it to use healthy neurovascular coupling. Once that happens, post-concussion symptoms subside.
We send each patient home with an individualized post-treatment plan of exercises to continue improving. We follow up with every patient to answer questions and make adjustments to that routine if necessary.

At the end of treatment, patients repeat the fNCI. We compare before-and-after results and give you a detailed report of each brain region we’ve measured.
Our patients average 77.5% improvement on their scans after just one week. They also report a 60% average improvement of post-concussion syndrome symptoms at the end of that same week.
We know how crazy this sounds.
We’ve treated thousands of patients with post-concussion syndrome. They tell us how they’ve been searching for answers for years. Some have tried treatment after treatment without success. Others have been told there’s nothing wrong with them, or that nothing more can be done. Many were skeptical that something as simple sounding as EPIC treatment could be effective. You can read some of their stories in our post, Living with Post Concussion Syndrome: How 7 Patients Found Hope for Recovery. You can also hear from patients in their own words in the Patient Stories section of our blog.
Post-concussion syndrome is real. Its effects are often devastating, but there is an effective treatment for it. To see if you are eligible for treatment, sign up for a consultation.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

Post-concussion syndrome is downright frustrating to experience. Doctors often miss it during diagnosis, and even if they do make the diagnosis, treatment methods vary considerably from clinic to...

Severe traumatic brain injury (TBI), concussion (mild traumatic brain injury or mTBI), and other head trauma can cause high blood pressure, low blood pressure, and other circulatory system changes....

Very few clinics offer specialized treatment forpost concussion syndrome (PCS). Cognitive FX specializes exclusively in treating the root causes of lingering post-concussion symptoms (as well as...
Perhaps this sounds familiar: You wake up from a relaxing nap expecting to feel refreshed, but instead, your heart is pounding for no reason. Or you stand up after a few hours on the couch and feel...

Recovering from a traumatic brain injury (TBI) often means dealing with physical symptoms, such as headaches, balance issues, weak muscles, and vision problems. These symptoms can affect every aspect...

Dry needling and acupuncture can help relieve certain post-concussion symptoms. They are not a cure-all, either for acute concussion or post-concussion syndrome, but if you suffer from headaches,...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY