Key Factors When Looking for Accelerated TMS Near You
A major challenge for patients with depression is that traditional antidepressant medications often take weeks or months to show results — if they work at all. This delay can be especially...


If you’re wondering what to do when transcranial magnetic stimulation (TMS) doesn’t work, you might be:
No matter where you are in the process, it can be disheartening to face uncertainty—especially if you’ve already tried multiple medications or therapies with little relief.
When TMS doesn’t deliver the expected benefits, it’s easy to feel discouraged or even hopeless. But you’re not alone—and you’re not out of options.
In this article, we discuss:
TMS can be a life-changing treatment for many people, but it’s not effective for everyone. Here are some potential reasons why TMS may not be producing the desired results:
TMS is FDA-approved for major depressive disorder (MDD) and treatment-resistant depression (TRD). If a patient is misdiagnosed—for example, they have bipolar disorder or schizophrenia—TMS may be ineffective or even worsen depression symptoms. A comprehensive psychological evaluation is essential before starting TMS treatment.
One of the most common technical reasons for poor outcomes is inaccurate placement of the magnetic coil. TMS works by stimulating a specific area of the brain known as the dorsolateral prefrontal cortex (DLPFC). The DLPFC as a whole isn’t hard to locate, but pinpointing the specific spot within the DLPFC that makes treatment work can be difficult.
The widely used “5 cm method” estimates coil placement based on external landmarks, which often fails to account for individual variations in head size, shape, and brain structure. As a result, the coil may stimulate the wrong part of the brain—leading to poor outcomes or even symptom worsening.
Roughly 20–25% of TMS patients experience a temporary worsening of symptoms during the first few sessions—a phenomenon known as the “TMS dip.”
This is a normal part of brain reorganization and often indicates that the brain is responding to treatment. Many patients who experience this go on to see meaningful improvements.
Common side effects like headaches, dizziness, or facial discomfort may be mistaken as signs the treatment isn’t working. These side effects are typically mild and temporary.
Severe side effects, such as seizures, are extremely rare (less than 1 in 10,000 sessions). TMS can trigger mania in patients with bipolar disorder, which is why proper screening is essential.
Further reading: Is TMS safe?
Missing occasional sessions is usually not a concern, but frequent or consecutive missed sessions—especially during the early stages—can reduce the effectiveness of treatment.
TMS may take longer to work for patients with severe depression or co-occurring mental health conditions such as anxiety, PTSD, obsessive-compulsive disorder (OCD), or bipolar disorder. In these cases, combining TMS with other treatments (e.g., antidepressant medications or psychotherapy) may enhance outcomes.
If you expect dramatic improvements within days, slower progress can feel like failure. In reality, changes are often gradual. Some patients don’t notice significant improvements until weeks after completing the full course of treatment.
For example, one of our patients worried that her treatment may not have worked in the first few weeks after treatment. But then something shifted.
“I suddenly realized I hadn’t felt that cloud in days. Smiling was easier. Laughing was easier. It just crept up on me—and then it felt like the sun just broke through. I went five months without a single depressive crash. That was monumental for me.”
Read Sarah’s success story here.
Your provider can reassess your diagnosis, treatment history, and coil placement technique. This review may reveal adjustments or alternative approaches that could improve outcomes.
In general, sticking with your treatment plan will give you the best chance at responding to TMS. Everyone responds at a different pace. While some feel better after a few TMS sessions, others see changes only after completing the full 4–6 week course—or even several weeks later.
Exception: If TMS causes extreme anxiety, distress, or challenging side effects, your provider may recommend pausing or stopping treatment.
Ask your provider about adjusting stimulation intensity, coil angle, or target location. These changes can increase the comfort and effectiveness of TMS.
If your symptoms begin to return some time after completing TMS, maintenance sessions (weekly, bi-weekly, or monthly) can help sustain progress.
Medication: Combining TMS with antidepressant medication may improve outcomes, though certain medications (e.g., tricyclics, some antipsychotics) may be contraindicated.
Psychotherapy: Talk therapy—especially cognitive behavioral therapy (CBT)—can enhance TMS effectiveness by reinforcing behavioral and cognitive changes. Studies suggest that combining TMS and CBT may be more effective than either treatment alone, particularly for patients with treatment-resistant depression. We follow this approach at Cognitive FX, and we’ll explain more below.
Lifestyle changes: Exercise, diet, sleep hygiene, and stress management all support brain health and can improve how your body responds to TMS.
Typically, only about 50% of patients respond to conventional TMS (rTMS), and just over 30% achieve remission.
If you tried rTMS without success, it may be worth exploring a more advanced protocol.
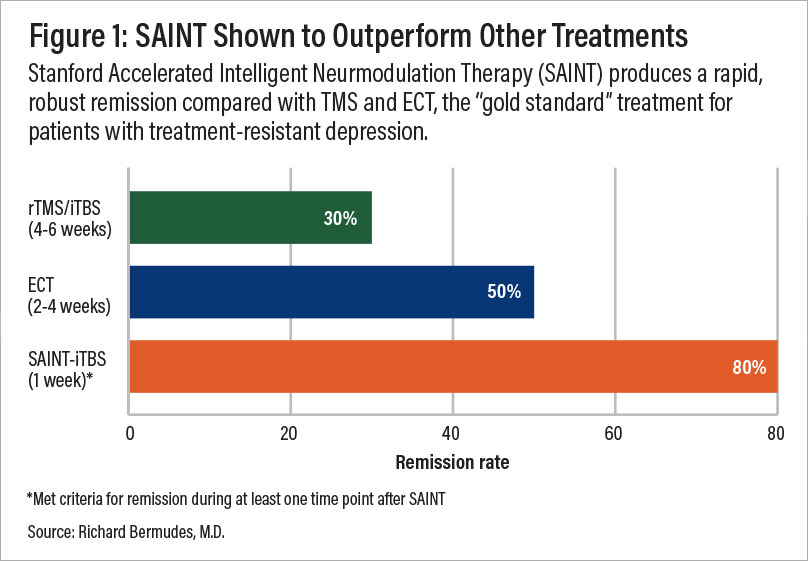
SAINT™ (Stanford Accelerated Intelligent Neuromodulation Therapy) uses intermittent theta-burst stimulation (iTBS), a more advanced brain stimulation that mimics natural brain wave rhythms, combined with fMRI-guided coil placement for precise targeting.
This ensures magnetic pulses hit the exact brain target, tailored to each patient’s head size, shape, and brain structure.
It delivers 10 sessions per day for five days—50 sessions total—compressing the typical 4- to 6-week treatment course into one week.
Clinical trials have yielded some of the highest depression treatment success rates to date:
While highly effective, SAINT™ costs roughly $30,000 and isn’t yet covered by most insurance providers.
At Cognitive FX, we offer a similar accelerated TMS protocol combining fMRI-guided targeting with theta burst stimulation—at a fraction of the cost ($9,000–$12,000).
| Accelerated fMRI - TMS | Magnus SAINT™ TMS | |
|---|---|---|
| FDA-Approved iTBS | ✔ | ✔ |
| FDA-Approved Neuronavigators | ✔ | ✔ |
| FDA-Approved Figure 8 Coils | ✔ | ✔ |
| Number of Treatment Days | 5 | 5 |
| Treatments per Day | 10 | 10 |
| Total Treatments | 50 | 50 |
| Number of TMS Pulses | Approx. 90,000 | 90,000 |
| Resting motor threshold pulse intensity | 90–120% | 90–120% |
| FDA-Approved Personalized DLPFC Targeting | ✘ | ✔ |
| Personalized DLPFC Targeting Assists Doctor in Target Location | ✔ | ✘ |
| Personalized E Field Coil orientation | ✔ | ✘ |
| Cost | $9,000 to $12,000 | $30,000+ |
Our team uses advanced fMRI post-processing to pinpoint each patient’s ideal DLPFC target based on functional brain patterns. You receive the same precision as SAINT™—but at a significantly lower cost.
We also include cognitive behavioral therapy during treatment, which can boost remission rates by up to 19% and support longer-term benefits.
Note: We do not treat patients under 18 or over 65, those with a history of seizures, or patients in immediate crisis.
To see if you’re a good fit for our accelerated fMRI-TMS treatment, take our good fit quiz. You can learn more about our approach here.
Further reading: ECT vs. TMS: side effects, effectiveness & cost
Further reading: Vagus nerve stimulation
Further reading: Ketamine vs. TMS
Lifestyle changes can reinforce the benefits of TMS or other therapies:
If TMS hasn’t worked for you, there are still paths forward. Whether it’s completing your current treatment, adjusting your protocol, trying a more advanced method like accelerated fMRI-TMS, or exploring alternative therapies, there is hope.
At Cognitive FX, we’re committed to providing precision-guided, effective care for patients with treatment-resistant depression—without the price tag of proprietary protocols.
To see if you’re a good fit for our accelerated fMRI-TMS treatment, take our good fit quiz. You can learn more about our approach here.

Dr. Mark D. Allen holds a Ph.D. in Cognitive Science from Johns Hopkins University and received post-doctoral training in Cognitive Neuroscience and Functional Neuroimaging at the University of Washington. As a co-founder of Cognitive Fx, he played a pivotal role in establishing the unique and exceptional treatment approach. Dr. Allen is renowned for his pioneering work in adapting fMRI for clinical use. His contributions encompass neuroimaging biomarkers development for post-concussion diagnosis and innovative research into the pathophysiology of chronic post-concussion symptoms. He's conducted over 10,000 individualized fMRI patient assessments and crafted a high-intensity interval training program for neuronal and cerebrovascular recovery. Dr. Allen has also co-engineered a machine learning-based neuroanatomical discovery tool and advanced fMRI analysis techniques, ensuring more reliable analysis for concussion patients.

A major challenge for patients with depression is that traditional antidepressant medications often take weeks or months to show results — if they work at all. This delay can be especially...

If you’re considering brain stimulation therapy for treating major depression, you may wish to understand the differences between repetitive transcranial magnetic stimulation (rTMS) and deep...

The type of protocol used is the most important factor influencing the price of TMS. Conventional TMS protocols are often the most affordable, while advanced protocols typically cost more, but can...

Transcranial magnetic stimulation (TMS) has been FDA-approved for treating major depressive disorder (MDD) since 2008 and is a well-established treatment option, especially for patients who haven’t...
Although transcranial magnetic stimulation (TMS) has been used for over 20 years and FDA-approved for treating major depressive disorder since 2008, it remains relatively less well-known among the...

If you’ve undergone TMS therapy and noticed an increase in depressive symptoms, you might worry the treatment wasn’t right for you. Similarly, if you’re considering TMS, you may wonder: Could TMS...