The number of patients with long COVID may be decreasing, but those still experiencing the condition need reliable treatments and resources for recovery more than ever.
The problem is that doctors still don’t know why some patients develop this condition and haven’t agreed on a gold-standard treatment. At the moment, there is no single strategy that helps everyone. The good news is that there are many treatments and at-home strategies that help long COVID recovery. The key is figuring out which ones are the most helpful for your individual situation.
At Cognitive FX, we tailor our treatment approach for each patient. We have been caring for patients with long COVID using a multidisciplinary approach since the first cases started to emerge. We use a state-of-the-art brain imaging scan (fNCI) to determine exactly how the virus disrupted blood flow dynamics and cross-region communication in the brain. With the scan results and information from a rigorous physical and cognitive evaluation, we develop a customized plan for each patient involving exercise, therapy, and rest. We also offer recommendations and resources for patients to use on their own or in conjunction with those offered by other care providers.
To learn more about how and why we developed this method, see our post on long COVID treatment.
In this article, we summarize 18 major treatments and at-home strategies to help with long COVID recovery, including the pros and cons of each.
Of the COVID long-haulers who meet our screening criteria, over 90% show improvement after treatment at our clinic. Our long COVID patients report over 40% decrease in symptom severity in 13 symptoms after just one week of multidisciplinary therapy. To discuss your specific long COVID symptoms and whether you’re eligible for treatment at our clinic, schedule a consultation.
Why Is Long COVID So Difficult to Treat?
The Centers for Disease Control and Prevention (CDC) defines long COVID as “signs, symptoms, and conditions that continue or develop after acute COVID-19 infection.” This condition can affect multiple parts of the body — such as the heart, lungs, kidneys, skin, and brain.
Despite this general definition, the current understanding is that long COVID should not be seen as a single disease, but as a group of conditions under the same umbrella. This means what triggers symptoms for one patient may not be the same as for another.
From our experience treating long-haulers, one of the main reasons behind symptoms is neurovascular coupling disruption. This occurs when the connection between brain cells and blood vessels in the brain is disrupted. Groups of cells with poor NVC might receive the wrong amount of resources or the right amount at the wrong time, and so forth. As a result, they no longer operate normally, forcing the brain to redistribute its work in an inefficient, taxing manner. Your symptoms may vary depending on which regions of the brain are affected by dysfunctional NVC. You can read more about NVC here.
Another possible explanation for the wide range of symptoms involves COVID-induced dysfunction of the Autonomic Nervous System (ANS). Under normal circumstances, two parts of the ANS — the sympathetic (SNS) and parasympathetic nervous system (PNS) — work together harmoniously. However, long COVID patients have to deal with an imbalance between the SNS and PNS (in most cases, overactivation of the sympathetic nervous system). This condition can cause symptoms such as abnormal heart rate, heart palpitations, blood pressure changes, fatigue, muscle pain, shortness of breath, and headaches.
Further reading: Yes, COVID causes POTS and dysautonomia
There are many other possibilities. Maybe your symptoms are caused by your immune system turning on you — a phenomenon known as autoimmunity; or maybe leftover viral particles remain in your body after the infection, keeping your immune system permanently on standby. It may be that COVID-19 dealt long-lasting damage to certain organs. Or, some think that the coronavirus awakens viruses that your body has fought before, such as the Epstein-Barr virus (which causes mononucleosis), for example.
All of these possibilities have some evidence to support them, and they’re not mutually exclusive. For some patients, these things could be happening all at the same time. This certainly would explain the sheer number of symptoms associated with long COVID (some symptom lists go over 200). However, this also makes treatment very challenging, making it all the more important to obtain an accurate diagnosis and a long-haul COVID treatment protocol that can be adapted to your specific needs.
With that in mind, here are some of the most prominent treatments offered today.
1. Hyperbaric Oxygen Therapy (HBOT)
![oxygen therapy in hyperbaric chamber [V6]](https://www.cognitivefxusa.com/hs-fs/hubfs/oxygen%20therapy%20in%20hyperbaric%20chamber%20%5BV6%5D.jpeg?width=1000&height=559&name=oxygen%20therapy%20in%20hyperbaric%20chamber%20%5BV6%5D.jpeg)
Possibly one of the most widely advertised treatments for long-term COVID-19 is hyperbaric oxygen therapy (HBOT). Briefly, this therapy involves putting patients inside a pressurized environment to breathe 100% pure oxygen. After an infection that causes inflammation, such as COVID-19, different tissues in the body sometimes struggle to receive enough oxygen, which delays the healing process.
During HBOT, patients alternate between pure oxygen and normal air (about 21% oxygen). When the body senses this drop, it interprets it as a lack of oxygen, which triggers the body to seek ways to repair itself. These responses include, for example, growing new blood vessels in the brain and activating the immune system.
A few studies show that HBOT can help long COVID patients, especially by improving memory and attention and reducing pain and fatigue. However, these results are based on limited data, and more research is needed to determine how effective it is and how long its effects last. There are some arguments that HBOT is more effective during acute infection than for long-haul treatment. For this reason, many medical experts — including Cognitive FX — advise caution in using it as a treatment for long-haulers. In addition, it’s not FDA approved for long COVID, and it’s an extremely expensive treatment only available at private facilities.
2. Repetitive Transcranial Magnetic Stimulation
Another type of treatment hailed to cure long COVID is called repetitive transcranial magnetic stimulation (rTMS). This is a non-invasive method of stimulating specific nerve pathways in the brain to promote certain changes in movement and behavior. RTMS has been found to be effective for a broad range of medical conditions, including movement disorders, such as dystonia and tremors caused by Parkinson’s disease, as well as for psychiatric conditions, such as depression and anxiety.
When it comes to long COVID, studies show that it can help neuropsychiatric symptoms, such as low mood and depression, but it does not improve physical symptoms such as fatigue. Similarly to HBOT, there are limited studies looking at how it can help long-haulers, so caution is advised. Nevertheless, this procedure has been approved by the FDA for treating depression with very positive results. This may help some long COVID patients with neurological and psychological symptoms, but it’s not a complete treatment.
3. Vaccines
As we’ve seen, long COVID is a complex and challenging condition to treat. As a way to counteract this, doctors are also working on preventative treatments to stop patients from developing long COVID in the first place.
Getting at least one dose of a COVID-19 vaccine not only lowers the risk of developing long-term COVID, but it also reduces the severity of the symptoms in those patients who develop this condition. Researchers don’t fully understand how the vaccine protects against long-term COVID but speculate that it may destroy any remaining viral reservoirs present in the body.
Unvaccinated people may benefit from the vaccine even if they already had the disease previously.
4. Paxlovid and Lagevrio

A second option to prevent long COVID was discovered by chance. In late 2021, the FDA approved a combination of nirmatrelvir and ritonavir (Brand name: Paxlovid) as the first antiviral medication to treat acute COVID-19. Very soon, it became clear that patients who had received Paxlovid soon after testing positive for the virus were less likely to develop long COVID. Recently, another study found a second antiviral — molnupiravir (Brand name: Lagevrio) — with a similar protective effect.
Similar to the vaccines, it’s believed these antivirals help eradicate any lingering viruses present in the body after the acute infection. Unfortunately, this protection is only activated if the antiviral is administered within a few days after the patient tests positive, but it has no effects if taken when patients realize they have long-term COVID.
5. Treating Individual Symptoms
Patients may need to seek treatments to help relieve specific post-COVID-19 symptoms they’re experiencing rather than focusing specifically on the virus. The downside of this approach is the need to visit multiple healthcare professionals, such as:
- Pulmonologists to treat a variety of breathing difficulties common in long-haulers, from shortness of breath to severe acute respiratory syndrome (SARS).
- Neurologists to address neurological symptoms of long COVID, including fatigue, headaches, and cognitive difficulties.
- Gastroenterologists to treat symptoms associated with the digestive system, including constipation, diarrhea, vomiting, and other signs of stomach distress.
- Cardiologists to check symptoms like chest pain, palpitations, or exercise intolerance. It’s also common for long-haulers to develop postural orthostatic tachycardia syndrome (POTS), a blood circulation disorder that causes lightheadedness or fainting when patients stand up from a lying down position.
- Psychiatrists and psychologists to help manage and treat neuropsychological symptoms caused by long-term COVID, including low mood, depression, and anxiety.
- Therapists to provide a variety of therapies, including speech and language therapy to help with communication and swallowing, occupational therapy to support your independence, and physical therapy to help with movement problems, to name just a few.
6. Multidisciplinary Rehabilitation Clinics

Taking the previous approach one step further, instead of having patients seek multiple healthcare professionals as needed, it is more supportive for patients to find different disciplines in the same place. Multidisciplinary long COVID rehabilitation clinics — with access to different medical specialties — are in a perfect position to recognize and respond to whatever symptoms patients are experiencing better and quicker than any other care models. Many healthcare providers believe these multidisciplinary clinics should form the backbone of our response to long COVID. Multiple hospitals around the country have now opened post-COVID clinics.
At Cognitive FX, we follow this multidisciplinary approach, but we offer more than just treatment for different symptoms under one roof. Our treatment tackles two common conditions underlying post-COVID syndrome: neurovascular coupling disruption and autonomic nervous system dysfunction.
We know this because we have seen it in our patients. We specialize in post-concussion syndrome (PCS), where patients suffer with long-term symptoms after a mild traumatic brain injury (mTBI) for months or even years. When patients started reporting long-term symptoms after COVID, we realized that PCS patients and long COVID patients had many symptoms in common.
We assessed long COVID patients using a brain imaging scan (see the procedures we follow below) and discovered that these patients were suffering from a similar type of brain dysfunction. We’ve since treated many long COVID patients with very positive results: Some symptoms improve immediately while others take a little longer, but most patients see significant improvements after our intensive treatment and continue to improve at home.
Treatment at Cognitive FX
We treat long COVID patients using a combination of physical exercise and multidisciplinary therapies. Our protocol includes:
- A detailed medical examination to determine how long COVID has affected your brain and body.
- Aerobic exercise to promote the release of important neurochemicals and healthier blood flow in the brain.
- Multidisciplinary therapies, such as cognitive therapy, sensorimotor therapy, neurointegration therapy, and physical therapy.
- Breathing exercises to support the autonomic nervous system (particularly important for long-haulers).
- Intentional rest (massage, meditation, etc.) to allow patients to recover before the next series of therapies.
- Patient support after treatment.
Before treatment starts, patients undergo a detailed medical examination. During this process, our doctors ask you about your symptoms, medical history, and any other relevant information, such as exams or treatments to address long COVID that you’ve already tried. This assessment also includes a physical exam to check reflex response, balance, and hand-eye coordination; a cognitive evaluation to assess cognitive issues, such as brain fog, poor memory, or difficulty focusing; and a psychological evaluation to detect signs of anxiety, depression, or other mental health problems.

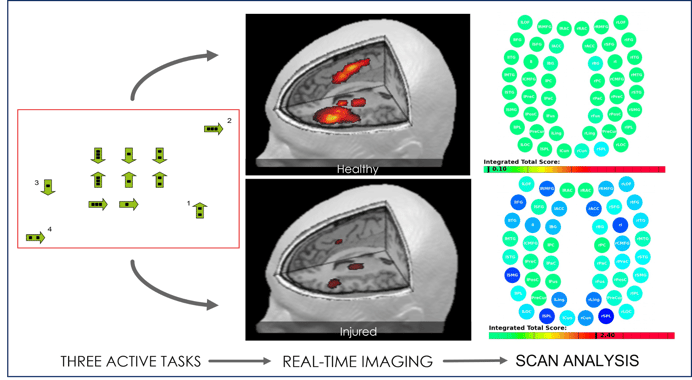
After this initial assessment, patients complete a brain imaging scan to find the areas in the brain most affected by the virus. The scan — called functional NeuroCognitive Imaging (fNCI) — investigates brain function in about 100 regions in the brain and how those regions communicate with each other. During the exam, the patient performs a series of standardized cognitive tasks.
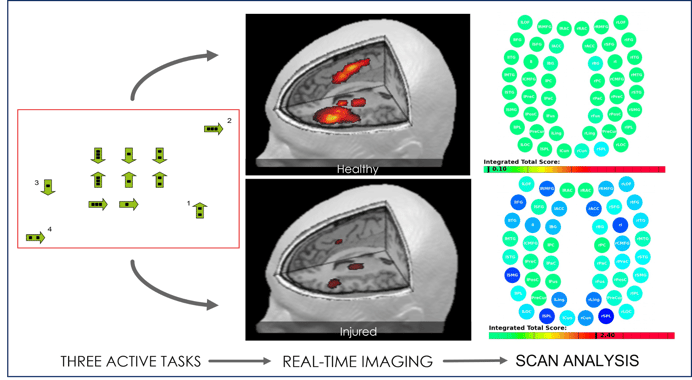
Once these exams are done, our team combines all the information and designs a treatment plan customized for each patient.
From my first day to my last day of my one week treatment at Cognitive FX I felt welcomed and relieved that I was finally getting the help I needed. The team at Cognitive FX runs like a well oiled machine. The communication between team members allows for adjustments to be made to your treatment plan instantaneously. The fMRI scans are only a starting point, the hands-on evaluations further fine tune the treatment to your individual needs. After suffering the effects of long Covid for over a year my balance was greatly improved by the last day of treatment and by the time I settled back into work the following week I noticed my stamina had improved as well. I fully expect continued improvement in the coming weeks and months. This was truly life-changing for me. Thank you!!
— Jennifer Hendrickson (via Google review)
During treatment, our therapists use a combination of physical exercise followed by different therapies. Aerobic exercise, usually on a treadmill or stationary bike, promotes blood flow to the brain and triggers the release of chemicals in the brain, including one called brain-derived neurotrophic factor (BDNF). BDNF improves communication between different areas of the brain, helping the brain become more flexible and able to benefit more from subsequent therapy.
![EPIC Treatment on elliptical [V6]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20on%20elliptical%20%5BV6%5D.jpg?width=1195&height=783&name=EPIC%20Treatment%20on%20elliptical%20%5BV6%5D.jpg)
Cognitive FX treats long COVID in children as well as adults.
Since cardiovascular exercise can be challenging for some post-COVID patients, our therapists closely monitor heart rate and symptom progression. They will modify the recommended exercise and intensity based on your situation to make sure you obtain the benefits of exercise without burning out too soon.
After exercise, patients engage in a variety of multidisciplinary therapies, including:
- Cognitive therapy
- Sensorimotor therapy
- Neuromuscular therapy
- Dynavision therapy
- Occupational therapy
- Neurointegration therapy
- Vision and vestibular therapy
- Psychotherapy
- And more
While most patients receive all of these therapies during their treatment, the way in which they’re used is personalized for each patient. Each patient is given a unique combination of exercises with emphasis on the skills and brain regions they need assistance with.

Many people experience breathing problems post-COVID (most likely caused by dysfunction of the autonomic nervous system), so an important part of our treatment is to teach these patients a variety of breathing exercises. This is done in combination with extra cardio sessions to encourage the parasympathetic nervous system (PNS) to become better regulated, neutralizing the dominance of the sympathetic nervous system (SNS). These exercises “retrain” the brain and body, allowing both SNS and PNS to work together to respond to what the body needs.
Throughout the treatment, patients also have multiple opportunities to rest so their brains can recover before the subsequent therapies. These periods may include a neuromuscular massage to the neck and shoulders, mindfulness exercises, or sitting in a dark room listening to binaural beats, which encourage relaxation and decrease anxiety.
At the end of treatment, we reassess the patient's physical and cognitive performance and administer a second fNCI. This helps us assess the patient’s progress and guides our recommendations going forward. It’s important to note that treatment at our clinic is only the beginning; recovery must continue at home.
![EPIC Treatment exercise with headphones [V1]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg?width=2265&height=1425&name=EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg)
At the end of his treatment, Cognitive FX patient Boston Sharp shared, “I was really happy because I felt like me again. This is super cliché, but I felt like me. And it was the greatest feeling that I was back.”
You can read more about the Sharp family’s road to post-COVID recovery here.
Each of them had work to do at home, but the fundamental healing they needed to experience had begun to take place.
Supporting our patients after treatment is an important part of our approach. Before leaving us, patients meet with one of our therapists to discuss their results and receive a series of exercises to do at home. This typically includes physical exercises, cognitive activities, visual and vestibular exercises, and relaxation techniques. It usually takes an hour or less five times a week and can be reduced as your symptoms improve. If our therapists feel that the patient may benefit from further therapy, we offer referrals to suitable specialists.
Of the COVID long-haulers who meet our screening criteria, over 90% show improvement after treatment at our clinic. Our long COVID patients report over 40% decrease in symptom severity in 13 symptoms after just one week of multidisciplinary therapy. To discuss your specific long COVID symptoms and whether you’re eligible for treatment at our clinic, schedule a consultation.
What to Do at Home
In addition to seeking medical assistance to treat your long COVID symptoms, there are many ways to speed up your recovery with simple lifestyle changes, such as engaging in regular exercise or following a healthy diet. Here are a few of our suggestions.
1. Follow a Healthy Diet

Following a healthy and balanced diet can help your body recover faster.
To help long-haulers, some studies recommend the Mediterranean diet as a way to reduce inflammation, which is believed to be behind many of the symptoms of long COVID. This diet focuses on foods known to reduce inflammation, such as green leafy vegetables, nuts, fatty fish, and fruits such as strawberries and blueberries, while avoiding foods that trigger inflammation, such as fried foods, refined carbohydrates, sugar, red meats, and processed meats.
Be cautious about specific diets you may see advertised online, which can be extremely restrictive and cause nutritional deficiencies. One example is the low histamine diet, which is supposed to control inflammation and reduce COVID symptoms. However, there is no evidence to support these claims, and given the lack of evidence, we think the risks outweigh the potential gain for most patients.
When in doubt, find a licensed and reputable nutritionist or a registered dietician, ideally someone who is already working with long COVID patients, to assist you in your recovery meal planning.
What Can Help My Sense of Smell and Taste?
Some patients experience changes in or loss of smell and taste after a COVID infection. Adding strong flavors to your food may help. Some patients find that eating foods with different textures makes meals more interesting. Others prefer to eat cold foods, which may taste better.
What Can I Do to Help My Gut Health?
Many long-haulers experience digestive issues, including feeling sick, bloating, pain, and diarrhea. Eating plenty of fiber-rich foods, such as fruit, vegetables, nuts, seeds, beans, pulses, and whole grains can help. Probiotics may also be a good option, although there is no hard evidence that these can support long-haulers. If these symptoms persist, speak to your doctor as it’s important to rule out other causes of gastric distress, such as celiac disease.
Should I Take Vitamin and Mineral Supplements?
Vitamin D is vital for the immune system to be fully functional. If you have little or no sunshine exposure due to long COVID, your doctor may advise you to take vitamin D supplements. Some patients with long-term COVID believe high doses of vitamins, such as niacin (vitamin B3), vitamin C, vitamin D, quercetin, and zinc will help with common symptoms. There is no evidence to support these claims, and taking high doses can actually be harmful to you. If you want to take vitamin supplements, read more in our article about natural long-COVID treatments.
2. Engage in Regular Exercise
Long COVID can drastically reduce your ability to engage in physical activity. This is worse than just deconditioning associated with a period of inactivity, and many patients struggle to begin exercising again and to get back to their pre-COVID levels of fitness. This situation is called post-exertional malaise, and it’s classed as a symptom associated with long COVID.
Nevertheless, going back to regular exercise can help with your long COVID symptoms. It’s important, however, to follow the right approach to avoid triggering symptoms and worsening your condition. You need to structure your exercise plan based on the severity of your symptoms rather than following a standard exercise program that consistently increases in intensity over time. Your progress is not going to be consistent all the time, and sometimes, you may need to reduce the amount of exercise you’re doing and prioritize rest.
In addition, exercise doesn’t have to be something very difficult. Start with whatever you’re capable of, even if it’s just 10 minutes of yoga. You can slowly build up with longer and more demanding regimens. Once you’re further along in your recovery journey, you can try a combination of endurance and strength training. These exercises are ideal to improve muscle strength, which is known to decline during a COVID infection and recovery. Exercise also improves respiratory and cardiovascular fitness, reduces fatigue and shortness of breath, helps with post-acute muscle aches, and boosts quality of life.
3. Challenge Your Brain
Patients with long COVID experience many cognitive symptoms, including deficits in attention, executive functioning, language, processing speed, and memory.
For these patients, engaging in cognitive activities strengthens brain function and reduces cognitive symptoms, but only if the games and activities are challenging. Watching TV is unlikely to provide any benefit, but trying to drive home via a different route can help with memory and decision making, for example. Virtually any mental activity can help, and the more senses you try to incorporate into your games, the better.
A few examples include:
- Make a list — a shopping list, things to do, or favorite books — and memorize it. An hour later, see how many items you can still remember. Start with easy lists, and gradually make them more challenging. Studies show that this method can help people recall words more effectively.
- Learn to play a musical instrument. Learning complex skills is good for the brain and helps with many cognitive skills, including memory, executive function, and problem solving.
- Do the math in your head. Figure out your change when you’re shopping, or calculate how much to tip without using paper or your phone. Solving math problems has a positive effect on cognition.
- Create word pictures. Visualize the spelling of a word, and then think of other words that begin or end with the same letters.
- If you visit a new place, draw a map of the area from memory. One study looking at the brains of London taxi drivers showed that those who memorized the city map had better cognitive function.
- Start a new hobby that involves fine motor skills to help you with hand-eye coordination. This could include racquet sports, tai chi, knitting, drawing, or painting.
- Engage in regular exercise. This not only helps with fitness and strength, but it also boosts cognitive function. Examples include yoga, golf, and swimming.
See our post on cognitive exercises for PCS for more ideas; they work just as well for long COVID patients.
Further reading: What to do about post-COVID brain fog
4. Keep Socially Active
Due to the nature of the condition, patients with long-term COVID are at a high risk of social isolation. Symptoms such as fatigue, headaches, and brain fog are not very conducive to engaging in social activities, and many patients tend to just stay at home.
Being socially active can help patients recover faster, but it needs to be done in the right way:
- Meet your friends in your house or a quiet cafe, where you don’t have to shout over the music.
- Let your friends know that you may have to rearrange your plans. Your energy levels can fluctuate from day to day or even hour to hour, and you may have to cancel at the last minute.
- If you find attending events in person difficult, at least stay connected with your friends virtually. This way, you can control when and how you engage in conversation.
- Ask for help if you need something. You may need practical help with household chores or a lift to the doctor, or you might just need an ally who can advocate on your behalf when you feel less able to.
- If you can, plan in advance for a social event, especially if it’s a big event with lots of people attending, like a wedding, for example. Planning ahead helps you prepare mentally, allowing you to have a good time within your capabilities.
5. Follow Healthy Sleep Patterns
One of the most common long COVID symptoms involves sleep disturbances. This often leads to fatigue and headaches, as well as low mood or even depression due to lack of sleep.
Getting enough sleep is crucial to your recovery. Various strategies can support better sleep, including:
- Keeping a sleep diary as a way to track information about your sleep and the different factors that influence how well you can rest at night. In the long term, this information can help you follow healthy sleep patterns and could be helpful information for a doctor, if needed.
- Following a strict routine by going to bed and getting up at the same time every day, including weekends and holidays.
- Trying to get some natural light during the day. At least 30 minutes of daylight — ideally in the morning — sets your circadian rhythm and promotes better sleep at night.
- Staying active and engaging in regular physical activity, but not too close to your bedtime.
- Finding a way to relax before bedtime, such as meditating, doing some light stretching, or listening to quiet music.
- Avoiding alcohol and caffeinated drinks in the afternoon and evening.
- Keeping your bedroom clean and tidy, dark, and not too hot. This will make it easier to fall asleep.
If all of these suggestions don’t really help you sleep, see a doctor to review symptoms and gain a fuller understanding of what is causing poor sleep.
Further reading: What to do about post-COVID insomnia
6. Rest Frequently During the Day

If you’re recovering from long COVID, you need to include frequent breaks when you plan your daily activities. Ignoring your symptoms and trying to “tough it out” will just make things worse.
If you’re not sure when you need a break, follow the rule of three. If you’ve noticed that three symptoms have started or are worsening, then you need a break. For example, if you’re feeling a little anxious and dizzy and you have a headache, find a quiet space for a break.
If you’re experiencing a single symptom, but it’s deteriorating quickly, it’s a sign that you need a rest. For example, if your headache started off as mild (level 1), but it’s jumped three levels, and it’s now severe (level 4), you need to get away from what you’re doing.
It’s important to note that you don’t have to take a break every time you experience symptoms. If you’re just feeling slightly nauseous, or you’re feeling a little “foggy,” it’s OK to continue your activity. In fact, this helps the brain heal and can help reduce other symptoms in the future.
If you work for long hours on the computer, the 20-20-20 rule may be helpful. The rule is easy to follow: Every 20 minutes, look at something that is 20 feet away for 20 seconds. You don’t need to be exact with the distance; the aim is to shift your focus from the computer (closed) to what’s outside (far away). You can just look out a window or go for a quick walk outdoors.
Even as you recover and start to manage working without triggering symptoms, it’s still advisable to take regular breaks. Simply set hourly reminders on your phone to know when it’s time for a break. When your phone beeps, stop what you’re doing and take a break.
These breaks don’t necessarily mean doing nothing (though they can). You just need to give your brain a rest from what you were doing and do something else. For example, you can:
- Go outside on short walks.
- Walk away from your computer for a few minutes.
- Take a power nap. Ideally, no more than 30 minutes and early in the afternoon to ensure that it doesn't affect your sleep at night.
- Take a few deliberately slow and deep breaths.
- Draw or doodle on a piece of paper.
Of the COVID long-haulers who meet our screening criteria, over 90% show improvement after treatment at our clinic. Our long COVID patients report over 40% decrease in symptom severity in 13 symptoms after just one week of multidisciplinary therapy. To discuss your specific long COVID symptoms and whether you’re eligible for treatment at our clinic, schedule a consultation.
7. Pace Yourself During the Day
Many long-haulers complain of fatigue during the day. If that’s the case for you, the best way to cope with this symptom is to pace yourself. In practical terms, this means working out what activities you can manage without overexerting yourself and gradually building up your activity level from there. This is a tried-and-tested formula: A study involving more than 3,700 long-haulers found that pacing was very helpful for symptom management.
Here are some simple tips for pacing yourself and managing fatigue as you recover:
- Think about the tasks you can manage, and plan your daily routine around them. Make sure you include something you enjoy doing.
- Break difficult tasks into small chunks, and spread them across your week, if possible.
- Once you start to tolerate more, slowly add new activities to your routine. For example, when you exercise, you may begin to go for longer walks.
- Take frequent breaks (see above).
- Do the most challenging tasks when you’re most alert. This could be first thing in the morning or after lunch.
- Don’t try to hide how you’re feeling. Ask for help if you need it. Letting others know when you’re struggling can make things easier at home or work.
Further reading: What to do about post-COVID fatigue
8. Look After Your Mental Health
Long COVID symptoms can be unpredictable. Patients often struggle to go back to work, complete daily tasks, or even go out with friends for social events. It’s not surprising that the long-term effects of COVID-19 can hurt not just physical health, but emotional health too, and that it lowers patients’ quality of life.
Typical signs and symptoms can include:
- Sadness
- Worry
- Low self-esteem
- Frustration
- Anger
- Feelings of hopelessness
- Feeling tired or lacking energy
- Not being able to concentrate on everyday things
- Eating for comfort or losing your appetite
- Sleeping more than usual or being unable to sleep
If you’re experiencing any of these, there are things you can do to manage your symptoms:
-
Look after yourself: Simple lifestyle changes can have a big effect on your mental health, including eating a balanced diet, engaging in regular exercise, and getting enough sleep.
-
Keep an active social life: Reach out to family and friends, and arrange to meet them in person or at least speak with them on the phone.
-
Take part in meaningful activities: When you feel low, you may not want to do your usual activities. Don’t give up on everything. Choose small activities you can complete that will give you a sense of enjoyment and accomplishment.
- Seek medical help if needed: If you’re still feeling low after a few weeks, it may be time to see a doctor. You may need treatment for depression or anxiety, which may include talk therapies or antidepressants. Cognitive behavioral therapy is especially helpful for post-COVID patients, and it even helps with fatigue reduction.
9. Practice Breathing Exercises

Especially if you have respiratory problems caused by COVID, breathing exercises can help relieve symptoms. Deep breathing exercises can help restore diaphragm function and increase lung capacity. These exercises also help fight feelings of anxiety and stress and promote sleep.
There are many different types of breathing exercises, but these two may be particularly helpful for patients with long COVID:
- Pursed lip breathing: Inhale slowly through your nose, then form an “o” shape with your lips, and blow out quickly through your mouth. The long inhalation increases levels of oxygen in the lungs, and the quick exhale forces out carbon dioxide.
- Diaphragmatic breathing: Breathe in through your nose while you count to four, pause while you count to two, then slowly breathe out through your mouth while you count to six. If you place your hand on your stomach, you can feel it pushing as you inhale.
Further reading: Post-COVID shortness of breath
10. Quit Smoking (and Vaping)
If you smoke (or vape), one way to reduce the severity of your symptoms during long COVID is by quitting. Several studies have shown that smoking increases the risk of developing long COVID and aggravates respiratory symptoms. This is not surprising given that smoking causes a wide variety of health problems, including lung disease, cardiovascular problems, and a poor immune system.
The good news is that once you decide to quit, the benefits for your body are almost immediate. You will notice how your lung function improves and associated health conditions become less severe.
Tips to look after your lungs:
- Don’t smoke (or if you do, quit). There are many options to help you quit. Our advice is to speak to your family doctor.
- Avoid areas with high pollution.
- Learn breathing exercises.
- See your doctor if you develop new chest symptoms or your symptoms worsen.
11. Consider Returning to Work/School
It may appear counterintuitive, but one way to speed up your recovery from long COVID is to return to work (or school), even before all your symptoms have subsided.
A good time to return to work could be when:
- Your symptoms have stayed the same for a while or even improved slightly.
- You can manage your symptoms during the day (with frequent rests, for example).
- You can carry out normal everyday activities, such as getting dressed and cooking a meal, without your symptoms getting significantly worse.
Discuss Your Return With Your Employer
If you have been off work due to long COVID and feel that you’re ready to go back to work, the first step is to meet with your employer. At this meeting, you can explain your current symptoms and what you still find hard to do. You may also want to discuss a phased return or a lighter workload as you slowly build back up to what you used to do. Coordinate with your healthcare professional as well; they can help you determine what’s realistic and make a plan for what to do if your symptoms are too oppressive.
Possible adjustments include:
- Extra support to do your job
- Time off to attend health appointments
- Shorter working days
- Working from home with virtual appointments
- Frequent breaks
- Changes to workload with fewer or less complex tasks
12. Give Yourself Time to Recover

Finally, recovery takes time. It’s not a linear process. You might have a good day or even three good days, but that’s no guarantee that you won’t then have a hard day and need a little extra give in your schedule to recuperate. This doesn’t mean you’re not improving over time.
That said, if you’re having more bad days than good days, you may be overexerting yourself. Rethink how much you can do each day.
Also, remember that long COVID can happen to those whose initial illness was entirely mild, not just to those who suffered severe COVID-19 needing intensive care and constant monitoring of their flagging oxygen levels. Post-COVID conditions can develop in anyone. If you feel alone in your journey to return to normal daily life, look for local and online support groups.
Want the support of a seasoned, multidisciplinary long COVID treatment team? Schedule a consultation to see if we can help.

![oxygen therapy in hyperbaric chamber [V6]](https://www.cognitivefxusa.com/hs-fs/hubfs/oxygen%20therapy%20in%20hyperbaric%20chamber%20%5BV6%5D.jpeg?width=1000&height=559&name=oxygen%20therapy%20in%20hyperbaric%20chamber%20%5BV6%5D.jpeg)



![EPIC Treatment on elliptical [V6]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20on%20elliptical%20%5BV6%5D.jpg?width=1195&height=783&name=EPIC%20Treatment%20on%20elliptical%20%5BV6%5D.jpg)

![EPIC Treatment exercise with headphones [V1]](https://www.cognitivefxusa.com/hs-fs/hubfs/EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg?width=2265&height=1425&name=EPIC%20Treatment%20exercise%20with%20headphones%20%5BV1%5D.jpg)