Neurofeedback is a confusing topic for patients to decipher on their own. Many clinics use big words and brief explanations, and they claim that neurofeedback can cure any number of conditions, from ADHD to post-concussion syndrome.
Are those claims true? Are they backed by good science? That’s what we intend to tackle today.
We cover:
We’ll go in-depth on the science and reasoning later in this post, but here’s the overview:
Neurofeedback is helpful if you struggle with anxiety, post-traumatic stress disorder (PTSD), or obsessive-compulsive disorder (OCD). It can help with depression if you frequently have intrusive thoughts. To the extent that neurofeedback helps with anxiety and promotes a relaxed brain, it is very helpful. But it is not a cure for post-concussion syndrome (PCS), and it cannot be used to identify which brain regions were affected by the injury and how.
Neurofeedback is a great tool for what it was originally designed to do: calm the brain and give it a break from stressors. While you can go to a clinic for neurofeedback, you can also get an at-home neurofeedback device (like the Muse™ headband) or use a Brainwave phone app to achieve a similarly relaxing, meditative effect.
If you truly want to recover from post-concussion syndrome, a neurofeedback clinic is not the answer. We talk later in this post about what kind of therapy works for post-concussion syndrome and how to find a good treatment clinic. Post-concussion syndrome is caused by dysfunctional neurovascular coupling (NVC), which is the connection between your neurons and the blood vessels that supply them. The most effective treatment re-establishes healthy neurovascular coupling. You can read more about post-concussion syndrome and how we image it via the linked posts.
We’ve treated thousands of mild traumatic brain injury (mTBI) patients at our clinic, and we want to see the very best outcomes for them. In the past, we used neurofeedback to help patients rest in between therapy sessions (but have since switched to more effective options) and have deep expertise in the mathematical analysis needed to conduct and interpret the results of electroencephalography, the technology used in neurofeedback. We’ve drawn on that knowledge to provide as accessible a description as we can here of how it works and when it can help patients.
If you suffer from long-lasting symptoms after a concussion or other brain injury, you’re not alone. Up to 30% of concussion patients develop lingering symptoms that don’t go away without treatment. 95% of our patients experience statistically verified restoration of brain function. To learn if we can help you, sign up for a consultation with our team.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
How Does Neurofeedback Work?
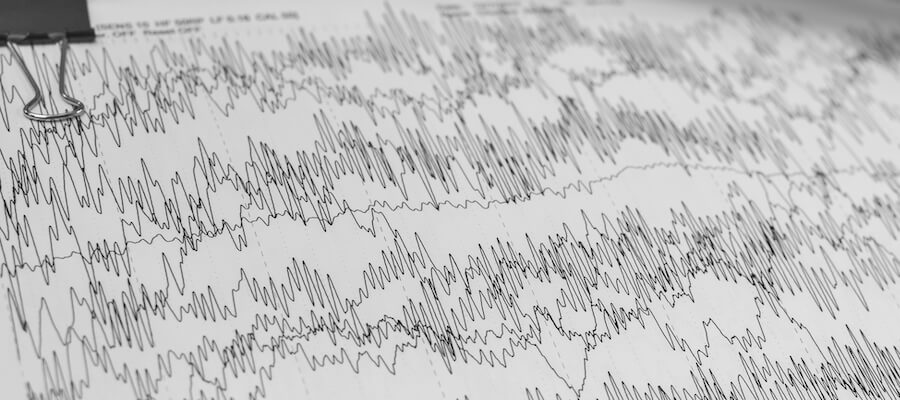
Neurofeedback uses electroencephalography (EEG, which also stands for the graph output: an electroencephalogram) to promote healthier brain waves.
EEG uses electrodes placed around your head to pick up a change in electrical charge (called potential) whenever neurons fire. Neurons don’t fire one by one; they fire in clusters while executing some task. That way, even if one neuron fails, your brain can still accomplish the task it set out to perform. So any signal picked up by an EEG represents bundles of thousands of neurons firing from different areas around your brain. That signal is a conglomerate of brain activity.
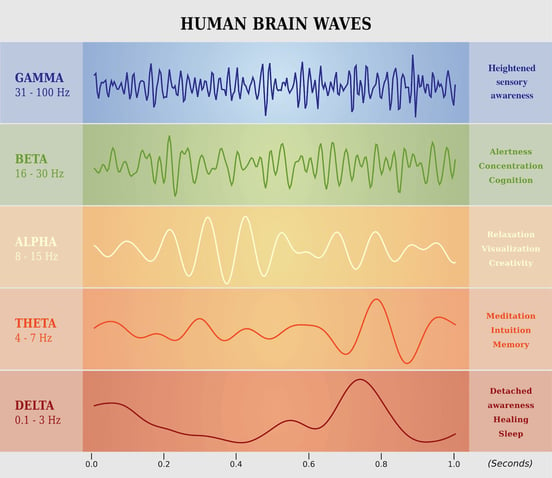
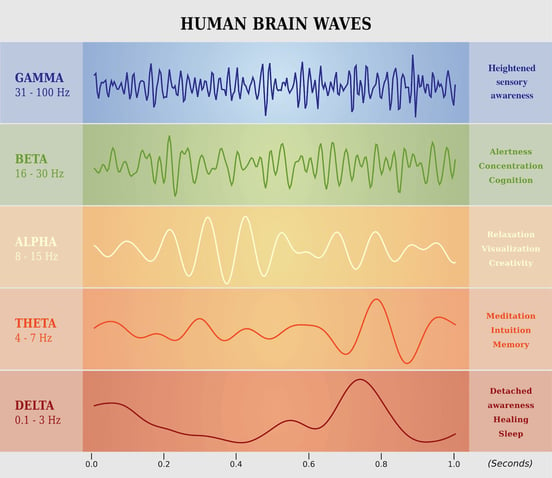
EEG’s are readable because neurons don’t just fire randomly. They fire rhythmically. So we can use EEG to monitor that rhythm, which produces overarching patterns (brain waves) that we can recognize (specifically, gamma, beta, alpha, theta, and delta). Delta waves (under 4 Hertz) are associated with sleep. Beta waves are associated with attentive actions like reading or conversing. Alpha waves are characteristic of a meditative state: alert, but resting.
Neurofeedback looks at those waves and uses an audible or electrical signal to indicate whether you’re getting closer to or further from a desired wave state. For example, at our clinic, we used to have patients use a Muse™ device to relax in between active therapy appointments. The patient would sit in a quiet room. The device we used had you imagine you were sitting on the beach (and provided some beach sounds to help).
If your brain was too active, the waves would be in beta or gamma range and the device would play the sound of seagulls calling to each other. As you relaxed, the bird calls would become fainter. So you would iterate toward a dominant alpha wave state. The device also provided some cues for breathing to help you relax.
Neurofeedback is a type of “brain training” to achieve a meditative state, even in people who have difficulty meditating.
Note: Some online resources and treatment programs treat neurofeedback and biofeedback as the same thing. They are similar; some say neurofeedback is a type of biofeedback. Biofeedback is the use of electrical signals alongside techniques like breathing and progressive muscle relaxation to help you gain control over involuntary biological processes. For example, it might help you relax chronically tense muscles or calm an overly high heart rate. Some therapy types include heart rate variability biofeedback (hrv), thermal biofeedback, and electromyogram biofeedback (for muscle activity/tension). Neurofeedback is used to help you regulate your brain waves. This post is focused exclusively on neurofeedback.
Can Neurofeedback Help Patients Recover from Post-Concussion Syndrome?
Claims that neurofeedback training can cure a head injury, or even cause a significant improvement in symptoms, are based on the notion that you can use an EEG reading to tell what brain wave frequencies (gamma, beta, alpha, etc.) are coming from specific areas of the brain. Unfortunately, that’s just not true.
However, neurofeedback is excellent for folks who suffer from anxiety (whether or not it’s caused by injury). And it’s helpful in overcoming brain fatigue in post-concussion syndrome. Here’s why.
How Neurofeedback Helps the Brain Rest

Remember how neurons fire in certain rhythms? The brain uses all kinds of neuron firing patterns. How often a neuron fires in the span of a second is the frequency of firing. For example, you might have a cluster of 10,000 neurons in part of a network used for memory encoding firing 12 times per second (12 Hertz, or Hz). When you plot that frequency on a graph, you get waves.
Neurons fire at different frequencies based on what kind of task they’re doing. Memory encoding doesn’t take the same frequency as understanding the words on a page, so an EEG’s reading is getting different frequencies from different locations around the brain, since those tasks occur in different areas.
If nothing interferes, they’ll carry on as they always do. But alpha waves are particularly interesting. If your brain produces alpha waves in one area, those alpha waves will “entrain” nearby neuron clusters to an alpha state as well. It can literally take over your brain! That sounds a little scary, but it’s actually helpful: It gives your brain a break.
Think about it: If you have ruminative or intrusive thoughts, those thoughts are being fueled by some clusters of neurons. If those neurons get taken over by alpha waves, they can’t produce the thoughts that are so frustrating for you to experience. Those neuron clusters that were figuring out your meal plan for this week? Or the ones worried about why your boss wants to talk to you? They have to give it a rest.
This is why meditation is a popular solution to anxiety: It won’t fix everything, but it will give your mind a rest. And combined with other efforts, that can give you the breathing room you need to make a more pronounced recovery.
But not everyone is good at meditation. That’s where neurofeedback comes in: It gives you real-time indicators of how close or far away you are from a meditative state. When used for anxiety or even just giving your brain a break (which is especially important for any TBI patient, since patients’ brains often get overwhelmed), neurofeedback sessions are helpful. That relaxation is also good for your autonomic nervous system. But that’s where its usefulness ends.
Why Neurofeedback Can’t Cure PCS
After seeing how great neurofeedback was at teaching patients how to encourage alpha waves, some people in the medical community started looking at other brain waves. What if you could train beta waves? What if you could identify issues like ADD? What if you could point to one brain region and say it’s not functioning right? What if it could unlock heightened cognitive performance?
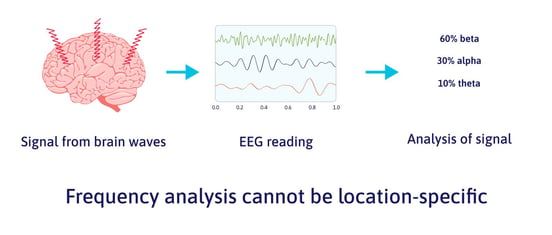
But neurofeedback therapy is not the wonder method that some hoped it would be (and that some clinics still claim it is). The reason it’s not viable in those applications is something called source localization. Using source localization (a complex mathematical process), you can isolate a signal from one region of the brain at a specific instant in time. So you can look at EEG data and say, “We picked up a signal from the prefrontal cortex,” for example.
But what you can’t say is something like, “We detected abnormalities in your thalamus. It’s producing too many beta waves.” Why? Because source localization only detects signal location from a moment in time. But to analyze a signal and pick out the contributing frequencies (which come from all over the brain and not a single location), you need a sample over time.
In other words, the EEG analysis we have available can either:
- Determine where the wave came from, or
- Determine what frequencies were in the signal detected (since each neuron cluster contributing to the total signal may have a different frequency).
In short, you can’t localize frequency.
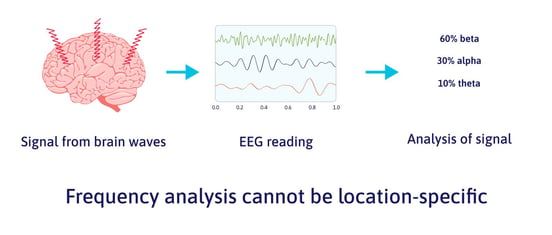
But that’s exactly what providers of neurofeedback for concussion claim to do with “quantitative” EEG (qEEG). There’s no doubt that they are measuring brain signals; there’s also no doubt that they are incorrectly interpreting the data.
Now, is it possible that you could discover a connection between oddly high beta waves and OCD, or some such condition? Certainly. But you can’t prove the connection without establishing a norm (think: bell curve distribution of normal people) and then showing that the condition in question regularly includes people who are more than one standard deviation outside the norm. Providers of neurofeedback have not done that work. Nor have they identified biomarkers (reproducible indicators of a specific condition) for post-concussion syndrome or many of the other neurological disorders they purport to treat.
Despite all that, some treatment providers use neurofeedback in an attempt to train brain wave types other than alpha. The claims you see from a neurofeedback clinic offering a cure for post-concussion syndrome are not backed by solid science. While some people in case studies may experience an improvement (due to some happy accident, other therapies, or the placebo effect), it’s not because neurofeedback itself is a reliable technique for that purpose.
Alternatives to Neurofeedback for Concussion Patients

At-home neurofeedback devices like the Muse™ are always an option if you’re looking for an aid to meditation or relief from some anxiety symptoms.
Note: There are other brands on the market besides Muse™, but we’ve never used them, so we can’t make other recommendations. We will not receive any monetary compensation if you use the link to purchase the Muse™; we just want you to know it’s available.
All that said, if you just need your brain to calm down, there are cheaper ways to do it than to go to a clinic or purchase a Muse™ device. And if you want to recover from PCS, you’ll need more than just periodic rest for your brain. We cover both in this section.
Brainwaves
In our clinic, we’ve used both the Muse™ headband (neurofeedback) and binaural beats (called Brainwaves).
While the Muse™ headband requires you to adjust your thought patterns consciously, Brainwaves will induce alpha waves for you. Here’s how it works:
When you listen to a Brainwaves app, it puts one frequency in each ear. The two frequencies are very close, but not the same. There’s nothing like it in the real world, so our brains can’t make sense of it immediately. Instead, your auditory cortex sends the signal to your thalamus, which then reinterprets the two frequencies as one. But when you average them together, they’re the same frequency as an alpha wave. So the audio induces a specific type of brain wave (a process called entrainment).
Remember how alpha waves induce more alpha waves? When you listen to Brainwaves, it causes your brain to start making alpha waves, which then spread to other parts of your brain.
It’s affordable (a similar app is free on Android, or $5 on iPhones for the one we use), and for most people, it works more quickly than neurofeedback to induce alpha waves. We found that Brainwaves worked a little faster and better at helping patients rest and recover before their next therapy session. There were always a few people who liked neurofeedback better, but the majority were helped more by the Brainwaves, which is why we now only use Brainwaves. The only downside is that you’re always reliant on technology to induce that brain state instead of learning how to get there on your own.
To learn more about how Brainwaves helps and what to try at home, see our video on the topic:
Remember: Alpha waves are good for everybody! Even if you have a healthy brain, it’s good to give it a break. And if you have post-concussion syndrome, regularly reaching an alpha wave state will help decrease symptom severity because it gives an overtaxed organ the chance to relax.
Note: We don’t receive any financial compensation for the links above; we simply think that the Brain Wave™ 35 Binaural Series is the best one available, which is why we use it with our patients.
Physical & Cognitive Therapy

After a concussion, the brain will route resources like oxygen around injured sites to areas that are still functioning normally. For patients who have lingering post-concussion symptoms, that distribution of resources (neurovascular coupling) doesn’t return to normal after the brain heals from acute injury. The result is that some brain regions shoulder more than their fair share of the work, while other regions don’t do the work they’re supposed to do. We can see those specific brain regions using functional neurocognitive imaging (fNCI), a special type of functional MRI. You can read more about how fNCI works here.
At CognitiveFX, we use your imaging results to inform therapy. Imaging shows us which regions were affected and whether they’ve become hypoactive (not doing enough) or hyperactive (doing too much) since your injury. We then tailor our multidisciplinary therapy regimen to engage those brain regions.
Some of the therapies we employ include cognitive therapy, occupational therapy, neuromuscular therapy, cardio exercise (even for folks who find it difficult to exercise after head trauma), sensorimotor therapy, neurointegration therapy, Dynavision therapy, and more.
These therapies challenge the brain and push it to return to healthier ways of handling cognitive and physical demands.
For example, an exercise that challenged our patient Samuel Gray was balancing on the flat side of a Bosu ball while a therapist had him name a fruit for every other letter of the alphabet, beginning with the letter Z and going backward… all while they tossed a football back and forth.
“The point is that you're occupying the parts of your brain that, at least in my case, I had mapped around and was supposed to use for balance and catching but that I was using for things like word retrieval as well as balance. But I wasn't using the correct part of my brain for word retrieval and memory. So that exercise was forcing my brain to use the correct parts,” he said. “Doing that is very difficult when you haven't used those parts of your brain in 33 years!”
You can read more about what therapy is like from these patients:
Conclusion
The point of this piece isn’t to say that all neurofeedback is bad. Neurofeedback is great for helping anxiety, OCD, and PTSD; getting your brain to relax; and learning how to meditate.
But neurofeedback is not good at fixing concussion symptoms such as brain fog, memory problems, difficulty concentrating, sleep disorders, and so forth. And it certainly can’t fix physiological symptoms like blood pressure dysregulation or nausea.
For comprehensive concussion care, you’ll need different treatment. You can use our guide to finding a good concussion clinic near you.
If you’ve been suffering from post-concussion syndrome for more than three months, we invite you to schedule a consultation with our team to help you decide what’s next in your recovery journey.