Can Post-Concussion Syndrome Cause Stuttering?
Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY

Returning to work after a concussion—especially if you’re still experiencing symptoms—can be a difficult and uncertain process. There’s no one-size-fits-all answer. For many patients, it’s possible and even beneficial to begin working again before they’re fully recovered, as long as they can safely manage their post-concussion symptoms.
This article offers general advice for returning to work or school after a head injury. We’ll cover what to expect, how to pace yourself, and what to do if your symptoms get in the way.
Table of Contents
Every patient’s return-to-work (RTW) timeline is unique.
Mild cases: Most patients with a mild traumatic brain injury (mTBI) recover within a few days to weeks and can return to work relatively quickly.
Persistent symptoms: Around 30% of concussion patients develop long-lasting symptoms, a condition called post-concussion syndrome (PCS), which can significantly lengthen recovery time. Many struggle to return to work, and about two-thirds never recover enough to go back with the same abilities they had before. A small proportion are never able to go back.
Note: If you’re in this group, personalized multidisciplinary post-concussion treatment can help. Learn more here.
If your symptoms persist, it’s essential to seek support from a medical professional experienced in brain injury rehabilitation. You may need a return-to-work plan that includes part-time hours, modified duties, and regular follow-up with your medical care team.
There’s no perfect moment—but a good sign is when you can complete cognitive activities or physical tasks for a sustained period without a spike in symptoms. Your job duties also play a role in determining readiness.
For example:
If your work activities involve physical labor, driving, or climbing ladders, returning while experiencing dizziness or balance issues may put you at higher risk for reinjury.
If you work in an office or remotely, easing back into shorter work days with flexible hours may be safer.
Remote work also allows more control over your environment—including limiting screen time, reducing noise exposure, and taking brain breaks as needed.
Many patients with traumatic brain injuries struggle with symptoms that interfere with both work-related activities and activities of daily living.
Some of the most common include:
Fatigue: Affects mental clarity, alertness, and decision-making.
Headaches and migraines: Make it hard to concentrate and can increase the risk of errors.
Emotional symptoms: Anxiety, irritability, and stress may be worsened by work pressure or concerns about job performance.
Cognitive challenges: Trouble with memory and focus can affect time management and learning new tasks.
Vision problems: Blurry or double vision can interfere with screen-based tasks or operating equipment.
Vestibular dysfunction: Dizziness and balance issues may limit standing, walking, or working in certain environments.
All of these symptoms can delay your return and should be closely monitored throughout your recovery process.
The safest and most effective approach is a gradual return—ideally guided by a healthcare professional or occupational therapist who works with TBI patients.
Begin with a light cognitive load and short shifts. Focus on emails, reading, or low-pressure tasks. If you’re not quite ready for paid employment, volunteering can be a helpful stepping stone to rebuild cognitive and physical capacity.
Expand your work day as tolerated. Continue to take breaks and limit overstimulation. Ask for extra time when needed to complete tasks safely.
As your symptoms subside and cognitive function stabilizes, you can gradually return to a full-time work schedule and your normal responsibilities.
They can help assess whether you’re ready and advise on workplace adjustments. Patients with moderate to severe TBI cases may also benefit from consulting with specialists experienced in complex brain injury rehabilitation.
You may be eligible for workplace accommodations under the Americans with Disabilities Act (ADA). A diagnosis alone doesn’t guarantee these—you’ll need proper documentation and a medical evaluation.
It’s crucial that you communicate with your employer about your condition. It can be helpful to provide them with resources explaining what post-concussion syndrome is, the symptoms you’re dealing with, and how they’re triggered.
You may need to advocate for yourself and ask for modified duties, reduced hours, or flexible schedules. A flexible work environment and supportive supervisor can make a big difference.
Minimize screen time, reduce noise and light exposure, and take regular breaks. Consider ergonomic adjustments to your workspace if physical discomfort is a trigger.
Keep a journal to spot patterns and triggers. Bring this to follow-up appointments with your doctor for better care planning.
Recovery isn’t linear. Some days will be better than others. Take care of your well-being and don’t hesitate to slow down or reduce working hours if your symptoms return.
Most patients with post-concussion syndrome (PCS) are eager to return to work—often due to financial obligations, pressure from family members, or concerns about missing out on career growth and opportunities.
The most effective way to get back to work safely and confidently is to treat the root cause of your symptoms. By restoring normal brain function, you can preserve your existing skills and re-enter the workplace with greater stability and independence.
That’s exactly what we help our patients do at Cognitive FX.
At Cognitive FX, we treat the neurological dysfunction at the heart of persistent post-concussion symptoms and other mild traumatic brain injuries. Our rehabilitation program is designed to address the root cause of your symptoms—rather than treat individual symptoms in isolation.
Our treatment, Enhanced Performance in Cognition (EPIC), is an intense, individualized program targeting each patient’s specific physical, cognitive, and emotional symptoms.
Our treatment process begins with an in-depth evaluation, which includes:
A meeting with one of our doctors to review the patient’s medical history and symptoms of post-concussion syndrome.
A physical exam to check balance, hand-eye coordination, reaction times, and other physical abilities.
A psychological evaluation to identify symptoms of anxiety, depression, and other mental health problems.
A structural brain and cervical spine MRI to spot any serious structural injuries that need medical treatment before patients start with us.
A brain imaging scan called Functional Neurocognitive Imaging (fNCI) to determine where and how the patient’s brain was affected by the injury.
Instead of strictly conducting interviews with the patient about their symptoms, as you’d experience at most concussion clinics, we use an advanced fMRI scan to pinpoint exactly where the brain is showing signs of dysfunction.
We use Functional Neurocognitive Imaging (fNCI), which measures two key things:
Regional brain activity: How much oxygen each brain region uses during specific cognitive tasks (indicating underactive, normal, or overactive function).
Connectivity between regions: How well different parts of the brain communicate with each other.
The scan results are visualized through intuitive charts and brain maps that help us identify whether a patient is experiencing hypoactivity (under-functioning), hyperactivity (over-functioning), or a mix of both—and where.
This detailed view of brain function allows us to tailor each person’s therapy precisely.
For example:
Someone with hypoactivity may need therapies that target various brain regions with stimulation and cognitive endurance training.
Someone with hyperactivity may benefit from therapies that reduce neural “noise” and promote regulation.
We’ve organized scan results for regional activity into six clear cognitive domains—like memory, attention, and executive function—to make them easier to understand and better guide individualized treatment.
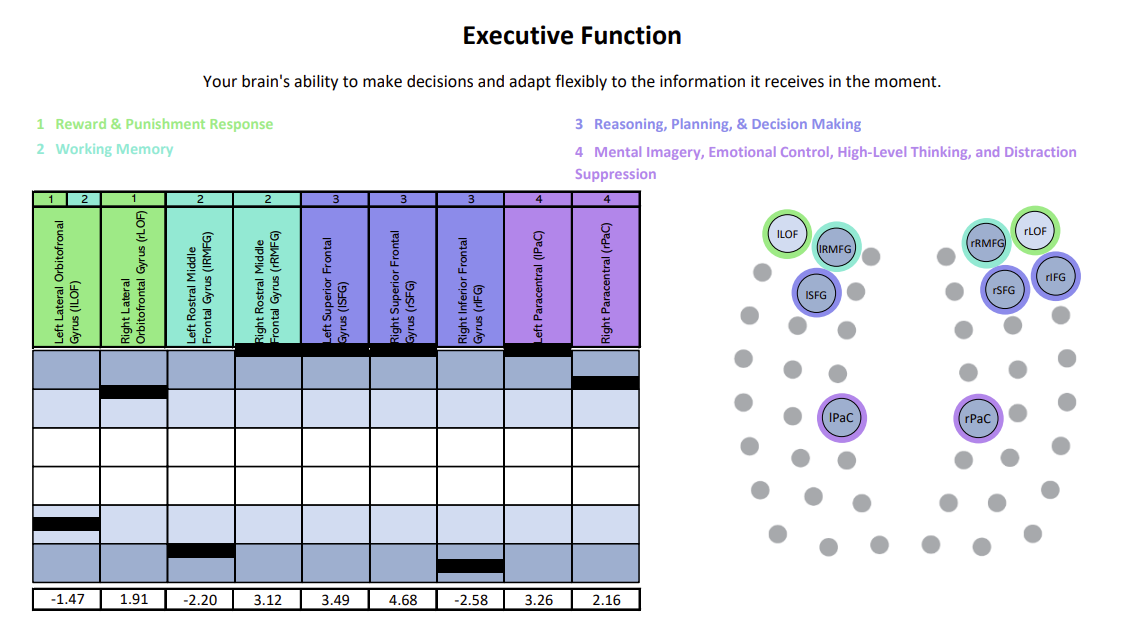
Each chart shows how specific brain regions are functioning compared to a normal brain. The white area represents the normal range, with the center line marking the average. Light and dark blue zones show increasing levels of abnormality.
A black line marks the patient’s result for that region—ideally landing within the white. Lines in the light and dark blue zones suggest that region is either hyperactive (blue zones above the white) or hypoactive (blue zones beneath the white).
In this example, the patient was experiencing both hypoactivity and hyperactivity within different key regions linked to executive function.
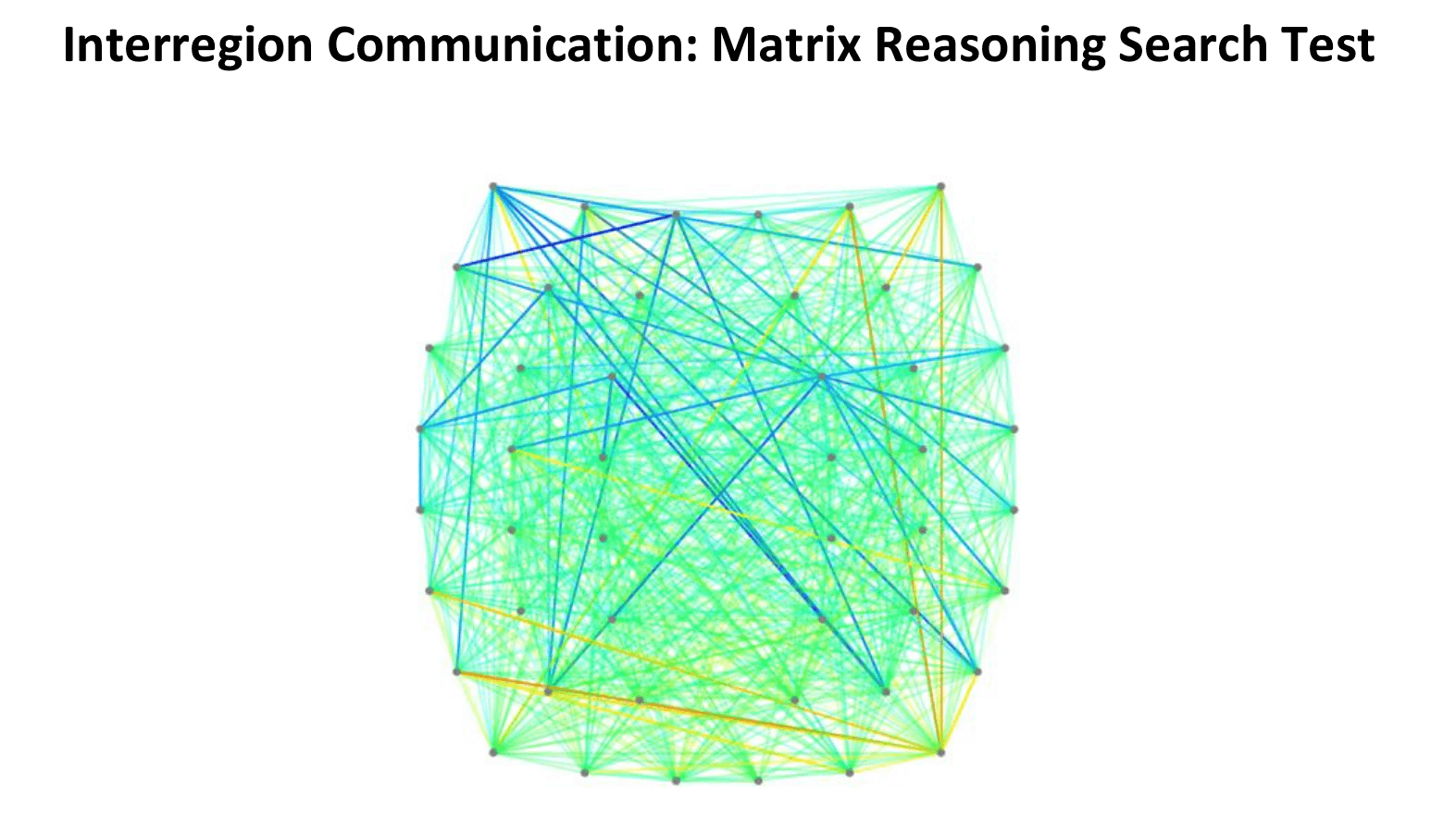
In this connectivity map, cooler colors (blues) indicate areas of hypoactivation (underactivity), while warmer colors (reds, oranges, yellows) indicate areas of hyperactivation (overactivity).
After patients complete this evaluation, our team designs a personalized treatment plan targeting the exact areas of their brain showing dysfunction.
We offer one- and two-week treatment plans based on symptom severity. Daily treatment involves a three-step cycle that repeats: Prepare, Activate, and Recover.

Therapy starts with short bursts of aerobic exercise, usually on the treadmill or stationary bike. Exercise triggers the release of important chemicals in the brain, which help the patient's brain become more flexible and boost the effects of subsequent therapy.
Our therapists are trained to help patients exercise according to their needs without triggering severe symptoms. Even patients who struggle with physical activity due to balance problems can make remarkable progress in these sessions.

After exercise, patients attend a variety of therapies, including:
Patients receive most or all of these therapies during their visit, but each regimen is uniquely tailored.
For greater impact, our therapists often combine exercises from different disciplines.
For example, you might balance on a Bosu ball to engage your vestibular system and brain’s balance center while tossing color-coded tennis balls to work hand-eye coordination and reflexes. Meanwhile, you’ll add or subtract from a running tally based on which ball you catch, challenging memory, problem-solving, and attention.
During neurointegration therapy, you might draw a mirror image of a pattern while answering simple questions from your therapist.
Rest periods are an important part of our treatment. Some examples of scheduled brain breaks include:
Neuromuscular massage: Therapists massage the neck and shoulders to relieve chronic pain and tension, relax muscles involved in vision, improve circulation, and alleviate headache pain.
Brainwaves: The binaural beats app we use produces two frequencies that are very close together. If you listen to a different frequency in each ear, your brain will average them together to produce one frequency. We set the parameters so that the frequency your brain creates is the same frequency you would experience through meditation. This frequency will propagate in your brain waves as you listen. As a result, you gain some of the restorative benefits of meditation without being a meditation expert.
Mindfulness: Patients learn mindfulness techniques during their time at the clinic.
At the end of treatment, patients undergo a second brain imaging scan to see the progress that has been made. They then meet with one of our therapists to review the results and receive a series of at-home exercises. These typically include physical activities, cognitive tasks, visual and vestibular exercises, and relaxation techniques. We recommend patients perform these exercises for about an hour, five times a week initially, with the frequency decreasing as symptoms improve.
For patients needing further therapy, we provide referrals to appropriate specialists.
You may find it helpful to read some of our other patient recovery stories:
Quieren is a Cognitive FX patient from the Netherlands who suffered from PCS after a bike accident.
Sam Gray sought treatment 33 years after a brain bleed.
Myrthe van Boon is a mother of two who struggled with debilitating post-concussion symptoms for years before finding Cognitive FX.
Olivia Seitz is a former figure skater who found symptom relief after more than a decade of chronic illness.
Sam Pembleton was an adolescent hit by a soccer ball in the head; she tried treatment methods for five years before finding Cognitive FX.
These patients all completed video testimonials about their initial injury and their experience at Cognitive FX.
Over 90% of our PCS patients experience significant recovery after treatment in our clinic. To determine if our program is right for you, please schedule a consultation with our team.
Support is available. These organizations can assist with your return-to-work and recovery journey:
Brain Injury Association of America (BIAA): Offers state-specific vocational rehab resources and legal guidance.
National Association of State Head Injury Administrators (NASHIA): Connects patients with public health programs, advocacy groups, and Medicaid Waiver services.
Concussion Alliance: Provides education and practical tips for navigating the workplace with PCS.
CDC Traumatic Brain Injury Resources: Offers tools for patients and employers, including Employee Assistance Programs and federal leave options.
Military Health System’s TBI Center of Excellence (TBICoE): A great resource for veterans and their families navigating post-TBI care and work transitions.
Bottom line: With a careful return-to-work plan and the right treatment, even patients with long-term post-concussion symptoms can regain independence and return to meaningful work. Be patient with yourself, stay informed, and don’t hesitate to seek the support you need.

Dr. Alina K. Fong received her Ph. D. in Clinical Neuropsychology with an emphasis in neuroradiology from Brigham Young University. She received the national American Psychological Association Clinical Neuropsychology Division 40 Graduate Student Research Award in 2004 for her research on "Cortical Sources of the N400 and 'The N400 Effect." Dr. Fong's interest in brain mapping soon turned to functional MRI, and since then, her research efforts have been focused on the clinical applications of fMRI.

Many people associate stuttering with childhood, but a sudden onset of stuttering can also occur after a head injury. This phenomenon, known as acquired stuttering, is one of many symptoms that can...

Severe traumatic brain injury (TBI), concussion (mild traumatic brain injury or mTBI), and other head trauma can cause high blood pressure, low blood pressure, and other circulatory system changes....
Perhaps this sounds familiar: You wake up from a relaxing nap expecting to feel refreshed, but instead, your heart is pounding for no reason. Or you stand up after a few hours on the couch and feel...

Leg weakness after a concussion can significantly impact mobility and daily life. Patients may feel their legs are untrustworthy, worry about falling, or contend with stiffness and fatigue.

Here’s something you probably won’t hear in the emergency room: A transient ischemic attack (TIA, or mini-stroke) can have symptoms that last for months or years afterward.
Many healthcare providers...

Persistent symptoms after a head injury (post-concussion syndrome) can be confusing. They don’t always seem like problems an injured brain should cause. Symptoms like memory problems, trouble...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY