Chemo Brain Treatment: What It Is & How to Recover | CFX
Key Takeaways
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY
When your child's concussion symptoms refuse to go away, every parent faces the same terrifying question: What's happening to my child's brain, and why isn't anyone able to help?
If weeks have passed since your child's head injury and they're still complaining of headaches, struggling in school, or just not acting like themselves, you're not imagining things. And despite what some doctors may have told you, this isn't something your child simply needs to "push through."
Your child may have post-concussion syndrome, a condition that affects between 10% and 30% of children following a concussion. The good news? With proper diagnosis and evidence-based treatment, most children with persistent symptoms can make significant improvements and return to their normal lives.
This guide will walk you through everything you need to know: how to recognize post-concussion syndrome in your child, what the latest research says about recovery, and what treatment options actually work.
In this article:
A concussion is a mild traumatic brain injury caused by a bump, blow, or jolt to the head. In children, the most common causes are falls, sports injuries, motor vehicle accidents, and playground collisions. According to the CDC, emergency departments treat approximately 700,000 children annually for traumatic brain injuries, with falls and sports being the leading causes.
Most children recover from a concussion within two to four weeks. But for a significant percentage, symptoms persist well beyond that window. When concussion symptoms last longer than four weeks in children (or three months using older diagnostic criteria), clinicians diagnose post-concussion syndrome.
What actually happens in a child's brain during PCS?
Post-concussion syndrome isn't about structural brain damage that shows up on CT scans or standard MRIs. In fact, most imaging comes back "normal" in children with PCS, which can be incredibly frustrating for parents searching for answers.
The real problem lies in how the brain functions after injury. Research has identified several key mechanisms:
Neurovascular coupling dysfunction: This is the relationship between neurons (brain cells) and the blood vessels that supply them with oxygen and nutrients. After a concussion, this communication system can become disrupted. Affected brain regions don't receive the right amount of oxygen at the right time, causing them to work inefficiently during tasks like reading, concentrating, or processing information.
Autonomic nervous system dysregulation: The autonomic nervous system controls automatic functions like heart rate, blood pressure, and body temperature. Concussions can disrupt this system, leading to symptoms like exercise intolerance, dizziness upon standing, and temperature sensitivity.
Vestibular and vision system dysfunction: The systems that control balance, spatial awareness, and eye movement are particularly vulnerable to concussion. Research published in the Journal of Sport and Health Science (2025) found that 62% of adolescents with persistent post-concussion symptoms have diagnosable vision disorders, many of which go undetected without specialized testing. [DOI: 10.1016/j.jshs.2025.101058]
Cervical spine involvement: The neck often sustains injury during the same forces that cause a concussion. Neck dysfunction can contribute to headaches, dizziness, and other symptoms that overlap with PCS.
Understanding these mechanisms is crucial because it explains why "just rest" often fails as a treatment strategy and why many children need targeted, multidisciplinary care to recover.
{% module_block module "widget_630732ec-bdaa-4645-aa16-bd80ad0751d4" %}{% module_attribute "child_css" is_json="true" %}null{% end_module_attribute %}{% module_attribute "css" is_json="true" %}null{% end_module_attribute %}{% module_attribute "html" is_json="true" %}"\n\nAnswer a few questions about your child's situation to get a personalized recommendation
\nBased on your answers, your child may benefit from:
\nNeed help understanding your child's symptoms or navigating the school accommodation process?
\n Talk to a Specialist\n
Here's the hard truth that keeps pediatric concussion specialists up at night: most children with post-concussion syndrome are either undiagnosed, misdiagnosed, or given outdated treatment advice that can actually prolong their symptoms.
Many parents hear some version of these frustrating phrases:
Meanwhile, their child continues to suffer, falls further behind in school, and watches friends move on without them.
The 2022 Amsterdam Consensus Statement, the international gold standard for concussion management, fundamentally changed what we know about pediatric concussion recovery. Yet many healthcare providers haven't caught up to the evidence. According to this consensus, the old "cocoon" approach of keeping children in dark rooms with no activity is not only unnecessary but may actually slow recovery.
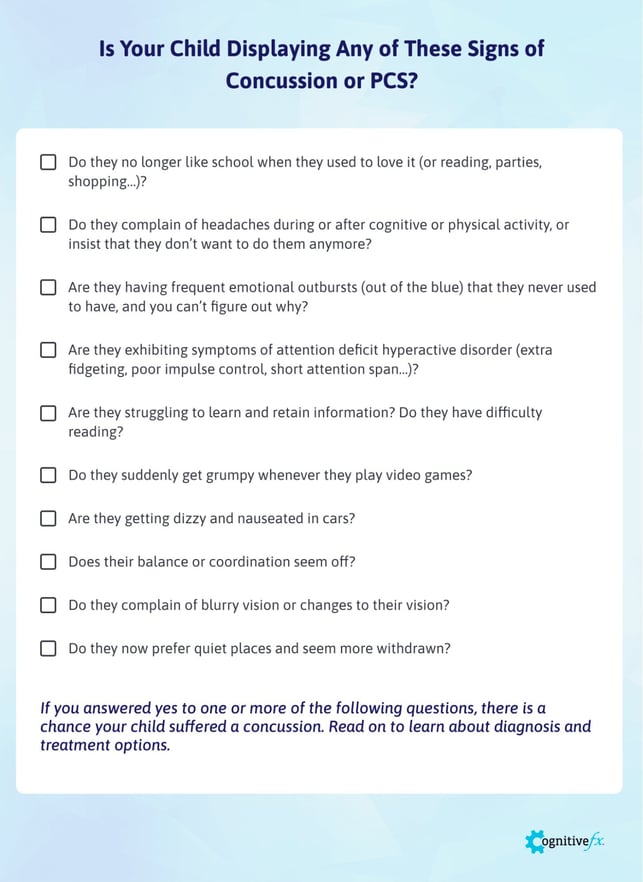
One of the biggest challenges in identifying post-concussion syndrome in children is that symptoms can look very different depending on age. Children often lack the vocabulary to describe what they're experiencing, and their symptoms may manifest as behavioral changes rather than physical complaints.
Symptoms in Toddlers and Preschoolers (Ages 2-5)
Young children can't tell you they have a headache or feel dizzy. Instead, watch for:
Symptoms in School-Age Children (Ages 6-12)
Elementary school children may be able to describe some symptoms but often don't recognize that what they're experiencing is abnormal. Look for:
Symptoms in Adolescents (Ages 13-18)
Teenagers may try to minimize symptoms to return to sports or social activities, or may not connect their symptoms to their injury. Watch for:

A 2025 study from Children's Hospital of Philadelphia found that nearly two-thirds of pediatric concussion patients report new sleep disturbances after injury, a rate higher than previously documented. Sleep disturbance was the second strongest predictor of prolonged recovery, behind only female sex. [DOI: 10.3389/frsle.2025.1528458]
Other frequently overlooked symptoms include:
Vision problems: Double vision, difficulty tracking text while reading, trouble focusing at different distances, eye fatigue. Research shows these symptoms often persist even when other symptoms improve and require specialized vision therapy.
Exercise intolerance: Symptoms that worsen with physical activity, elevated heart rate responses to minor exertion, or a sensation that the heart is "racing" inappropriately.
Cognitive fatigue: Mental exhaustion that comes on faster than expected, difficulty sustaining attention throughout the school day, needing frequent breaks.
Emotional regulation difficulties: Crying more easily than usual, getting frustrated quickly, emotional responses that seem out of proportion to situations.
|
Immediate or Early |
|
Early or Delayed |
|
||
|
||
|
|
|
|
|
|
|
||
|
||
|
|
|
|
||
|
|
|
|
||
|
|
|
|
||
|
||
|
|
|
|
||
|
||
|
||
|
|
|
|
||
Not every child who gets a concussion develops post-concussion syndrome. Research has identified several factors that increase risk:
Pre-injury factors:
Injury factors:
Post-injury factors:
Research consistently shows that adolescent girls experience longer concussion recovery times than boys of the same age. A 2025 study in the Journal of Head Trauma Rehabilitation found significant sex differences in blood biomarkers related to brain injury, suggesting biological factors may contribute to these differences. [DOI: 10.1097/HTR.0000000000001110]
Several theories explain this pattern:
Regardless of the cause, girls who sustain concussions should be monitored closely and parents should be prepared for potentially longer recovery timelines.
Go to the emergency department immediately if your child experiences:
Consult a specialist if your child:
Many pediatricians and even some neurologists don't specialize in post-concussion syndrome and may not be familiar with current evidence-based treatments. Look for:
Let's look at what the evidence actually tells us about recovery timelines:
Typical recovery (most children):
Post-concussion syndrome (10-30% of children):
Factors associated with faster recovery:
Factors associated with slower recovery:
The 2022 Amsterdam Consensus Statement revolutionized pediatric concussion management with several key updates:
Old approach (now outdated):
New evidence-based approach:
This represents a fundamental shift: prolonged rest can actually prolong recovery by deconditionining the brain and body, increasing anxiety, and disrupting the social connections children need.
Week 1 (Days 1-7):
Week 2 (Days 8-14):
Weeks 3-4 (Days 15-28):
Beyond 4 weeks:
For decades, the standard advice for concussion was complete rest until symptoms resolved. We now know this approach is not only ineffective for many children but can actually prolong recovery.
Research shows that:
The Amsterdam 2022 Consensus states clearly: "Gone are the days of complete physical and cognitive rest. 'Cocooning,' in which a patient is kept in a darkened environment with little stimulus, not only lacks benefit but may be harmful by slowing recovery."
Modern evidence-based treatment for pediatric PCS focuses on active rehabilitation. A 2024 study in Neuropsychological Rehabilitation found that multimodal intervention programs significantly improved symptoms in children with persistent post-concussion symptoms. [DOI: 10.1080/09602011.2024.2402564]
Aerobic Exercise Therapy
Sub-symptom threshold aerobic exercise has emerged as one of the most effective treatments for PCS. Research shows that prescribed aerobic exercise improves quality of life and reduces symptoms.
Key principles:
Vestibular Rehabilitation
For children with dizziness, balance problems, or motion sensitivity, vestibular therapy is crucial. This specialized physical therapy retrains the balance and spatial orientation systems.
A 2024 study found that adolescents who received vestibular rehabilitation showed similar benefits regardless of sex, with both males and females improving equally. [DOI: 10.1097/HTR.0000000000001113]
Vision Therapy
Given that over 60% of children with persistent symptoms have vision disorders, specialized vision assessment and therapy is often essential.
Vision therapy addresses:
Cognitive Rehabilitation
For children struggling with attention, memory, and thinking speed, cognitive therapy provides targeted exercises to rebuild these skills. This may include:
Cervical Spine Treatment
Neck dysfunction contributes to many PCS symptoms, particularly headaches and dizziness. Treatment may include:
Psychological Support
The emotional impact of prolonged symptoms shouldn't be underestimated. Effective treatment often includes:
At Cognitive FX, we take a comprehensive, multidisciplinary approach to treating children with post-concussion syndrome. Here's what makes our approach different:
Functional Brain Imaging (fNCI)
Unlike standard MRI or CT scans, which typically appear normal in PCS patients, our functional Neurocognitive Imaging (fNCI) scan shows us how different regions of your child's brain are actually functioning. This proprietary technology allows us to:
This imaging gives parents something they often haven't had: objective proof that something is wrong and a clear path forward.
EPIC Treatment Protocol
Our Enhanced Performance in Cognition (EPIC) treatment is an intensive, one-week program designed to jumpstart recovery. The treatment follows a cycle of preparation, activation, and recovery:
Therapies included may incorporate:
Treatment for Children
We treat children ages 8 and up (or at a third-grade reading level). Our approach is tailored for younger patients:
Treatment Outcomes
An independent peer-reviewed study found that 77% of patients treated at Cognitive FX showed statistically significant improvement in symptoms. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
If your child has been struggling with post-concussion symptoms, schedule a consultation with our team. We'll review their medical history and determine if they're eligible for treatment.

The old advice to keep children home from school until symptoms completely resolve is now considered harmful. Research shows that extended school absence:
The Amsterdam Consensus recommends returning to school within one to two days of injury, with appropriate accommodations. Missing school for more than a week is explicitly not recommended for most children.
Students should progress through these stages as tolerated, spending at least 24 hours at each stage before moving on:
Stage 1: Daily Activities at Home
Stage 2: School Activities at Home
Stage 3: Partial Return to School
Stage 4: Full Return with Accommodations
Stage 5: Full Return Without Accommodations
Academic accommodations for children with PCS may include:
Environmental modifications:
Schedule modifications:
Workload modifications:
Testing modifications:
Support services:
504 Plan: Provides accommodations within regular education. Appropriate for most students with PCS. Faster to implement and modify.
IEP (Individualized Education Program): Provides specialized instruction and related services. May be needed if PCS causes significant, long-term educational impact.
Most children with PCS will benefit from a 504 plan. Work with your school's 504 coordinator to develop appropriate accommodations.
When requesting accommodations, specific language helps. Examples:
"Due to post-concussion syndrome, [Child's Name] requires extended time (time and a half) on all tests and quizzes, to be administered in a quiet environment separate from the classroom."
"[Child's Name] is permitted to take rest breaks as needed, signaled to the teacher by [agreed-upon signal], with access to the nurse's office or other quiet space for breaks lasting 10-15 minutes."
"Homework assignments will be reduced by 50% during the accommodation period, with priority given to core concepts as identified by the teacher."
Effective communication with your child's teachers is essential. Consider:
Remember: teachers want to help but may not understand concussion. Brief education about PCS can go a long way.

Following the Amsterdam 2022 guidelines, young athletes should complete this graduated return-to-play protocol after being cleared for activity by a healthcare provider. Each step should take at least 24 hours, with return to the previous step if symptoms worsen.
Step 1: Symptom-Limited Activity
Step 2: Light Aerobic Exercise
Step 3: Sport-Specific Exercise
Step 4: Non-Contact Training Drills
Step 5: Full-Contact Practice
Step 6: Return to Competition
Critical rules:
The Amsterdam 2022 Consensus made several important updates to return-to-play protocols:
Previous guidance: Complete rest until symptom-free, then begin graduated protocol.
Current guidance: Brief rest (24-48 hours), then begin symptom-limited physical activity. The graduated protocol now begins earlier, with light activity permitted even while mild symptoms persist.
Why this matters: Emerging evidence shows that early, controlled physical activity may actually promote recovery rather than delay it. Athletes who remain completely sedentary may decondition and experience prolonged symptoms.
Once your child returns to sports, consider these evidence-based prevention strategies:

Sleep optimization:
Activity pacing:
Screen time management:
Nutrition and hydration:
Physical activity support:
Once your healthcare provider approves, gentle cognitive activities can support recovery:
Key principles:
Post-concussion syndrome takes an emotional toll on children and families. Support strategies include:
Validation: Acknowledge that symptoms are real and frustrating. Avoid phrases like "it's all in your head" or "just try harder."
Patience: Recovery can be slow. Celebrate small improvements rather than focusing on remaining limitations.
Hope: Remind your child that most children with PCS do get better with appropriate treatment.
Connection: Maintain social connections when possible, even if activities need to be modified.
Professional support: Don't hesitate to involve a mental health professional if anxiety, depression, or mood changes become significant.
Contact your healthcare provider if:

Most children recover from concussion within two to four weeks. Post-concussion syndrome is diagnosed when symptoms persist beyond four weeks. With appropriate treatment, most children with PCS show significant improvement within one to three months. Some children may require longer treatment periods, particularly if they have risk factors like previous concussions or pre-existing conditions.
Post-concussion syndrome does not typically cause permanent brain damage. The brain has remarkable capacity for healing, particularly in children. However, prolonged symptoms that go untreated can lead to secondary problems like depression, anxiety, academic difficulties, and social challenges. This is why early, appropriate treatment is important.
This is where professional evaluation becomes crucial. Symptoms of PCS can overlap with anxiety, depression, ADHD, learning disabilities, and other conditions. A comprehensive evaluation by a specialist can distinguish between these possibilities. Sometimes multiple conditions exist together and all need to be addressed.
A pediatric neurologist can be helpful in some cases, particularly to rule out other neurological conditions. However, many neurologists don't specialize in post-concussion syndrome and may not offer the multidisciplinary treatment most children need. Look for providers specifically experienced in PCS treatment rather than assuming any neurologist will be the right fit.
Current evidence does not support complete screen avoidance after concussion. Moderate screen use is generally acceptable, though some children may need to limit screens that worsen their symptoms. Pay attention to your child's individual response and adjust accordingly. Complete isolation from screens may increase anxiety and social isolation without providing benefit.
Children should complete a graduated return-to-play protocol and receive medical clearance before returning to contact sports. This process takes a minimum of one week after symptoms resolve but often takes longer. Never return a child to contact sports on the same day as a concussion, regardless of how minor it seems.
If your child has had symptoms for more than four weeks without improvement, "waiting" is not a treatment plan. Seek evaluation from a specialist with expertise in post-concussion syndrome. Active rehabilitation, not passive waiting, is now the evidence-based standard of care.
Medications may help manage specific symptoms but don't treat the underlying dysfunction. Be cautious about:
Discuss any medications carefully with a provider familiar with pediatric PCS.
Signs of improvement may include:
Some options to explore:
Even if intensive treatment isn't immediately accessible, working with your primary care provider to implement active rehabilitation principles can help.

If your child has been struggling with symptoms following a concussion, you don't have to accept that this is just how things will be. Post-concussion syndrome is real, it's treatable, and most children can make meaningful recovery with the right approach.
The first step is getting proper evaluation from providers who understand PCS. Whether that's at Cognitive FX or another specialized clinic, the key is finding healthcare providers who offer:
Ready to get answers about your child's symptoms?
Schedule a free consultation with the Cognitive FX team. We'll review your child's medical history and determine if they're eligible for treatment at our clinic.
95% of our patients show statistically verified restoration of brain function after treatment. Your child deserves to feel like themselves again.
{{cta('124586502405')}}
References and citations are available upon request. This article incorporates current research from PubMed and guidelines from the 2022 Amsterdam Consensus Statement on Concussion in Sport.
Dr. Alina Fong, PhD, is a Clinical Neuropsychologist and co-founder of Cognitive FX. She holds a doctorate in Clinical Neuropsychology and has dedicated her career to developing evidence-based treatment protocols for brain injury patients.
Related Articles:

Dr. Lynn Gaufin graduated from the University of Utah and then attended medical school at Cornell University in New York City. After medical school he join the Army and was a surgeon in the military before finishing his Neurological Residency at University of California Los Angeles. Dr. Gaufin specializes in cervical and lumbar spine surgery, brain tumors, brain hemorrhages, and treatment of traumatic brain injuries. Dr. Gaufin is one of the emergency trauma neurosurgeons on call at Utah Valley Hospital. Before he began his practice in Utah he saw a significant amount of traumatic brain injuries during his career in the Army and his residency in Los Angeles. As a surgeon who treats individuals who suffer from mild to severe traumatic brain injuries he recognized a problem in the post operative rehabilitation. Individuals who suffered severe trauma would be admitted into speciality facilities where they would receive months of care. But patients who had a more mild trauma would be released and would largely be on their own when it came to restoring their cognitive function. That problem is what lead Dr. Gaufin to team up with Dr. Fong and Dr. Allen in the creation of Cognitive FX. Cognitive FX was able to take the research that Dr. Fong and Dr. Allen started in their Phd programs and bring it into the clinical environment.



You stand up from the couch and your heart takes off like you just sprinted across a parking lot. Your vision narrows. Your legs feel heavy and strange. You grab the counter and wait for it to pass.

Brain injury recovery is hard. The severity of your injury, which parts of your brain were affected, and how they were affected, all factor into things such as how much you can recover and how long...

The clatter of dishes. A child laughing in the next room. The hum of an air conditioner. For most people, these are background sounds their brain filters out automatically. But after a concussion,...

If you've searched "is Lyme brain fog permanent" or "will I ever think clearly again," you're not alone. And more importantly, you deserve a real answer based on actual science, not empty...
Published peer-reviewed research shows that Cognitive FX treatment leads to meaningful symptom reduction in post-concussion symptoms for 77% of study participants. Cognitive FX is the only PCS clinic with third-party validated treatment outcomes.
READ FULL STUDY