Head injuries vary wildly in severity. You could suffer anything from debilitating brain damage to a few days of feeling “off” before returning to normal. You might suffer a moderate traumatic brain injury and feel no lasting effects, or suffer from persistent symptoms after “just” a mild TBI.
Given the wide range of symptoms and outcomes, head injury treatment is not always easy. Sadly, this reality makes the journey to recovery an arduous process for many patients.
Patients with no visible structural damage on CT or MRI scans can be met with skepticism when they try to get help for their symptoms. Many of our patients have told us stories about providers who either said, “There’s nothing we can do to help you,” or, “You’re just imagining it; you’re just stressed.”
And patients with visible damage have their own hurdles to overcome. It’s hard to know when you’re “as good as you’re going to be” or if there’s another treatment option that could help your recovery. And that recovery can take many years.
At our clinic, Cognitive FX, we treat patients who are suffering from long-term symptoms after their brain injury. While the majority of our patients have post-concussion syndrome, we’ve treated patients with lingering symptoms from moderate and severe TBI, hypoxia, carbon monoxide poisoning, "chemo brain", bacterial and viral encephalitis, COVID-19, transient ischemic attack, and other sources of acquired brain injury.
In this article, we’ll look at the diagnosis and treatment process for mild, moderate, and severe traumatic brain injury:
We’ve also included some information at the end of the article explaining what a head injury is, what types of head injury you can have, and how doctors determine head injury severity. You can skip down to those sections if you want to learn more about brain injury terminology before reading about symptoms, diagnosis, and treatment options.
If you’re experiencing symptoms that won’t resolve after a concussion, you’re not alone. And you’re not crazy. On average, our patients’ symptoms improve by 60% after just one week of treatment at our center specializing in neuroplasticity-based therapy. To see if you are eligible for treatment, sign up for a consultation. (If you’re suffering from a COVID-related brain injury, please visit this form instead.)
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
What Are the Symptoms of a Head Injury?

Traumatic brain injuries have a wide range of physical, cognitive, visual, vestibular, autonomic, and psychological symptoms. Some signs appear immediately after the traumatic event, while others may not develop until a few days or weeks later.
Here are a few of the common symptoms that a mild traumatic brain injury (concussion) can cause:
For a more comprehensive discussion, see our article about the symptoms of a concussion.
Moderate to severe traumatic brain injuries can include any of the symptoms described above, but often affect the injured person more severely or for a longer period of time. This includes, for example, persistent or severe headaches that don’t go away and/or repeated vomiting and nausea even days after the injury. In addition, these injuries can also cause:
Physical symptoms:
- Loss of consciousness lasting from several minutes to hours
- Convulsions or seizures
- Dilation of one or both pupils of the eyes
- Clear fluids draining from the nose or ears
- Inability to awaken from sleep
- Weakness or numbness in fingers and toes
- Loss of coordination
Cognitive or mental symptoms:
- Profound confusion
- Agitation, aggression, or other unusual behavior
- Slurred speech
- Coma and other disorders of consciousness
When to See a Doctor

Not all head injuries need a trip to ER, but even seemingly mild injuries can have serious consequences if not treated promptly. Sometimes, it can be difficult to decide whether to seek medical care or not, but if you (or a family member) have any of these symptoms or situations, go to the Emergency Room (ER) or call 911 immediately:
- You are unconscious or lack full consciousness for a long time.
- You have clear fluid running from the ears or nose.
- You have bleeding from the ears.
- You’re showing signs of skull damage or a penetrating head injury.
- Your injury happened at high speed.
- You had a previous brain surgery.
- You are taking medication that may cause bleeding problems, like anticoagulants.
Continue to monitor symptoms for the first 48 hours. You may still need to go to the hospital if you develop any of the following:
- Loss of feeling in parts of the body
- Problems with balancing or walking
- General weakness
- Changes in eyesight
- Seizures
- Problems with memory of events before or after the injury
- A headache that won't go away
- Repeated vomiting
- Irritability or altered behavior
How Is a Head Injury Diagnosed?

In many cases, the full extent of the problem may not be immediately obvious after the head trauma. This is particularly true with closed injuries, which we can’t see with the unaided eye. That’s why we recommend that you seek medical attention to get a comprehensive evaluation.
Typically, doctors start with a quick examination of the entire body, including cardiac and pulmonary function. If they suspect a severe head injury, they’ll also test the ability of the pupils to become smaller with a bright light. In patients with swelling in the brain or large lesions, one or both of the pupils will remain wide even with a light.
At this stage, it’s also common to use the Glasgow Coma Scale (GCS) to assess the patient’s:
- Ability to speak, including whether they can speak normally, speak in a way that doesn’t make much sense, or can’t speak at all.
- Ability to open their eyes, including whether they can open eyes spontaneously, need to be asked, or can’t open eyes.
- Ability to move, ranging from moving easily, moving with visible pain, or not moving.
Healthcare providers rate the responses in each category and then calculate the overall score. Lower scores indicate more severe injury. A score of thirteen or higher indicates a mild TBI, between twelve and nine indicates a moderate TBI, and below eight indicates a severe TBI.
The duration of loss of consciousness after the injury and post-traumatic amnesia can also be used to assess the severity of the brain injury. Severe cases are more likely to cause extended periods of unconsciousness and post-traumatic amnesia, whereas patients with a mild head injury may never show these symptoms at all.
| Severity |
GCS |
Loss of consciousness |
Post-traumatic amnesia |
| Mild |
13-15 |
A few minutes and only in about 10% of patients |
A few minutes |
| Moderate |
9-12 |
15 minutes - 6 hours |
Up to 24 hours |
| Severe |
< 8 |
More than 6 hours |
More than 24 hours |
| Very severe |
< 8 |
More than 48 hours |
More than 7 days |
Following this initial examination, doctors may require a series of medical tests, including:
Imaging Tests
Healthcare providers who suspect a TBI may order a brain scan. Brain scans are useful in some patients to evaluate the extent of the injury and determine if surgery is needed to repair any damage to the brain, such as a skull fracture or internal bleeding.
These brain scans may include:
- Computerized tomography (CT). A CT scan takes X-rays from multiple angles to create a 3D picture of the brain and can show a skull fracture or any brain bruising (contusion), hematoma, hemorrhage (bleeding), or swelling. It’s mostly used to assess people with suspected moderate or severe TBI. It’s primarily useful in viewing harder structures (bone). We’ve discussed in another post why CT scans don’t really show concussions.
- Magnetic resonance imaging (MRI). MRI uses magnets and radio waves to produce more detailed images than CT scans, particularly of soft tissues. If needed, it can be used after the initial assessment to pick up subtle changes in the brain that a CT might have missed. A structural MRI can’t see the dysfunction caused by concussions either.
- Functional neurocognitive imaging (fNCI): This scan — only available at Cognitive FX — is a type of functional MRI (versus a structural one). It measures the amount of blood flow to different areas of the brain as the patient performs a series of cognitive tasks. By determining how far from the norm your brain’s response to stimulation is, we can identify regions that are malfunctioning due to dysfunctional neurovascular coupling.
Monitoring Intracranial Pressure
In moderate to severe TBI, tissue swelling may increase the pressure inside the skull and cause additional damage to brain tissue. To detect these cases, doctors insert a probe through the skull to monitor pressure. If needed, the device can also be used to drain excess fluid and relieve excess pressure in the brain. While the device is in place, patients are usually given medication to alleviate pain and stay comfortable. When the swelling has gone down, the device can be removed.
Neurological and Cognitive Examination
For patients with less severe injuries, doctors may also perform a series of neurological and cognitive exams to determine how much the brain has been affected. Your doctor may test your strength, reflexes, coordination and balance, as well as your cognitive skills, such as recall ability and concentration.
What Can You Expect from Head Injury Treatment?

Once you’ve gotten first aid, take the first 48 hours after a mild traumatic brain injury to rest and allow your brain to recover. That includes both mental and physical rest, such as limiting work on a computer and avoiding sports. After this period, you can gradually increase daily activities (see our sister clinic’s concussion recovery protocol for more guidance). During the first few days, avoid activities (such as sports) that have a high risk of causing a further injury until you are further into recovery.
Depending on the injury, your doctor may recommend going back to school or work with shorter days or a reduced workload for a period of time. You may also benefit from different therapies, including vision therapy, physical therapy, cognitive therapy, and others.
During the recovery period, it’s common for patients to complain of headaches. To manage this pain, it’s safe to take pain-killers such as acetaminophen (Tylenol), but it’s better to avoid ibuprofen (Advil, Motrin IB) and aspirin since these medications may increase the risk of internal bleeding. If you experience a constant headache that continues to worsen, seek medical advice.
Moderate and severe traumatic brain injuries usually need more intense treatment. Especially for patients who suffered a severe injury, the initial focus may be to prevent death, or at least to ensure proper breathing, control blood pressure, and prevent further brain damage.
Surgery might be part of emergency care to limit damage to the brain. That could include removing blood clots or controlling bleeding in the brain; repairing skull fractures or cleaning debris from the area affected by the injury; and relieving pressure inside the skull caused by swelling or bleeding.
After a period in hospital, many patients with severe brain injuries need rehabilitation with a team of multidisciplinary healthcare providers, including neurologists and psychologists, as well as physical, occupational, speech, and cognitive therapists, to name just a few. Most of these initial therapy providers will focus on returning the skills needed for daily living activities, such as tying shoes, brushing teeth, and holding a basic conversation. As patients progress, they will need more challenging therapies to continue their recovery.
What Can You Expect from Treatment in the Long Term?

It’s virtually impossible to predict how long it will take to recover from a head injury. As a general rule, the more severe the injury, the less likely you are to experience a full recovery. Patients with moderate injuries are more likely to regain consciousness quickly and make a full recovery. In contrast, severe injuries progress more slowly, and patients may remain in a state of impaired consciousness for a longer period. However, this is not always the case, and even patients with a severe injury may be able to improve with the right treatment.
On the other end of the scale, most patients with a mild brain injury don’t experience such extreme situations. The majority make a full recovery within a couple of weeks after their injury. However, not all patients follow this pattern. Up to 30% experience long-term symptoms which may last for months or even years after the concussion. This condition is called post-concussion syndrome (PCS).
PCS can be extremely disruptive. Often, PCS patients restructure their lives to avoid situations that may cause their symptoms to worsen. This condition can seriously impact quality of life, interfere with personal and work activities, and greatly increase the risk of depression and other mental health problems.
Further reading: Brain injury recovery stories from five survivors
Treatment for Persistent Head Injury Symptoms at Cognitive FX

At Cognitive FX, we specialize in treating patients with post-concussion syndrome. We also treat patients with lingering symptoms from moderate and severe TBIs (though the extent of improvement may not be as good due to injury severity), as well as certain other types of brain injuries. These different types of head injuries have one thing in common: brain dysfunction caused by changes in neurovascular coupling (NVC).
Neurovascular coupling refers to the connections between brain cells and the surrounding blood vessels. When the brain needs to perform a particular task, it relies on these blood vessels to transport precise amounts of oxygen and nutrients to the right areas of the brain at the right time.
However, this mechanism can be disrupted by a head injury. Vascular and axonal shearing and pulling can disrupt blood circulation and deprive some areas of the brain of the amount of oxygen needed to operate normally. The brain continues to try to deliver supplies, attempting different routes to reach the final destination, but this is typically a less efficient method. Ultimately, some areas can’t get enough blood and become hypoactive. Many of the signs and symptoms PCS patients experience are directly or indirectly caused by this disruption.
For most patients, symptoms will continue until healthy neurovascular coupling is restored. Therefore, our main focus during treatment is to restore this mechanism using a combination of physical and cognitive activities. We also work extensively to rehabilitate the autonomic nervous system, which can be disrupted and contribute to symptoms after a brain injury. Most patients undergo treatment with us for one or more weeks.

Treatment begins with an fNCI scan to determine where and to what extent the brain injury caused neurovascular coupling dysfunction. In addition, our team of therapists evaluate the visual, vestibular, and autonomic systems (which can't be imaged in the fNCI but can cause major brain injury symptoms). Our therapists then use this information to design a treatment plan customized to your brain’s specific needs.
Some of the therapies we use during treatment include:
Patients undergo a second fNCl to re-evaluate brain function compared with before they started treatment. While we can’t promise a full recovery, many of our patients find significant relief after therapy at our clinic, even those with moderate and severe brain injuries. 90% of our patients experience symptom improvement in the first week, with an average symptom improvement of 60%. To learn more about getting treatment, schedule a consultation with our team. (If you’re suffering from a COVID-related brain injury, please visit this form instead.)
To learn more about what treatment is like from a patient’s perspective, read some of our patient stories:
Understanding Brain Injury Terminology
In this section, we cover some introductory information about brain injuries, including what qualifies as a head injury, what the types of head injuries are, and how doctors determine head injury severity.
What Is a Head Injury?
A head injury is a broad term describing injuries that cause damage to the scalp, skull, brain, blood vessels, and any other underlying tissue in the head. Although not strictly the same, the names “head injury” and “brain injury” are often used interchangeably in the medical literature.
Head injuries are one of the most common causes of death and disability in adults. These injuries vary greatly and can be as mild as a bump, a bruise, or a cut on the head; or as severe as open wounds, fractured skull bones, or damage caused by internal bleeding.
The two most common causes of head injury are falls and road traffic accidents, including collisions between two or more cars (especially if not wearing a seatbelt), pedestrians, cyclists, or motorcyclists. Other common causes include injuries during sports, suicide attempts, domestic abuse, and military combat.
Types of Head Injury
There are various ways to classify a head injury. The classification is important for diagnosis and treatment, as well as when deciding whether the patient should receive neurorehabilitation.
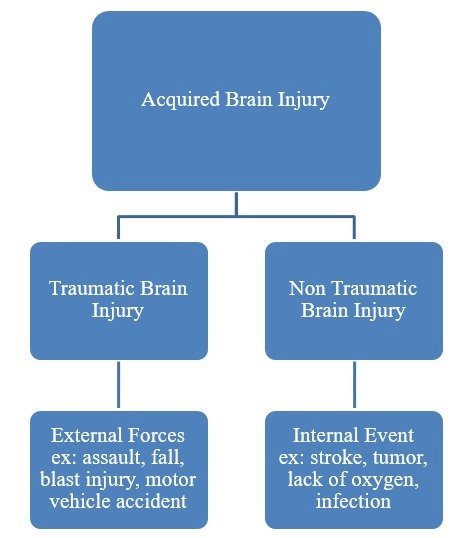
Acquired head injuries can be classed as:
- Closed versus open: In a closed head injury, damage to the brain occurs as a consequence of a blow to the head or a sudden stop after moving at high speed. This causes the brain to move back and forth or side to side, crashing the soft tissue against the skull. Injuries after a motor vehicle crash, for example, are typically closed injuries. Open injuries, on the other hand, occur from the impact of a bullet, knife, or another object that forces skin, bone, or fragments from the object into the brain.
- Primary versus secondary: Primary injuries occur at the time of injury, whereas secondary injuries occur after the initial injury, usually within a few days. Secondary injuries are often caused by lack of oxygen, which may be the result of conditions such as sustained low blood pressure or increased intracranial pressure (often from swelling or intracranial hematoma) inside the brain.
- Focal versus diffuse: Focal injuries are localized in a small area and are commonly associated with events where the head strikes or is struck by an object. In contrast, diffuse injuries occur over a more widespread area. They are more often found in acceleration/deceleration injuries, such as from a car crash. It is common for both to occur as a result of the same incident; many brain injuries have aspects of both focal and diffuse injury.
Degree of Severity of the Injury
A traumatic brain injury is caused by a blow, bump, or jolt to the head. It could involve the head suddenly or violently hitting an object, for example, or an object piercing the skull and entering the brain. In other words, a traumatic brain injury can stem from any outside impact and may result in brain dysfunction.
Note: Some brain injuries are classified as non-traumatic. In this case, the damage doesn’t result from an external source. Instead it’s caused by non-violent factors, such as an illness, a genetic condition, or degenerative disease (dementia, and so on).
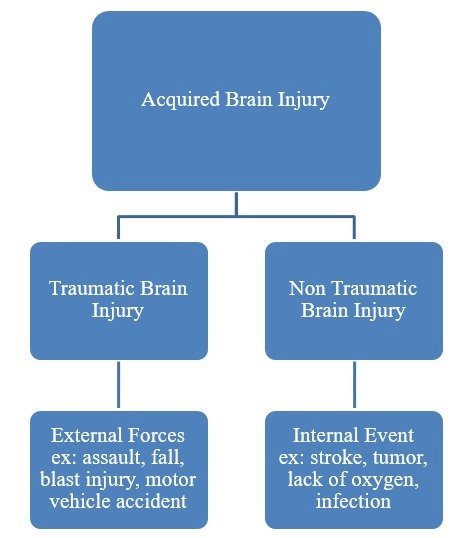 Image source: Brain Injury Alliance Colorado
Image source: Brain Injury Alliance Colorado
These conditions and injuries are still serious and traumatic for the patient even though the scientific labeling is “non-traumatic.” Both traumatic and non-traumatic injuries can have long-term symptoms that affect the patient for years. Most of the patients that we treat have dealt with lingering symptoms caused by a traumatic brain injury, but we also treat certain types of non-traumatic brain injuries.
Traumatic head injuries are classified as mild, moderate, or severe traumatic brain injuries.
Commonly called concussions, mild traumatic brain injuries (mTBI) are the most common type of brain injury. About three out of every four TBIs are concussions. This head injury occurs when the brain is shaken hard enough to bounce against the skull. You don't have to be hit directly in the head to get a concussion; an impact elsewhere on the body can create enough force to reach the brain. Contrary to popular belief, you don’t have to lose consciousness to have a concussion. In fact, only 1 in 10 patients with an mTBI experience loss of consciousness, and only for a brief period at that. Just because it’s classed as mild, it doesn’t mean it’s a minor head injury. Concussions can result in serious long-term symptoms. This condition is known as post-concussion syndrome.
Moderate traumatic brain injuries are typically associated with loss of consciousness between 15 minutes and six hours, or a period of post-traumatic amnesia (memory loss) of up to 24 hours. Patients with moderate TBIs often feel confused for a few days after the injury and may suffer from a number of long-term symptoms, including tiredness, headaches, cognitive issues, and irritability. For the majority of people, these residual symptoms gradually improve, although it may take a few months.
Severe traumatic brain injuries involve loss of consciousness for six hours or more or a post-traumatic amnesia of 24 hours or more. In the most extreme cases, patients lose consciousness for 48 hours or more, or have a period of post-traumatic amnesia of seven days or more. The longer the period they stay unconscious or experience post-traumatic amnesia after the injury, the poorer the outcome. Many of these patients need hospitalization and rehabilitation for months after the injury, and may suffer long-term impairments.
If you’re experiencing symptoms that won’t resolve after a concussion, you’re not alone. And you’re not crazy. To see if you are eligible for treatment, sign up for a consultation. (If you’re suffering from a COVID-related brain injury, please visit this form instead.)